Every year, millions of Medicare beneficiaries get a free, one-on-one review of all their medications. But too many people show up unprepared - and miss out on real benefits. If you’re on multiple prescriptions, take over-the-counter drugs, or use supplements, this review could catch dangerous interactions, lower your costs, or even save your life. The key? Preparation.
What Exactly Is a Medicare Annual Medication Review?
This isn’t just a chat with your pharmacist. It’s a formal, federally required service called a Comprehensive Medication Review (CMR), part of Medicare Part D’s Medication Therapy Management (MTM) program. By law, your drug plan must offer it at least once a year if you qualify. The goal? To make sure every pill, capsule, and herbal drop you take is safe, necessary, and working the way it should.
The review covers everything: prescription drugs, OTC pain relievers like ibuprofen or antacids, vitamins, fish oil, herbal teas, even patches or eye drops. A licensed pharmacist spends 30 to 60 minutes with you - in person or over video - going through each one. They check for duplicates, harmful interactions, side effects you might not have mentioned, and whether you’re even taking them correctly.
You’ll walk away with three things: a written summary, a personalized action plan, and an updated list of every medication you use. This isn’t just paperwork - it’s your medication blueprint for the year ahead.
Who Qualifies for the Review?
Not everyone gets invited. The rules changed in 2025 to make it easier to qualify. You’re eligible if you:
- Have at least three chronic conditions (like diabetes, heart disease, COPD, high blood pressure, or arthritis)
- Take at least two to eight Medicare Part D-covered medications (including maintenance drugs)
- Spent at least $1,623 out-of-pocket on covered prescriptions in the last year
That’s lower than before. In 2023, the threshold was over $4,000. Now, more seniors - especially those managing multiple conditions but with modest drug costs - can get this service. If you’re unsure, call your Part D plan. They’re required to notify you if you’re eligible.
Why This Review Matters More Than You Think
Most people think their doctor knows everything they’re taking. They don’t. You might get blood pressure meds from your cardiologist, diabetes drugs from your endocrinologist, and painkillers from your orthopedist. Each one might not know what the others prescribed. Add in your daily aspirin, melatonin for sleep, and turmeric capsules - and the risk of dangerous overlaps skyrockets.
Studies show that seniors on eight or more medications have a 1 in 3 chance of experiencing a harmful drug interaction. Many of these go undetected for years. One 2023 study found that 42% of Medicare beneficiaries on multiple drugs were taking something they didn’t need - like duplicate painkillers or outdated antibiotics.
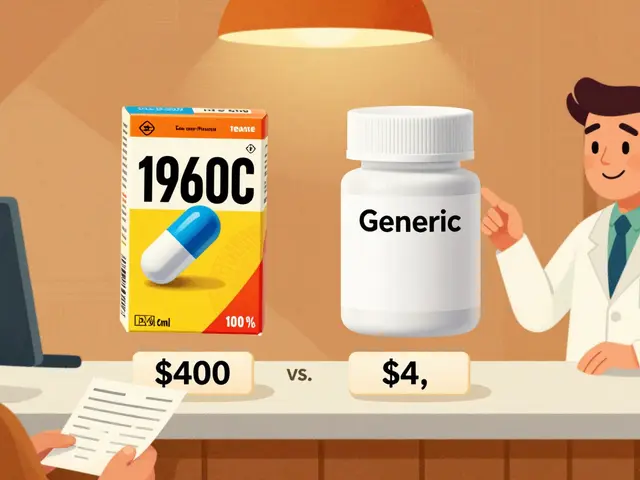
The CMR catches these. In fact, beneficiaries who prepared well and attended their review were 78% more likely to report improved health outcomes, according to the Medicare Rights Center. One woman in Ohio found out her fish oil was dangerously interacting with her blood thinner. Another saved $800 a year after switching to a generic version his pharmacist recommended.
What to Bring: The 5-Item Checklist
Don’t wing this. Showing up with just a mental list is the #1 reason reviews fail. Here’s what you need - and why:
- All medications in original bottles - This includes prescriptions, OTC drugs, supplements, and even topical creams. The pharmacist needs to see the label: name, dose, frequency, and expiration date. Don’t rely on pill organizers - they don’t tell the whole story.
- A written list - Make a simple list: drug name, dose, how often you take it, and why. Use a notebook or print this out. If you have 10+ meds, use a spreadsheet. Include the reason for each - e.g., “Lisinopril 10mg - for blood pressure.”
- Recent lab results or hospital discharge papers - Did your kidney function change last month? Did you get hospitalized for dizziness? These details help the pharmacist spot cause-and-effect links between your meds and symptoms.
- A list of questions - Write down anything confusing: “Why am I taking this?” “I feel dizzy after lunch - is it the pill?” “Can I stop this one?” Don’t be shy. This is your time.
- A family member or friend - Bring someone who can listen, remember, and ask follow-up questions. Memory fades fast, especially under stress. Two sets of ears are better than one.
Pro tip: Take photos of each bottle with your phone. If you forget something at home, you can still show the pharmacist the images.

What to Do Before the Appointment
Set aside 45 to 90 minutes - yes, it’s a lot - but it’s worth it. Here’s how to use that time wisely:
- Count your pills - Open each bottle and count how many are left. If you’re supposed to take one daily and you have 30 left after 10 days, you’re not taking them regularly. That’s critical info.
- Track side effects - Did you start feeling tired after adding a new med? Did your stomach hurt after switching brands? Note the timing and severity. “I feel foggy every afternoon” is better than “I feel weird.”
- Check costs - Are you skipping doses because it’s too expensive? Say so. Pharmacists can often find cheaper alternatives, coupons, or even patient assistance programs.
- Review your timeline - When did you start each med? Did you stop one recently? Did your doctor change your dose? Write it down. A timeline helps the pharmacist see patterns.
One woman in Florida spent 30 minutes doing this and discovered she’d been taking two different versions of the same blood pressure pill - one from her doctor, one from a mail-order pharmacy. The pharmacist caught it and stopped the duplicate. She saved $120 a month.
What Happens During the Review
The pharmacist will:
- Compare your physical meds to your list
- Check for drug interactions using real-time databases
- Ask about how you take your meds - do you use a pillbox? Do you forget doses?
- Identify any unnecessary or outdated prescriptions
- Suggest cheaper or safer alternatives
- Explain what each drug does and why
You’ll get a Medication Action Plan (MAP) - a clear, written guide on what to do next. Maybe you need to stop one med. Maybe you need to split a dose. Maybe you need a new prescription. The plan is yours to keep.
You’ll also get a Personal Medication List (PML) - an official, updated version of everything you take. Give this to every doctor you see. Keep it in your wallet. Update it every time something changes.
Common Mistakes People Make
Don’t fall into these traps:
- “I don’t need to bring my vitamins.” - Wrong. Herbal supplements like St. John’s Wort can interfere with antidepressants. Ginkgo biloba can thin your blood. The pharmacist needs to know.
- “My doctor already knows what I take.” - Not necessarily. Most doctors don’t have access to your full pharmacy history unless you give it to them.
- “I’ll just remember what was said.” - Studies show people forget 50% of medical advice within 48 hours. Write it down.
- “I’m not eligible - I don’t take enough meds.” - You might be. The threshold is now $1,623 in out-of-pocket costs. That’s less than $136 a month.

What If You’re Not Eligible?
Even if you don’t qualify for the official CMR, you can still ask your pharmacist for a free medication review. Many community pharmacies offer them - no insurance needed. Just walk in and say, “Can you help me review all my meds? I’m on several and want to make sure they’re safe together.”
Some plans also offer quarterly Targeted Medication Reviews (TMRs) if you’re flagged for potential issues. Don’t ignore those calls - they’re your safety net.
Next Steps After the Review
Your work isn’t done after the meeting:
- Keep your updated Personal Medication List in your wallet, purse, or phone.
- Share the Medication Action Plan with your primary care doctor.
- Set a reminder in your phone: “Check meds again in 3 months.”
- If you start a new medication - even a one-time antibiotic - update your list right away.
- If you notice new side effects, call your pharmacist before calling your doctor. They can often fix it faster.
Medicare’s program is designed to keep you healthy and out of the hospital. But it only works if you show up ready.
Do I have to pay for the Medicare Annual Medication Review?
No. The Comprehensive Medication Review is a free benefit included in your Medicare Part D plan. There’s no copay, no deductible, and no extra charge. It’s part of what your plan is required to provide by law.
Can I do the review over the phone or video instead of going to the pharmacy?
Yes. Medicare now allows telehealth CMRs. Your plan will contact you to schedule a call or video chat with a pharmacist. You’ll still need to have your medications ready to show on camera, and you’ll receive the same written summary and action plan as if you’d gone in person.
What if I don’t have all my pill bottles? Can I still have the review?
You can still have the review, but it will be less effective. Pharmacists rely on labels to verify exact doses, expiration dates, and prescribing doctors. Without bottles, they can’t confirm what you’re actually taking. You’ll likely be asked to reschedule when you have your meds ready. Taking photos of labels ahead of time can help if you forget the bottles.
How often should I update my medication list?
Update it every time you start, stop, or change a medication - even if it’s just a one-week antibiotic. Keep your Personal Medication List current at all times. Many seniors keep it in their wallet or on their phone. Share it with every new doctor, ER visit, or hospital admission.
What if the pharmacist says I don’t need one of my medications?
Don’t stop it on your own. The pharmacist will recommend you talk to your doctor about discontinuing it. They’ll send a note to your prescriber explaining why. Your doctor will decide if it’s safe to stop. Never stop a prescription without medical advice - even if the pharmacist says it’s unnecessary.
Can I get a medication review if I’m on Medicaid, not Medicare?
Medicaid programs vary by state. Some offer similar medication reviews, but they’re not federally required like Medicare’s CMR. Contact your state’s Medicaid office or local pharmacy to ask if they offer a free medication review for Medicaid recipients.
What if I live in a rural area and can’t get to a pharmacy?
You still qualify for a telehealth review. Call your Part D plan and ask to schedule a phone or video appointment. Many plans now offer mail-in kits with pre-addressed envelopes to send your meds for review - though this is less common. If you’re homebound, ask about mobile pharmacy services in your area.
Is the Personal Medication List official? Can I show it to my doctor?
Yes. The Personal Medication List (PML) is a standardized CMS document that doctors recognize as an official record of your current medications. Bring it to every appointment. Many clinics now scan it into your electronic health record. It’s one of the most important documents you’ll ever carry.
Final Tip: Make This a Habit
This isn’t a one-time task. Medication management is a lifelong skill. Set a calendar reminder for your annual review date. Keep your list updated. Talk to your pharmacist regularly. The more you engage, the safer you’ll be. Your health isn’t just about the pills you take - it’s about knowing why you take them, and making sure they’re still the right ones.





Harry Henderson
27 January 2026 - 09:26 AM
This is the most important thing no one tells you about Medicare and I'm pissed no one told me sooner. I had a stroke last year because I was taking three blood thinners and didn't know it. The pharmacist caught it during my CMR. I'm telling everyone I know. Don't wait until you're in the ER. Bring your bottles. Write it down. Show up ready. This isn't optional - it's survival.
suhail ahmed
27 January 2026 - 22:32 PM
Bro, this is the real MVP of Medicare - not the free gym membership or the dental discount. I'm from India and I've seen my uncle in Delhi juggle 12 meds with no one to help him. Here, you get a trained pharmacist sitting down with you like family. That's magic. Bring the bottles, bring your cousin, bring your coffee. This ain't a chore - it's your golden ticket to not keeling over next Tuesday.
Paul Taylor
27 January 2026 - 22:36 PM
Look I've been doing this for 15 years and I can tell you the CMR is the single most underutilized tool in senior healthcare. People think it's just a chat but it's not. It's a full forensic audit of your entire pharmacological life. You need to bring every single thing you put in your body including that turmeric capsule you take because your yoga instructor said it 'cleanses your chakras'. The pharmacist doesn't care about your beliefs they care about your INR levels. And yes you need to count your pills because if you have 40 left after 14 days you're not taking them right and that's a red flag they'll flag. Also stop thinking your doctor knows what you're on they're drowning in paperwork and they're not reading your pharmacy records unless you hand them the PML. This isn't a suggestion it's your lifeline.
Andrew Clausen
29 January 2026 - 07:39 AM
Correction: The threshold for eligibility in 2025 is not $1,623 out-of-pocket. That figure is the 2024 threshold. The 2025 threshold is $1,725 as per CMS final rule 98-217. The article is outdated. Also, the term 'Comprehensive Medication Review' is technically correct but the official CMS designation is 'Medication Therapy Management Comprehensive Review'. Precision matters. And no, you cannot use photos of pill bottles as a substitute for physical bottles if the plan requires an in-person review. That's a common misconception. The label must be legible and unaltered. This post is well-intentioned but dangerously imprecise.
Anjula Jyala
30 January 2026 - 17:54 PM
Let me cut through the fluff. You don't need a checklist you need discipline. If you're on more than 5 meds you're already in danger zone. The pharmacist isn't your friend they're your last line of defense against polypharmacy disaster. You think St John's Wort is harmless? It's a CYP3A4 inducer that will nullify your anticoagulants and SSRIs. Ginkgo? Platelet aggregation inhibitor. You're not 'supplementing' you're playing Russian roulette with your liver and kidneys. Bring the bottles or don't bother. And stop saying 'my doctor knows' - your doctor has 12 minutes per patient and they're not cross-referencing your CVS with your Walgreens with your mail-order. You're the only one who can protect yourself. Do it right or die quietly.
Kirstin Santiago
1 February 2026 - 00:09 AM
I just did my CMR last week and it was actually kind of nice? Like someone finally cared enough to ask me why I was still taking that old painkiller from 2018. I brought my list and my pills and my daughter and the pharmacist didn't judge me for having 3 kinds of melatonin. She just said 'oh sweetie you don't need two of these' and helped me switch to a cheaper blood pressure med. I cried a little. It felt good to be seen. If you're nervous just go. You've got nothing to lose and your health to gain.
Kathy McDaniel
1 February 2026 - 18:31 PM
OMG I forgot my pill bottles and brought photos instead and they still did the review!! I was so nervous but the pharmacist was chill and said pics were fine as long as they were clear. I didn't even know you could do it on video!! I did mine from my couch in my robe. Also I found out I was taking two different versions of my heart med and they fixed it and now I save $80 a month. This is the best thing ever. I'm telling my whole book club.
Patrick Merrell
2 February 2026 - 20:54 PM
People need to stop treating this like a freebie. This is a responsibility. You don't get to be lazy with your health. If you can't be bothered to bring your pills or write down your meds then you don't deserve to live past 70. I've seen too many people die from preventable interactions because they thought 'it's just a vitamin' or 'my doctor knows'. You're not special. You're not exempt. You're just another statistic waiting to happen. Do the work. Or don't. But don't cry about it when your kidneys give out.