Drinking alcohol with diabetes isn't just about calories or liver health-it can land you in the emergency room. If you're on insulin, sulfonylureas, or even metformin, alcohol can trigger a silent, life-threatening drop in blood sugar that hits hours after you've finished your drink. This isn't theoretical. It happens every night in homes, bars, and parties across the country-and most people don’t see it coming until it’s too late.
Why Alcohol Drops Your Blood Sugar So Fast
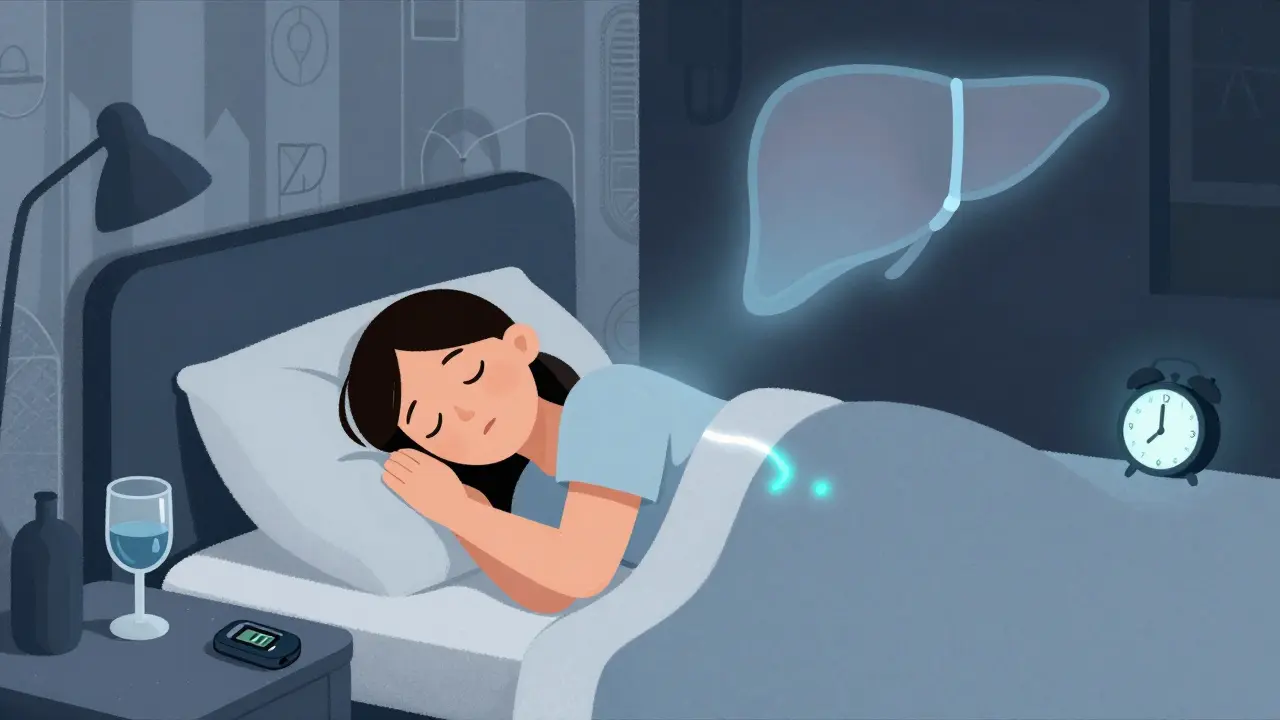
Your liver is your body’s glucose factory. When you haven’t eaten, it breaks down stored glycogen or makes new glucose from proteins and fats to keep your blood sugar stable. Alcohol shuts that down. Ethanol metabolism in the liver uses up NAD+, a key enzyme cofactor needed for glucose production. Without it, your liver can’t release glucose into your bloodstream-even when your levels are already dropping. This isn’t just a delay. Research shows alcohol can reduce glucose production by up to 37% for up to 8 hours after drinking. If you’re on insulin or a sulfonylurea like glipizide or glyburide, your body is already being pushed to lower blood sugar. Alcohol adds fuel to that fire. The result? A dangerous double hit: your meds are lowering glucose, and your liver can’t respond to save you.Which Diabetes Medications Are Most Dangerous With Alcohol?
Not all diabetes drugs react the same way. Some are riskier than others.- Insulin: Alcohol can extend hypoglycemia risk for up to 24 hours. That means a drink at dinner could cause a low at 3 a.m. while you’re asleep.
- Sulfonylureas (glyburide, glipizide, glimepiride): These drugs force your pancreas to pump out insulin regardless of your blood sugar. Alcohol makes this effect stronger. Studies show they increase hypoglycemia risk by 2.3 times when mixed with alcohol.
- Metformin: While it doesn’t directly cause low blood sugar, alcohol increases the risk of lactic acidosis-a rare but deadly condition. The FDA requires a boxed warning on metformin labels because alcohol raises this risk by 5.7 times. Symptoms? Confusion, rapid heartbeat, muscle pain, nausea. It’s often mistaken for being drunk.
- Chlorpropamide: This older sulfonylurea can cause a disulfiram-like reaction-flushing, vomiting, fast heartbeat-even with just one drink. It’s rarely prescribed today, but if you’re still on it, alcohol is off-limits.
How Much Alcohol Is Safe? The Real Numbers
There’s no universal “safe” amount. But guidelines from the American Diabetes Association give you a starting point:- Women: No more than one drink per day
- Men: No more than two drinks per day
- 12 oz of regular beer (about 150 calories, 13g carbs)
- 5 oz of wine (about 120 calories, 4g carbs)
- 1.5 oz of distilled spirits (vodka, whiskey, gin-about 100 calories, 0g carbs)
When You Drink, Do This-No Exceptions
If you choose to drink, treat it like a medical procedure. Follow these steps every single time:- Never drink on an empty stomach. Eat a meal with protein and complex carbs before you start. Skipping food turns alcohol into a hypoglycemia bomb.
- Check your blood sugar before you drink. If it’s below 100 mg/dL, eat something first. Don’t wait.
- Check again 2 hours after your last drink. This is when levels often start falling.
- Check before bed. If your blood sugar is under 100 mg/dL, eat a snack with slow-digesting carbs-like peanut butter on whole wheat or a small apple with cheese.
- Wear your medical ID. If you pass out, paramedics need to know you have diabetes. A bracelet cuts emergency response time by nearly half.
- Tell someone. Make sure a friend knows you have diabetes. Alcohol masks low blood sugar symptoms-sweating, shakiness, confusion-making them look like intoxication.
What Happens When You Don’t Follow the Rules
Real stories from real people tell the truth better than statistics. One user on Reddit described passing out after tequila shots. Friends thought he was drunk. His blood sugar was 42 mg/dL. He woke up in the ER. Another, on the ADA forum, had three glucagon injections after drinking two beers with insulin. He didn’t realize the low would hit 8 hours later-while he was asleep. A 2021 study found that 68% of hypoglycemia ER visits in young adults involved alcohol-and 82% happened between 11 p.m. and 6 a.m. That’s when your body’s natural defenses against low blood sugar are weakest. Even worse, 38% of people who had alcohol-related lows didn’t recognize the symptoms because alcohol dulled their thinking. They didn’t check their glucose. They didn’t eat. They just passed out.What to Drink-and What to Avoid
Not all alcoholic drinks are created equal. Here’s what to pick:- Best choices: Vodka or gin with soda water and lime, dry white wine (under 1g sugar per serving), light beer (under 5g carbs per 12 oz)
- Avoid: Sweet wines, cocktails with juice or syrup, regular soda mixers, flavored rum or liqueurs

New Tech Is Helping-But It’s Not a Free Pass
New continuous glucose monitors (CGMs) like Dexcom’s G7, released in late 2023, now let you log alcohol intake. The app can warn you if your glucose is dropping faster than expected after a drink. That’s helpful-but it’s not a magic shield. CGMs can’t predict how your liver will react. They can’t override the metabolic shutdown alcohol causes. They’re a tool, not a rulebook. You still need to eat, monitor, and plan.What’s Changing in 2026?
Doctors are starting to screen for alcohol use during every diabetes checkup. The AUDIT-C questionnaire-three simple questions about drinking habits-is now used by 78% of primary care physicians, up from 54% in 2018. Researchers are also testing machine learning models to predict who’s most at risk. Factors like liver function, medication type, sleep patterns, and even genetic differences in alcohol metabolism (CYP2E1 enzyme variants) may soon help tailor advice down to the individual. But here’s the bottom line: no algorithm replaces your own awareness. If you’re on diabetes meds and you drink, you’re playing with fire. The risk isn’t theoretical. It’s measurable. It’s documented. It’s happening right now.Final Rule: If You’re Not Sure, Don’t Drink
The American Diabetes Association doesn’t say you must quit alcohol. But they do say: know your risk. Know your meds. Know your body. If you’ve had a low blood sugar episode before, if you don’t feel the warning signs, if you’re on insulin or sulfonylureas, if you’re older or have liver disease-then alcohol isn’t worth it. One drink might seem harmless. But one drink can turn into one emergency. One night. One missed check. One sleepless hour where your body can’t save you. Your health isn’t negotiable. Your safety isn’t optional. If you choose to drink, do it with eyes wide open. If you don’t know how to do that safely? Skip it. There’s no prize for taking the risk.Can I drink alcohol if I have type 2 diabetes and take metformin?
You can, but with serious caution. Metformin doesn’t cause low blood sugar on its own, but alcohol increases your risk of lactic acidosis-a rare but life-threatening condition. The FDA warns that combining alcohol with metformin raises this risk by 5.7 times. Symptoms include nausea, muscle pain, rapid heartbeat, and confusion. If you drink, limit it to one drink per day, never on an empty stomach, and avoid binge drinking. If you feel unwell after drinking, seek help immediately.
How long after drinking alcohol can I get a low blood sugar?
Low blood sugar can happen within 2 to 3 hours after drinking-but it can also strike 8 to 24 hours later, especially if you’re on insulin or sulfonylureas. The liver’s ability to make glucose stays suppressed for hours after alcohol leaves your system. That’s why checking your blood sugar before bed is critical. A drink at dinner could cause a low at 2 a.m. while you’re asleep.
Is wine safer than beer or liquor for people with diabetes?
Dry wine (like Sauvignon Blanc or Pinot Noir) is often the safest choice because it has less than 1 gram of sugar per 5 oz serving. Sweet wines (like Moscato or Port) can have 8-14 grams of sugar-enough to spike your blood sugar then crash it later. Beer has carbs (12 oz = 10-15g), and liquor is carb-free but dangerous when mixed with sugary drinks. The key isn’t the type of alcohol-it’s what you mix it with and whether you eat with it.
Why do I feel drunk even when my blood sugar is low?
Alcohol and low blood sugar cause similar symptoms: dizziness, confusion, slurred speech, shakiness, and fatigue. This overlap is dangerous. People often mistake a severe low for intoxication-and vice versa. If you’re drinking and feel off, check your blood sugar immediately. Don’t assume you’re just drunk. You could be in danger.
Should I carry glucagon if I drink alcohol with diabetes?
Yes-if you’re on insulin or sulfonylureas, you should always have glucagon on hand. Alcohol increases the risk of severe hypoglycemia, especially at night. If you pass out or can’t swallow, glucagon is the only thing that can raise your blood sugar fast enough. Make sure someone close to you knows how to use it. Keep it with you when you go out.
Can I drink alcohol if I have type 1 diabetes?
You can, but the risks are higher. Type 1 diabetes means you rely entirely on insulin, and alcohol can delay or mask low blood sugar for up to 24 hours. Many people with type 1 report unexpected lows hours after drinking-even if they checked their sugar before bed. Use your CGM, eat with alcohol, check your levels overnight, and never drink alone. Talk to your endocrinologist about adjusting insulin doses if you plan to drink regularly.





Ian Long
8 January 2026 - 01:41 AM
Man, I drank two beers after dinner last week and woke up at 3 a.m. sweating like I was in a sauna. Thought I was having a panic attack. Glucometer said 38. Had to chug orange juice in the dark like a zombie. Never again. This post saved my life.
Alicia Hasö
9 January 2026 - 21:03 PM
Let me tell you something important-this isn’t just about numbers on a screen. It’s about your future. Every time you ignore the warnings, you’re gambling with your organs, your brain, your family’s peace of mind. Alcohol doesn’t care if you’re ‘just having one.’ Your liver doesn’t negotiate. Your pancreas doesn’t take breaks. Please, for the love of everything good in this world-check your levels. Eat first. Tell someone. Wear your ID. You’re worth more than a night out.
Micheal Murdoch
11 January 2026 - 17:33 PM
I used to think ‘one drink’ was harmless. Then I watched my dad pass out after a glass of wine-glucagon shot, ER, three days in the hospital. He’s on metformin. No sulfonylureas. No insulin. And still-alcohol shut down his liver’s backup system. The science here isn’t just valid-it’s personal. We need to stop treating this like a lifestyle choice and start treating it like a medical condition with real consequences. Your body doesn’t have a ‘reset’ button after a binge.
And yeah, CGMs help-but they’re not magic. They don’t stop the ethanol from poisoning your gluconeogenesis. You still have to eat. You still have to be smart. No app replaces discipline.
Jeffrey Hu
12 January 2026 - 14:04 PM
Everyone’s acting like this is new info. The FDA boxed warning on metformin has been there since 2005. The ADA guidelines have been unchanged since 2012. People just ignore them because they want to drink. This isn’t a medical mystery-it’s a behavioral failure. Stop pretending you’re special. Your liver doesn’t care if you’re ‘healthy otherwise.’
Chris Kauwe
14 January 2026 - 12:40 PM
Alcohol is a Western decadence that’s killing our diabetic population. In my country, we don’t mix medicine with recreational toxins. We don’t celebrate ignorance. This post is correct: if you’re on insulin or sulfonylureas, you’re not just risking your health-you’re risking public resources. ER visits from drunk diabetics cost taxpayers $1.2 billion last year. This isn’t personal-it’s a systemic failure of accountability.
Meghan Hammack
15 January 2026 - 06:31 AM
My mom had a low at 2 a.m. after a glass of wine. She didn’t know what was happening. My dad thought she was just tired. She ended up in the hospital. I cried for three days. Now I make her drink only with me-and I check her glucose every hour. It’s not about being controlling. It’s about being alive. Please, if you’re reading this-don’t wait for your version of this to happen.
RAJAT KD
15 January 2026 - 20:09 PM
Always eat protein before drinking. Peanut butter + apple works. Always. No exceptions.
Darren McGuff
16 January 2026 - 16:08 PM
I’ve been a diabetes educator for 18 years. I’ve seen hundreds of cases where people thought they were ‘fine’ because they checked before bed. The truth? The drop comes later. I had a patient who drank on Friday night, checked at 11 p.m.-140. Woke up Saturday at 4 a.m. at 32. Glucagon didn’t work the first time. He was unconscious. His wife didn’t know how to use the pen. He nearly died. Don’t be that person. Know your glucagon. Teach your people. Write it on your hand if you have to.
Heather Wilson
18 January 2026 - 10:31 AM
Let’s be honest-this post is overly dramatic. Yes, alcohol can cause hypoglycemia. But so can skipping meals, stress, over-exercising, and even certain antibiotics. Why is alcohol singled out like it’s the devil? Most people with diabetes drink responsibly. The real issue is poor glycemic management, not the beverage. Also, ‘one drink’ is not a medical procedure. You’re making people paranoid. This isn’t helping-it’s fearmongering.
Matthew Maxwell
19 January 2026 - 23:31 PM
If you’re choosing to drink alcohol while on insulin, you’re not just irresponsible-you’re selfish. You’re putting your family, your friends, your EMTs, your doctors through trauma for the sake of a buzz. You think you’re being ‘cool’? You’re being a liability. Stop romanticizing your poor choices. This isn’t a lifestyle. It’s a death sentence waiting to happen. Quit. Now.
Lindsey Wellmann
21 January 2026 - 18:10 PM
OK but like… I had a vodka soda with lime last night 🍸 and my CGM went from 110 to 68 in 4 hours 😱 I screamed so loud my dog ran out of the room. I ate a banana and cried into my pillow. But hey-still alive. 🙏✨ #DiabetesLife #AlcoholIsTheEnemy
Ashley Kronenwetter
21 January 2026 - 22:24 PM
The ADA guidelines are a good starting point, but individual variability is extreme. Factors like body weight, liver enzyme activity, and medication timing all affect outcomes. I recommend consulting a clinical pharmacist for personalized risk assessment before consuming alcohol. Many hospitals now offer this service free of charge.
Aron Veldhuizen
22 January 2026 - 04:12 AM
Actually, this post ignores the real issue: insulin resistance. People with type 2 diabetes who drink are often sedentary and obese. The alcohol isn’t the villain-it’s the lifestyle. If you exercised more and ate real food, you wouldn’t need to panic about one drink. This fear-based approach doesn’t solve anything. It just makes people feel guilty. Let’s fix the root cause, not the symptom.
Drew Pearlman
23 January 2026 - 17:06 PM
I’ve been living with type 1 for 22 years and I still drink-sometimes. But I’ve learned. I eat a protein-heavy meal before. I drink slowly. I check every 90 minutes. I sleep with my meter on the pillow. I have glucagon by the bed. I tell my partner. I don’t do shots. I don’t do mixed drinks. I don’t drink on empty stomachs. And I’ve never had a hospital visit because of it. It’s not about quitting. It’s about mastering the game. You can still live a full life. You just have to be smarter than the alcohol.
Don’t let fear stop you. Let knowledge guide you. You’ve got this.