When you pick up a prescription, you might see two options: the name you recognize from TV ads, or a simpler label with a different color and shape. It’s the same medicine-just cheaper. But should you choose the generic? Or stick with the brand? For many people, this isn’t just a cost question. It’s about trust, fear, and confusion. And it shouldn’t be.
What’s the Real Difference Between Generic and Brand Medications?
The active ingredient in a generic drug is exactly the same as in the brand-name version. If your doctor prescribed atorvastatin, the generic version of Lipitor, it contains the same molecule that lowers cholesterol. The FDA requires this. No exceptions.
What’s different? The color, the shape, the filler ingredients-things like starch or dye that hold the pill together. These don’t affect how the drug works. The FDA calls this bioequivalence. It means the generic must deliver the same amount of medicine into your bloodstream at the same speed as the brand. The acceptable range? Between 80% and 125% of the brand’s performance. In reality, most generics are within 3-4% of the original.
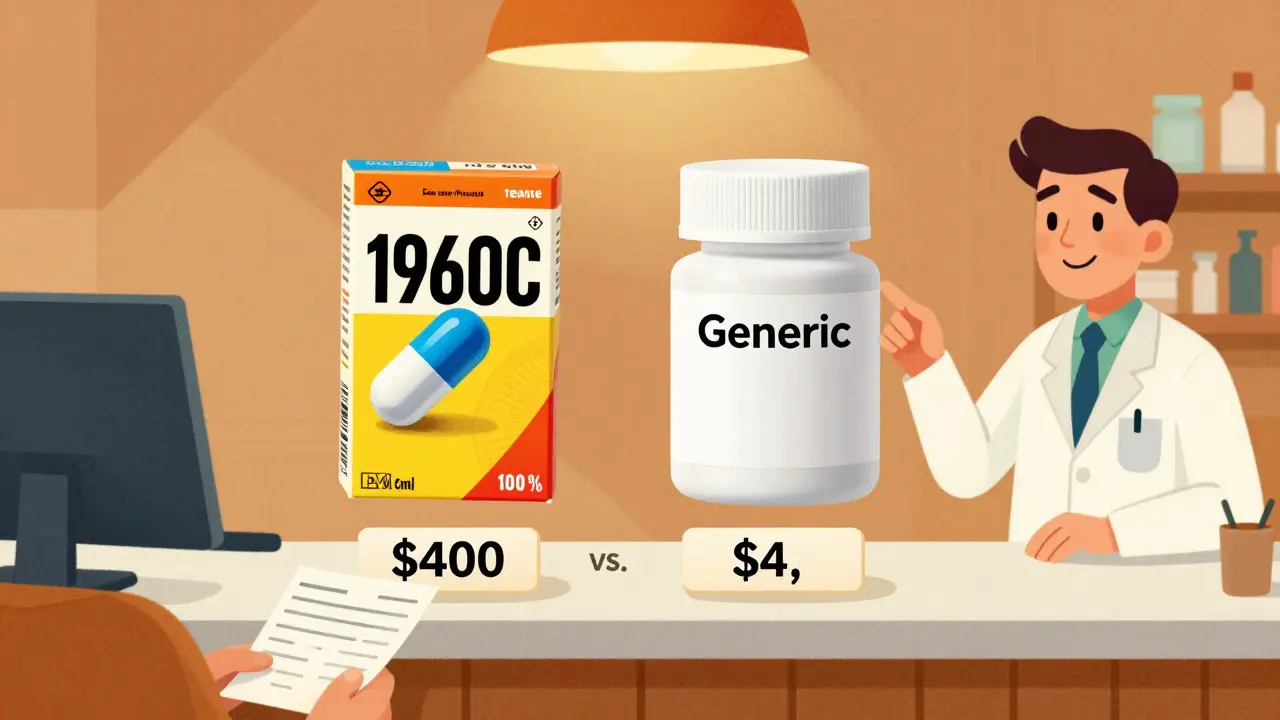
Here’s the kicker: 90% of all prescriptions filled in the U.S. are generics. Yet they make up only 23% of total drug spending. That’s because a 30-day supply of generic sertraline (Zoloft) can cost $4, while the brand runs $400. Generic atorvastatin? As low as $0.10 per pill. Brand? Over $4.50.
Why Do People Still Choose Brand-Name Drugs?
It’s not about science. It’s about perception. Many patients believe brand-name drugs are stronger, safer, or more reliable. That’s understandable. Big companies spend millions on advertising. You see the logo. You hear the jingle. You remember the name.
But here’s what the data says: a 2019 review of 47 studies involving nearly 10,000 patients found that generics performed identically to brand-name drugs in 98.5% of cases. That includes heart medications, antidepressants, diabetes drugs, and more.
Still, some people swear they feel worse on generics. Often, it’s not the drug-it’s the change. Switching from a blue oval pill to a white round one can trigger anxiety. Some patients report headaches, dizziness, or a sense that the medication “isn’t working.” In most cases, these symptoms fade within days. But they’re real enough to make people switch back.
When Generics Might Not Be the Best Choice
There are exceptions. And they matter.
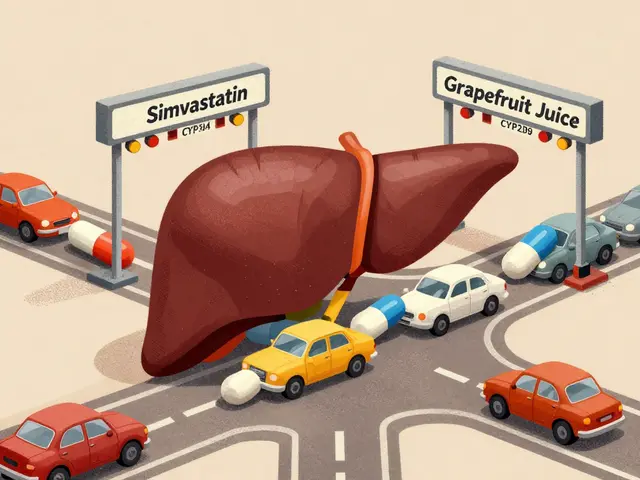
Drugs with a narrow therapeutic index are the main concern. These are medications where even a tiny change in blood levels can cause harm-or make the drug useless. Examples include:
- Warfarin (blood thinner)
- Levothyroxine (thyroid hormone)
- Phenytoin (anti-seizure)
- Carbamazepine (anti-seizure)
In these cases, even small differences in absorption can lead to serious problems. For levothyroxine, switching between generic brands can cause TSH levels to fluctuate. That’s why 28 states require doctors to specifically approve generic substitution for thyroid meds. Some pharmacists even recommend sticking with one manufacturer to avoid variability.
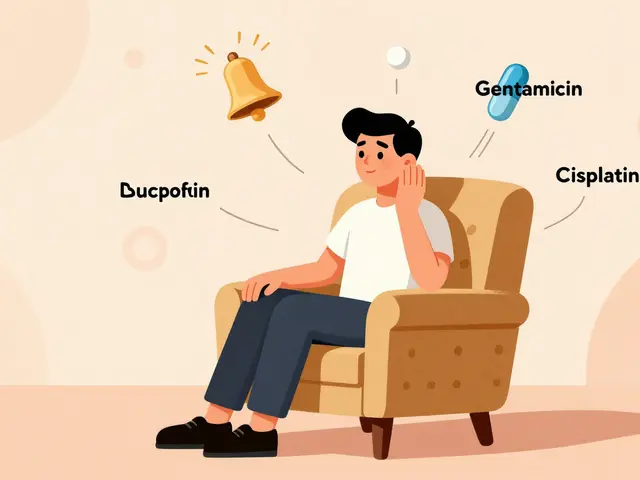
Another issue: complex delivery systems. Inhalers like Advair Diskus or patches like Fentanyl don’t just contain the drug-they rely on precise engineering to deliver it. A 2016 study found that 12% of patients switching to a generic inhaler had trouble using it properly. The active ingredient was the same, but the device felt different. That led to underdosing.
And then there’s extended-release pills. Some generic versions of Wellbutrin XL (bupropion) were found to release the drug faster than the brand, leading to lower effectiveness and more side effects. The FDA issued a warning in 2012. Today, some generics are approved as “AB-rated” (safe to substitute), while others aren’t. Always check the FDA’s Orange Book to see if your generic has an “AB” rating.

Cost Isn’t Just a Number-It’s a Health Issue
Let’s say your doctor prescribes Lyrica for nerve pain. The brand costs $650 a month. You can’t afford it. So you skip doses. Or stop taking it. That’s not rare. One in three Americans skips medication because of cost.
But the generic-pregabalin-costs $15. Same effect. Same side effects. Same results. One patient wrote on Drugs.com: “Switched to generic. Pain control is identical. I can finally afford to take it every day.”
That’s the real story. A 2020 study from the American College of Physicians found that 29% of people on brand-only drugs skip doses due to cost. Only 14% of those on generics do. That’s a 15-point gap. And it’s not about willpower. It’s about access.
Doctors know this. That’s why many now prescribe generics by default. If you’re worried, ask: “Is there a generic? And is it right for me?”
How to Make the Switch Safely
Switching from brand to generic isn’t risky for most people. But it’s not something you should do without a plan.
Here’s how to do it right:
- Ask your pharmacist if your prescription has a generic. They can tell you if it’s AB-rated and which manufacturer makes it.
- Check the FDA’s Drugs@FDA database. Search your drug name. Look for “therapeutic equivalence” ratings. “AB” means it’s interchangeable. “BN” or “NR” means it’s not.
- Stick with one pharmacy. If your generic switches manufacturers every month, your pill might look different each time. That’s confusing. A consistent pharmacy can track which version you’re on.
- Watch for changes. If you feel different after switching-more tired, more anxious, less pain relief-call your doctor. Don’t assume it’s “all in your head.”
- Use visual aids. Take a photo of your pill. Save it on your phone. If the shape or color changes, you’ll know it’s a different manufacturer-not a different drug.
Some states require pharmacists to notify you when switching to a generic. Others don’t. But you have the right to ask. And you have the right to refuse a substitution if you’re uncomfortable.
What About Branded Generics?
Ever heard of “branded generics”? These are drugs made by the original manufacturer but sold under a different name at a lower price. For example, Eli Lilly sells Humalog insulin as both a brand and an “authorized generic.” The formula is identical to the brand-but costs 20-30% less.
These are a smart middle ground. You get the brand’s reputation, the same manufacturing, and lower cost. They’re not always available, but they’re worth asking for-especially for chronic conditions.
What the Experts Say
Dr. Niteesh Choudhry from Harvard puts it plainly: “Brand-name medications are not always better. Many of them are highly expensive.”
Dr. Aaron Kesselheim from Brigham and Women’s Hospital studied over 100,000 patients switched from brand to generic warfarin. He found no increase in bleeding or clots. “The fear of generics is real,” he says, “but the data doesn’t support it.”
The FDA’s official stance? “Generic drugs have the same risks and benefits as their brand-name counterparts.”
And yet, 68% of patients are initially nervous about generics. That drops to 11% after a pharmacist explains how they’re tested. Education works.
What’s Changing Now?
The generic market is growing fast. In 2022, over 1,100 new generics were approved-more than double the number in 2016. The Inflation Reduction Act of 2022 will let Medicare negotiate prices for 10 high-cost drugs starting in 2026. That will push even more brands toward generic competition.
But challenges remain. Over 78% of the active ingredients in generics come from India and China. Supply chain issues can cause shortages. And complex drugs-like inhalers, eye drops, and injectables-are still lagging. Only 35% of off-patent complex drugs have generic versions.
The FDA is working on new rules to fix that. But for now, the message is clear: for most people, generics are safe, effective, and life-changing.
Final Thought: Your Health, Your Choice
Choosing between generic and brand isn’t about being smart or naive. It’s about being informed. The science is solid. The savings are huge. And the risks? Minimal-for most drugs.
If you’re on a chronic medication, ask your doctor: “Is there a generic? Is it right for me?” If you’re on a narrow therapeutic index drug, ask: “Should I stick with one manufacturer?”
Don’t let fear or confusion cost you your health. A $4 pill can do the same job as a $400 one. And sometimes, that’s the difference between taking your medicine-and not.




Mark Able
20 December 2025 - 01:53 AM
Bro I switched my cholesterol med to generic and saved like $380 a month. My doctor was like 'you sure?' and I was like 'dude I'm not dying, I'm just broke.' Now I can afford my Netflix and tacos. Generics are the real MVP.
Chris Clark
20 December 2025 - 21:39 PM
sooo i had this whole thing where i thought brand name was better cause my grandpa used to say 'if it dont say Pfizer on it, its not real medicine' lol
but then i read the FDA stuff and realized the fillers are just starch and dye, like, who cares if the pill is blue or white? my anxiety was the problem, not the drug.
switched to generic sertraline, same exact feeling, just cheaper. also my pharmacist said the 'AB rating' thing is key, always check that. also, take a pic of your pill. i did. saved it. now i dont freak out when it looks different.
William Storrs
22 December 2025 - 09:38 AM
Hey, I just want to say - this post is incredible. You’re not just sharing facts, you’re giving people their power back.
So many folks skip meds because they can’t afford them - and that’s not laziness, that’s systemic failure.
Switching to generics isn’t cutting corners, it’s choosing survival. And if you’re nervous? Talk to your pharmacist. Ask for the AB rating. Take a photo of your pill. Do it slow. You’ve got this.
And if you’re on thyroid meds? Stick with one brand. Don’t gamble with your TSH. Small changes matter. But for 90% of people? Generics are 100% fine. You’re not being cheap - you’re being smart.
James Stearns
24 December 2025 - 04:17 AM
It is, regrettably, a matter of considerable public misconception that pharmaceutical equivalence is tantamount to therapeutic equivalence. While the FDA mandates bioequivalence within an 80-125% range, the clinical implications of such variability - particularly in polypharmacy patients with renal or hepatic compromise - remain underappreciated.
Moreover, the notion that '90% of prescriptions are generics' is statistically misleading; it conflates volume with clinical significance. The most critical medications - anticoagulants, antiepileptics, immunosuppressants - remain disproportionately branded due to legitimate pharmacokinetic concerns.
One must not confuse affordability with appropriateness. To advocate for generic substitution without individualized risk assessment is not evidence-based medicine - it is cost-driven negligence.
Nina Stacey
24 December 2025 - 17:12 PM
i just wanna say i switched to generic warfarin last year and i was so scared i cried
my husband said 'you're gonna die' and i was like 'i might but at least i can pay rent'
and guess what i'm still alive and my INR is perfect
and i don't even remember what the brand pill looked like anymore
also my pharmacy switched me to a different generic and i thought i was dying but it was just the color
now i take a picture of every pill and i feel like a spy
if you're scared just talk to your pharmacist they are the real heroes
also why do people think brand is better like we're still in 1998
also i have anxiety and i think i'm allergic to the word 'filler' but i'm not
please just try it
Dominic Suyo
26 December 2025 - 11:34 AM
Oh wow, another feel-good corporate shill piece. Let me guess - Big Pharma just woke up and decided to be nice? Nah.
Generics are made in India and China where the FDA doesn't have teeth. You think they're testing every batch? Please. There's a reason why the EU bans half of them.
And 'AB-rated'? That's just a fancy word for 'we didn't catch the impurities yet'.
My cousin had a seizure after switching to generic phenytoin. The hospital said 'it's probably the generic'. They didn't even test it.
And now they're pushing this under the Inflation Reduction Act like it's a public service. It's a supply chain hostage situation.
Don't be fooled. This isn't about savings - it's about control.
Kevin Motta Top
27 December 2025 - 04:56 AM
Generic works. Save your money. Ask your pharmacist. Check the FDA. Done.
Alisa Silvia Bila
28 December 2025 - 16:27 PM
I used to be scared of generics too - I thought they were like knockoff sneakers that fall apart.
But then I switched my blood pressure med and nothing changed. I didn't feel 'off' or weird. My BP stayed steady.
Now I always ask my doctor for the generic first. If they say no, I ask why. Sometimes it's because it's a narrow index drug - and that's fair.
But most times? They just forget to mention it. So I remind them.
It's not about being cheap. It's about being practical. And honestly? It's kind of empowering to know you're not being scammed.
Marsha Jentzsch
29 December 2025 - 04:17 AM
YOU THINK IT'S SAFE?!?!?!
WHAT ABOUT THE TALC?!?!
THEY PUT TALC IN THE PILLS TO MAKE THEM LOOK PRETTY!!
AND THE TALC IS FROM CHINA AND IT'S CONTAMINATED WITH ASBESTOS!!
MY AUNT HAD LUNG CANCER AND SHE WAS ON GENERIC LEVOTHYROXINE AND THE PHARMACY SWITCHED BRANDS AND SHE DIED IN HER SLEEP!!
AND THE FDA IS IN THE POCKET OF BIG PHARMA AND THEY DON'T TEST ENOUGH!!
AND WHY DO YOU THINK THEY MAKE THE PILLS DIFFERENT COLORS?! TO CONFUSE YOU!!
THEY WANT YOU TO FEEL LIKE YOU'RE LOSING CONTROL SO YOU'LL STAY ON THE BRAND AND PAY MORE!!
YOU THINK YOUR 'AB RATING' MEANS SOMETHING?!?!
IT MEANS NOTHING!!
YOU'RE BEING MANIPULATED!!
STOP TRUSTING THE SYSTEM!!
Janelle Moore
29 December 2025 - 23:05 PM
Wait, I just realized - if generics are so identical, why do some of them have different side effects? Like, I took generic Wellbutrin and I felt like I was being electrocuted inside my brain. Brand didn't do that. Maybe the FDA is lying? Or maybe the 'same molecule' thing is a lie? I think they're testing on poor people and then selling the 'better' version to rich folks. I read it on a forum. It makes sense.