Storing your medications wrong isn’t just a small mistake-it can make them useless or even dangerous. Think about it: if your insulin freezes, your asthma inhaler gets too hot, or your antibiotics sit in a humid bathroom, they might not work when you need them most. This isn’t speculation. The FDA found that 78% of pharmaceutical recalls in 2022 happened because of temperature or humidity problems during storage. That’s not a glitch. It’s a systemic risk-and it’s happening in homes, clinics, and pharmacies every day.
Why Temperature and Humidity Matter
Medications aren’t like canned food. They’re complex chemical formulas, many built around proteins, hormones, or fragile molecules that break down easily. Heat, moisture, and even sudden temperature swings can trigger chemical reactions that reduce potency or create harmful byproducts. A study from Baystate Health showed that exposure outside the 59°F-77°F range reduced effectiveness by 23% to 37%, especially for drugs like birth control, chemotherapy agents, and anti-seizure medications. One pill that’s lost half its strength might not cause immediate harm-but over time, it can lead to treatment failure, hospitalization, or worse.Humidity is just as critical. Moisture causes tablets to stick together, capsules to soften, and liquid medications to grow mold. The World Health Organization says 15-20% of global medication waste comes from poor storage conditions. That’s $35 billion lost every year-not because the drugs were expired, but because they were stored like groceries in a hot kitchen.
The Official Storage Zones
You don’t guess at storage conditions. You follow science-backed categories defined by the US Pharmacopeia (USP Chapter 1079) and the FDA:- Room Temperature: 68°F-77°F (20°C-25°C). This is where most pills, capsules, and creams go. Brief excursions to 59°F-86°F are allowed, but don’t make it a habit.
- Controlled Cold: 36°F-46°F (2°C-8°C). This is for insulin, some vaccines, biologics, and injectables. Never freeze unless the label says so.
- Frozen: -13°F to 14°F (-25°C to -10°C). Used for certain long-term storage of plasma or specialty drugs.
- Deep Frozen: Below -4°F (-20°C). Rare, but required for some gene therapies and rare disease treatments.
And humidity? Aim for 50% relative humidity. Too dry, and some liquids evaporate. Too damp, and tablets crumble or pills degrade. The WHO and FDA both say: cool and dry. That’s the mantra.
Where NOT to Store Medications
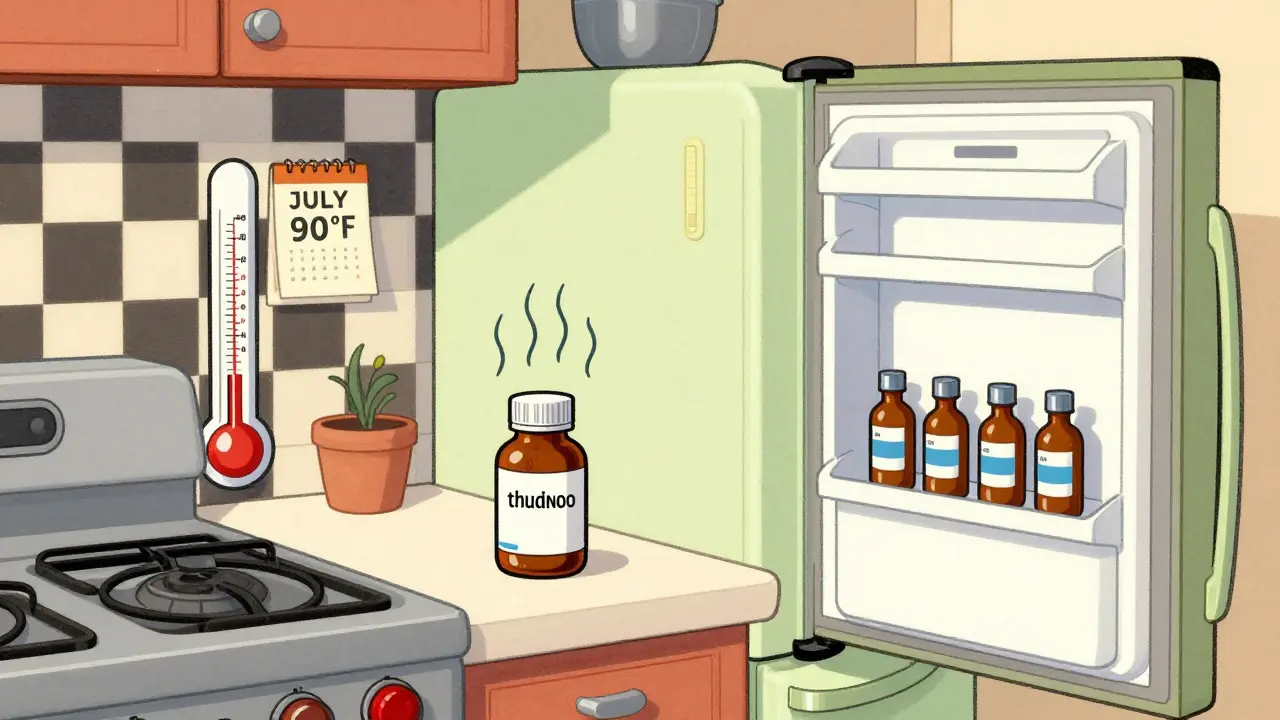
Your bathroom cabinet? A bad idea. Showers create steam. Toilets release moisture. The temperature swings from cold in the morning to hot after a long shower. A 2022 study by Helmer Scientific found that bathroom storage units had humidity levels hitting 75%+-far above safe limits.What about the kitchen? Tempting, because it’s convenient. But near the stove? The oven? The dishwasher? Heat rises. Even on a cool day, the air above your stove can hit 90°F. That’s enough to ruin your thyroid medication or diabetes pills.
Windowsills? Don’t even think about it. Sunlight doesn’t just warm things up-it triggers photo-degradation. Some medications, like tetracycline or nitroglycerin, can turn toxic when exposed to UV light. And don’t store them in your car. In Calgary, even in January, parked cars can hit 70°F inside. In July? They hit 120°F. That’s not storage-that’s a chemical experiment.
How to Monitor Your Storage
You can’t manage what you don’t measure. A simple thermometer from the hardware store won’t cut it. You need a data logging device (DDL) that:- Uses a buffered probe (not just a bare sensor)
- Records temperature every 30 minutes or less
- Has an alarm for out-of-range conditions
- Shows minimum and maximum temperatures
- Has a current calibration certificate
These aren’t luxury items. They’re required by the CDC’s Vaccine Storage and Handling Toolkit. Even pharmacies without formal protocols should use them. Dickson Data’s analysis of 15,000 pharmacy logs found that 18.7% of locations had at least one temperature spike above 77°F during summer months-with each incident lasting an average of 4.2 hours. That’s long enough to damage a week’s supply of medication.
For home use, you can get reliable DDLs for under $50. Place one inside your medicine cabinet, fridge, or storage box. Check it weekly. If the max temp hits 85°F, move your meds. Don’t wait for a warning label to fade or a pill to look funny.
Refrigerator Mistakes (And How to Avoid Them)
Storing insulin or vaccines in the fridge seems smart-until you realize that fridge doors are the warmest spots. The CDC says temperature swings near the door can be 5°F higher than the center. That’s enough to degrade sensitive drugs.Here’s what to do:
- Store medications in the center of the fridge, not on the door.
- Avoid placing them against the back wall-where condensation builds up.
- Never put them in the crisper drawer. Too humid.
- Use a dedicated, labeled bin. No sharing with leftovers.
Also, check your fridge’s actual temperature. Many home fridges run at 40°F or higher. That’s too warm for controlled cold storage. Use a separate thermometer inside the fridge. If it’s above 46°F, adjust the setting or get a small medical-grade refrigerator.
What Happens When You Skip the Rules?
It’s not just about wasted pills. Improper storage leads to real health consequences. The Joint Commission found that 17% of medication errors in hospitals trace back to storage issues. In one case, a patient on chemotherapy received a degraded dose because the vial had been left in a car for three hours. The drug lost potency. The treatment failed. The patient had to restart the entire cycle.And it’s not just hospitals. In developing countries, the WHO estimates 50% of vaccines are lost due to temperature failures. That’s millions of children unprotected. Even in wealthy countries, pharmacies lose $127,000 per rejected shipment when drugs arrive warm. That cost gets passed down-to you.
What’s Changing in 2025?
The rules are getting tighter. In January 2024, the FDA announced a new requirement: all healthcare facilities must use real-time remote monitoring for temperature-sensitive drugs by December 2025. No more manual logs. No more hoping the fridge stayed cold overnight.USP is also updating Chapter 1079 to tighten humidity controls, proposing a strict range of 45% ± 5%. And new tech is emerging fast:
- Blockchain monitoring: Used by Pfizer and Moderna-every temperature reading is tamper-proof and timestamped.
- AI predictive alerts: Systems that learn your fridge’s patterns and warn you before a spike happens.
- Phase-change materials: Special packs that keep drugs at 2-8°C for up to 120 hours during transport-no electricity needed.
By 2027, 85% of pharmacies will use IoT-based monitoring. That’s up from 42% in 2023. The cost of non-compliance is rising faster than the cost of upgrading.
What You Can Do Today
You don’t need to wait for regulations to catch up. Here’s your action plan:- Check your meds. Look at the label. Does it say “store at room temperature,” “refrigerate,” or “do not freeze”? If it doesn’t say, call your pharmacist.
- Find a better spot. Move meds away from bathrooms, kitchens, windows, and cars. A closet on an interior wall is ideal.
- Buy a data logger. Get one for your medicine cabinet and fridge. Set the alarm to notify you if it goes out of range.
- Train your household. If someone else picks up your prescriptions, make sure they know where to store them.
- Dispose of damaged meds properly. If a pill is discolored, sticky, or smells odd, don’t take it. Return it to your pharmacy for safe disposal.
Medications are life-saving tools. But they’re only as good as the care they’re given. A simple $50 monitor, a change of shelf, and five minutes of attention can mean the difference between a treatment that works-and one that doesn’t.
Can I store all my medications in the fridge?
No. Only store medications in the fridge if the label specifically says to. Many pills, like antibiotics or pain relievers, can break down in cold, damp environments. Refrigeration is only needed for insulin, some vaccines, and certain biologics. Storing everything in the fridge can cause condensation, which damages packaging and reduces shelf life.
What happens if my insulin freezes?
Frozen insulin loses its effectiveness and can become dangerous. Freezing damages the protein structure, making it unable to regulate blood sugar properly. Even if it looks normal, don’t use it. Throw it out and get a new vial. Always check the appearance-frozen insulin may look cloudy or have clumps.
Is a digital thermometer enough to monitor my medicine cabinet?
No. A regular digital thermometer only shows the current temperature. You need a data logger that records highs and lows over time. Door openings, power outages, or hot days can cause spikes you won’t notice unless you have a log. The CDC and FDA require logging devices with calibration certificates for compliance-not just basic thermometers.
How often should I check my medication storage conditions?
Check your data logger at least once a week. If you live in a place with extreme seasons-like Calgary, where winters are harsh and summers can be hot-check more often. After any power outage, travel, or move, verify the temperature hasn’t spiked. Don’t wait for a pill to look bad-act before it’s too late.
Are there affordable monitoring devices for home use?
Yes. Reliable data loggers start around $40-$60. Brands like Dickson Data and American Thermal offer models designed for home pharmacies. Look for one with a buffered probe, alarm function, and the ability to download data via USB or Bluetooth. Some even connect to your phone. It’s a small investment compared to the cost of replacing spoiled meds or risking your health.
Can I trust the pharmacy’s storage conditions?
Most do, but not all. A 2023 study found that 73% of pharmacies had inadequate monitoring equipment, and 41% used probes that gave false readings during door openings. Ask your pharmacist if they use continuous monitoring systems. If they can’t show you temperature logs or don’t know the answer, consider switching to a pharmacy that follows FDA and USP standards.
What should I do with expired or damaged medications?
Never flush or throw them in the trash. Take them to a pharmacy with a take-back program. Many pharmacies offer free disposal bins for expired, damaged, or unwanted meds. This prevents environmental contamination and stops someone else from accidentally using a degraded drug. If no take-back program is available, mix pills with coffee grounds or cat litter, seal them in a container, and throw them in the trash-but still avoid flushing.






Katelyn Slack
5 January 2026 - 15:11 PM
i had no idea my bathroom cabinet was basically a science experiment for my pills. i just put them there because it was convenient. guess i’m moving them to the closet now.
also, typo: i meant ‘meh’ not ‘me’ but you get it.
Melanie Clark
6 January 2026 - 04:36 AM
78% of recalls because of storage? That’s not negligence thats a coverup. The pharma giants want you to keep buying new pills because they know your fridge is a death trap. They dont want you to know that a $50 logger can save you $2000 in wasted meds. This is controlled chaos. They profit from your ignorance. And the FDA? They’re in bed with them. Wake up.
also the humidity thing? They’ve been hiding this since 2012. I read it in a forum. Its real.
Harshit Kansal
7 January 2026 - 05:19 AM
bro this is actually super useful. i used to keep my insulin next to the microwave. now i know why it always felt weird. gonna grab one of those loggers this weekend. thanks for the heads up.
also no emojis because im not a robot.
Brian Anaz
7 January 2026 - 09:23 AM
if you cant afford to store your meds right then you shouldnt be taking them. this country is full of people who think medicine is a freebie. you want your pills to work? Stop being lazy. Buy a thermometer. Move your stuff. Simple. No excuses.
and no i dont care if you live in a studio apartment. you have a closet. use it.
Vinayak Naik
8 January 2026 - 05:45 AM
yo i work in a pharmacy in Bangalore and let me tell you - the heat here is brutal. we had a whole shipment of antibiotics turn to mush last monsoon. it smelled like wet socks and regret. we lost 12k in one week.
now we keep everything in sealed bins with silica packs. no more ‘eh, it’s fine’. the humidity here hits 90% and your pills turn into paste. trust me, this ain’t just a US thing. global problem.
also, data loggers? yes. cheap ones work fine. i got mine off Amazon for $38. no cap.
Saylor Frye
8 January 2026 - 09:25 AM
how quaint. another article telling people how to live their lives. next you’ll be telling me to alphabetize my spice rack. the fact that this is even a conversation shows how absurd our healthcare system has become. you need a $50 gadget to know if your aspirin is still alive?
pathetic. But hey, at least we’re all doing our part to keep Big Pharma’s quarterly reports glowing.
Molly McLane
9 January 2026 - 16:50 PM
thank you for writing this. i’m a caregiver for my mom and i had no idea about fridge door temps. we’ve been storing her insulin there for years.
i just ordered a data logger and labeled a bin in the center shelf. also shared this with my sister who takes thyroid meds - she was keeping them above the stove. oops.
we’re all learning. this is the kind of info that saves lives. really appreciate the clarity.
Wesley Pereira
10 January 2026 - 22:15 PM
so let me get this straight - we’re now at the point where you need a PhD in pharmacology just to store your ibuprofen? congrats, we’ve turned basic human care into a compliance checklist.
also, i’ve got a 2017 digital thermometer that says 72°F. why do i need a ‘buffered probe’? because the FDA says so? cool. i’ll just keep doing what i’ve been doing. my pills haven’t killed me yet.
ps: i’m not being sarcastic. i’m just tired.
Isaac Jules
11 January 2026 - 21:14 PM
you’re all idiots. if your meds are breaking down because of a 5-degree swing then they were junk to begin with. stop blaming storage and start blaming the manufacturers who make weak-ass formulations. this is a scam to sell you more gadgets. your insulin isn’t fragile - your trust in pharma is.
and that $50 logger? it’s probably made in China with counterfeit sensors. you’re being played.
Pavan Vora
12 January 2026 - 06:28 AM
Dear all, I am from India, and I must say, this topic is so critical, especially here, where power cuts are frequent, and refrigerators are often unreliable. I have seen people store insulin in clay pots to keep it cool - yes, clay pots! It works surprisingly well, as evaporation cools the surface. But humidity? Oh, my goodness, we have a 90% humidity level during monsoon - it turns tablets into mush. I recommend using airtight containers with silica gel packs - available at any pharmacy here for ₹20. Please, do not underestimate the power of dryness. Thank you for sharing this - it’s a lifeline for many.