Personalized Medication Risk Calculator
How Medications Affect Women Differently
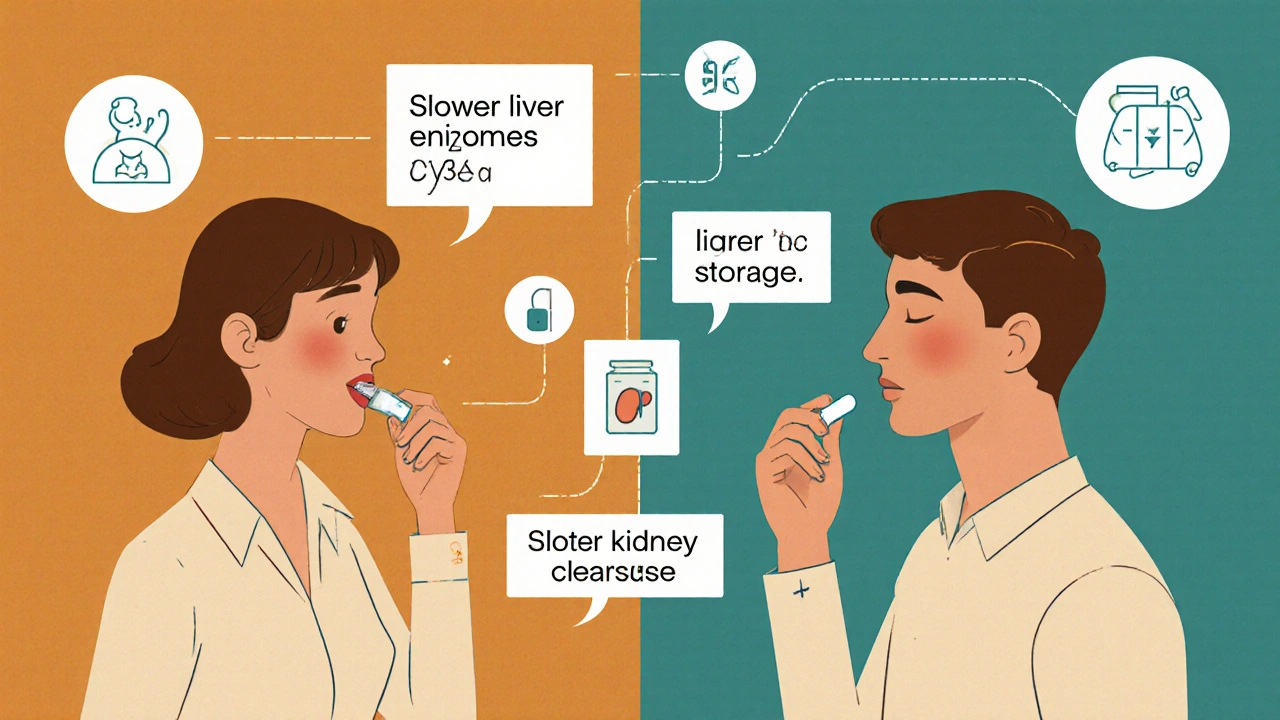
Women process medications differently due to biological factors: 40% less liver enzyme (CYP3A4), 10-12% more body fat, and 20-25% slower kidney clearance. These differences mean standard doses often cause more side effects for women.
Enter Your Information
Your Personalized Risk Assessment
Example: Zolpidem metabolism is 50% slower in women. After FDA dose reduction, adverse events decreased by 38%.
Women are nearly twice as likely as men to have serious side effects from the same medication at the same dose. It’s not because they’re more sensitive or overreacting. It’s because most drugs were tested mostly on men - and that’s still the standard today.
What’s Really Going On With Drug Dosing?
In the 1970s, the FDA stopped including women of childbearing age in early drug trials. The goal was to protect unborn babies. But that decision created a blind spot that never got fully fixed. Even after the 1993 NIH law required women to be included in clinical trials, researchers kept using male bodies as the default. By the time a drug hits the market, its dosing is based on how men’s bodies process it - not women’s.That’s why a woman taking the same pill as her husband might feel dizzy, nauseous, or groggy while he feels fine. Her body isn’t broken. The drug label is outdated.
Biological Differences That Change Everything
Women’s bodies work differently from men’s - not just in reproduction, but in how they handle medicine.For starters, women have about 40% less of a key liver enzyme called CYP3A4. That enzyme breaks down half of all prescription drugs, including statins, sleeping pills, and antidepressants. Slower breakdown means the drug stays in the system longer. Higher concentrations. More side effects.
Body fat matters too. On average, women have 10-12% more body fat than men. Fat-soluble drugs like diazepam (Valium) get stored in fat tissue and release slowly. That’s why a woman might still feel sedated the next morning after taking a standard dose that a man would clear by bedtime.
Kidney function is different too. Women clear drugs like lithium and some antibiotics 20-25% slower. Hormones play a role as well. Birth control pills can cut the effectiveness of the epilepsy drug lamotrigine by half. During certain phases of the menstrual cycle, metabolism can shift by up to 30%.
Real-World Examples: Drugs That Hit Women Harder
Some drugs have clear, documented sex-based risks:- Zolpidem (Ambien): Women metabolize it 50% slower. In 2013, the FDA cut the recommended dose for women by half - after years of reports about morning drowsiness, car accidents, and falls. Post-reduction, adverse event reports from women dropped by 38%.
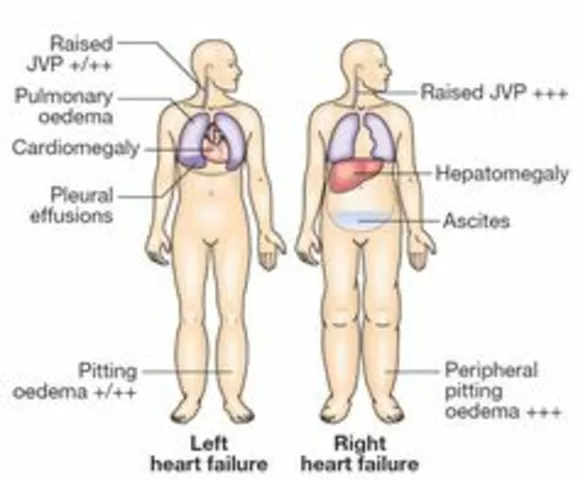
- Digoxin: Used for heart failure, this drug builds up to 20-30% higher levels in women at standard doses. That raises the risk of toxicity - including dangerous heart rhythms - by 40%.
- SSRIs like sertraline (Zoloft): Women report 1.5 to 2 times more nausea and dizziness. Men report more sexual side effects, but women are far more likely to quit the drug because of how they feel physically.
- Antipsychotics like haloperidol: Women are 2.3 times more likely to develop QT prolongation - a heart rhythm issue that can turn deadly.
- Antibiotics like sulfamethoxazole: Women have a 47% higher risk of severe skin reactions.
These aren’t rare cases. A 2020 study found that 86 FDA-approved drugs have known sex-based differences in how they’re processed or how they affect the body. And only 4% of drug labels tell you about them.
It’s Not Just Biology - It’s Behavior Too
Some researchers argue that biology isn’t the whole story. Harvard’s Dr. Sarah Richardson looked at 33 million adverse event reports and found something surprising: once you account for the fact that women take 56% more prescriptions than men on average, the gap in side effect rates shrinks to less than 5%.That doesn’t mean biology doesn’t matter. It means women are more likely to notice symptoms, report them, and seek help. Men often brush off dizziness or fatigue as “just tired.” Women are more likely to call their doctor.
Dr. Janine Austin Clayton from the NIH puts it simply: “Biological differences exist. But reporting behavior matters too.”
Who’s Getting Hurt?
The numbers are staggering:- Women make up just over half the U.S. population - but account for 63-70% of all severe adverse drug reactions.
- Every year, adverse drug reactions cost the U.S. healthcare system over $30 billion. Women shoulder most of that burden.
- A 2022 survey of 15,000 chronic pain patients found women were 2.1 times more likely to have to stop opioids because of side effects.
- On patient forums, 78% of women reported morning grogginess from standard zolpidem doses - compared to just 32% of men.
These aren’t theoretical concerns. They’re real people - mothers, sisters, coworkers - who are being harmed by outdated medical standards.
Why Aren’t Doctors Doing More?
Most doctors don’t know the data. A 2022 AMA survey found only 28% routinely consider sex differences when prescribing. Two out of three didn’t even know about the FDA’s 2013 zolpidem dose change for women.Drug labels don’t help. Out of 200 commonly prescribed medications, only 15 have sex-specific dosing instructions. The rest? Same dose. Same label. Same risk.
Even when studies show clear differences, it takes 10 to 15 years for guidelines to change. Zolpidem’s sex-based metabolism was known as early as 1992. It took 21 years for the FDA to act.

What’s Changing - and What’s Not
There’s progress. The FDA launched its “Sex and Gender Roadmap” in 2023, aiming to make sex a standard consideration in all drug reviews by 2026. The EMA now requires sex-stratified data in Phase III trials. The NIH invested $12.5 million in a new research center focused on sex differences in medicine.Startups like Adyn and Womb Society are building drugs specifically for women’s biology. Investors poured $1.4 billion into femtech in 2023. The market for women’s health drugs is growing at nearly 9% a year.
But here’s the catch: these efforts still represent less than 0.5% of total pharmaceutical R&D spending. Most drug companies still treat women as an afterthought.
What You Can Do
If you’re a woman taking medication:- Ask your doctor: “Was this dose tested on women?”
- Track your side effects. Write down when they happen, how bad they are, and if they line up with your cycle.
- Don’t assume a higher dose means better results. Sometimes, less is safer.
- If you’re on zolpidem, antidepressants, or heart meds - ask if a lower dose might help.
If you’re a caregiver or partner: notice if the woman in your life seems unusually tired, dizzy, or nauseous after starting a new drug. That’s not normal - it’s a signal.
The Future Is Personalized Dosing
Researchers at UC are testing AI models that predict the right dose based on sex, weight, age, and hormones. Early results show a 40% drop in side effects when dosing is adjusted for sex.That’s the goal: not one-size-fits-all, but one-size-fits-you.
The system isn’t broken because women are different. It’s broken because medicine hasn’t caught up to the fact that women aren’t just smaller men. They’re different - and their health deserves better.
Why do women have more side effects from the same medication dose as men?
Women have different body composition, hormone levels, and enzyme activity than men. On average, women have 40% less of the liver enzyme CYP3A4, which breaks down half of all prescription drugs. They also have higher body fat percentages, which affects how fat-soluble drugs are stored and released. Their kidneys clear some drugs 20-25% slower. These biological differences mean the same dose can lead to higher drug levels and more side effects in women.
Which medications are known to affect women differently?
Zolpidem (Ambien) is the most well-known - the FDA cut the recommended dose for women by half in 2013 because they metabolize it 50% slower. Other examples include digoxin (higher toxicity risk in women), SSRIs like sertraline (more nausea and dizziness), antipsychotics like haloperidol (higher risk of heart rhythm issues), and antibiotics like sulfamethoxazole (higher risk of severe skin reactions). At least 86 FDA-approved drugs have documented sex-based differences in metabolism or side effects.
Are drug labels updated to reflect sex differences?
Very rarely. Only 4% of drug labels in the U.S. contain sex-specific dosing information. Even when studies prove differences - like with zolpidem - it can take over a decade for labels to change. Out of 200 commonly prescribed medications, only 15 have any sex-based dosing guidance. Most labels still use the same dose for everyone, regardless of sex.
Why weren’t women included in early drug trials?
In the 1970s, the FDA recommended excluding women of childbearing potential from early clinical trials to protect potential fetuses from unknown risks. This policy created a decades-long gap in data. Even after the 1993 NIH Revitalization Act required inclusion of women, many studies still didn’t analyze results by sex. As a result, dosing guidelines were built on male physiology - and that standard persists today.
Is it true that women report side effects more often than men?
Yes, but that doesn’t mean the biological differences aren’t real. Studies show women are more likely to notice, report, and seek help for side effects. They also take 56% more prescriptions on average. When researchers account for this higher usage and reporting rate, the gap in side effect rates shrinks - but doesn’t disappear. Biology and behavior both play roles.
What’s being done to fix this problem?
The FDA’s 2023 Sex and Gender Roadmap aims to integrate sex considerations into all drug reviews by 2026. The European Medicines Agency now requires sex-stratified data in late-stage trials. The NIH has invested $12.5 million in a new research center focused on sex differences in medicine. AI models are being developed to predict sex-specific doses. But progress is slow - only 32% of cardiovascular drug trials currently analyze results by sex, and most drug companies still treat women as an afterthought.
Should women always take lower doses of medication?
Not always - but they should ask. Lower doses may be safer for some drugs like zolpidem, statins, or SSRIs, but not all. The key is personalized care. If you’re experiencing side effects, talk to your doctor. Don’t assume the standard dose is right for you. Ask if your sex, weight, or hormones might affect how the drug works. Your body isn’t a one-size-fits-all model.



Joseph Townsend
17 November 2025 - 23:29 PM
Okay but let’s be real - if we started dosing everything based on sex, next thing you know we’ll be giving men different insulin because they ‘have more muscle’ or women different coffee because they ‘have slower metabolisms.’ This is slippery slope nonsense wrapped in lab coats.
Also, why are we still pretending women are this fragile biological mystery? I’ve seen women lift heavier than me at the gym and run marathons while on their period. If they can handle that, they can handle a damn pill.
Stop infantilizing half the population. Just fix the damn system instead of making it more complicated.
Shannon Hale
18 November 2025 - 16:55 PM
Y’all are missing the point. This isn’t about ‘women being weak’ or ‘men being tough.’ It’s about 50 years of medical research pretending women are just tiny men with extra parts.
I’ve been on SSRIs since 2018. My doctor gave me the same dose as my brother. I was nauseous 24/7. He felt fine. I asked if it was the dose. He laughed and said ‘maybe you’re just sensitive.’
Turns out? My body processes sertraline slower. I dropped to half the dose. My life changed. Why did it take me five years to find this out? Because no one told me. Because the label didn’t say. Because medicine still thinks ‘average patient’ means ‘male.’
It’s not about feminism. It’s about science. And science is late to the party.
Bill Machi
19 November 2025 - 10:06 AM
Another woke medical agenda. You people act like men’s bodies are the problem, not the standard. The FDA didn’t exclude women to be sexist - they did it because of fetal safety. That’s not misogyny, that’s precaution.
And now you want to re-engineer every drug in existence because some women report side effects? What’s next? Different aspirin for left-handed people?
Also, women take more prescriptions because they’re more likely to doctor-shop and over-medicate. Stop blaming the system for your own healthcare habits.
Jessica Healey
21 November 2025 - 09:29 AM
OMG I’m literally crying. I took Ambien for 3 years thinking I was just ‘a heavy sleeper’ - turns out I was almost crashing my car at 7am because the dose was designed for MEN.
I had to beg my doctor to lower it. He said ‘you’re just sensitive.’ I almost died from a fall trying to get to the bathroom at 4am.
This isn’t theory. This is my life. And I’m not the only one.
saurabh lamba
21 November 2025 - 20:21 PM
Interesting... but isn't this just another example of how modern medicine is losing its way? We are reducing human complexity to binary sex differences... while ignoring the real issue: pharmaceutical companies care about profit, not people.
Why not just test drugs on actual humans instead of pretending biology is a checkbox? :/
Also, I heard in Japan they use lower doses for everyone. Maybe we should just go smaller, not gender-specific. 🤔
Holli Yancey
22 November 2025 - 00:21 AM
I’ve been reading this thread and I just want to say - thank you to everyone sharing their stories. I didn’t realize how many of us have been silently suffering because the system was built on outdated assumptions.
My mom had to stop her heart medication because of dizziness. No one ever told her it might be her sex. She just thought she was ‘getting old.’
Maybe the real solution isn’t just changing doses - it’s changing how doctors are trained. We need to teach them that ‘normal’ isn’t male.
Levi Hobbs
23 November 2025 - 12:16 PM
Just chiming in - I’m a nurse and I see this every day. Women come in saying ‘I feel off’ and we dismiss it as anxiety or stress. Then we find out they’re on a drug that’s not dosed for them.
It’s not that we’re bad people - it’s that we’re taught to follow the label. The label doesn’t say ‘adjust for sex.’ So we don’t.
Change needs to come from the top. Not from patients begging for better care.
Kiran Mandavkar
25 November 2025 - 12:05 PM
How quaint. You think biology is a social construct? You’re mistaking correlation for causation. Women take more meds because they’re more neurotic, not because their liver enzymes are inferior.
And if you want to fix this, stop lobbying for gendered medicine - start lobbying for universal health literacy. People need to stop self-diagnosing and blaming Big Pharma for their poor lifestyle choices.
Also, why are we still using 1970s data? Because the science hasn’t changed. The narrative has. That’s the real problem.
Eric Healy
25 November 2025 - 12:10 PM
So let me get this straight - women have more side effects because they’re biologically different AND they report more? So which is it? The science or the noise?
Also, if you’re gonna say ‘dose for sex’ then why not dose for weight? Age? Ethnicity? Blood type? Why stop at XX vs XY?
And where’s the data on nonbinary people? Oh right - because they don’t exist in your binary worldview.
Fix the system? Or fix the narrative?
henry mariono
26 November 2025 - 15:14 PM
I just want to say - I appreciate this thread. My sister had to stop her antidepressant because she couldn’t function. She didn’t know it was the dose. She thought she was broken.
She’s fine now on half the dose. No one ever told her to ask.
Maybe the real issue isn’t the science. It’s that we don’t teach people how to advocate for themselves in the system.
Joseph Townsend
26 November 2025 - 18:34 PM
Wow. So now we’re doing personalized dosing by sex, weight, and mood? Next you’ll be saying I need a different blood thinner because I’m a Leo.
Let’s not turn medicine into astrology with a stethoscope.
Just use the lowest effective dose for everyone. Problem solved. No labels. No gender. No nonsense.