Hyperkalemia Risk Calculator for ACE Inhibitors + Spironolactone
This tool helps you understand your individual risk of developing hyperkalemia (high potassium) when taking ACE inhibitors with spironolactone. Enter your information below to get personalized risk assessment and monitoring guidance.
Risk Assessment
Your Personalized Risk Assessment
Key Risk Factors
Recommended Monitoring Schedule
| When | Test Type | Frequency |
|---|---|---|
| Before starting | Potassium and creatinine | Once |
| Initial phase | Potassium | |
| Stable condition | Potassium |
Next Steps
Combining ACE inhibitors with spironolactone can save lives - but it can also put you at serious risk. This isn’t theoretical. Every year, thousands of heart failure patients are prescribed this combo because it cuts death risk by up to 30%. But for every life saved, another might end up in the ER with dangerously high potassium - a condition called hyperkalemia. And it doesn’t always show symptoms until it’s too late.
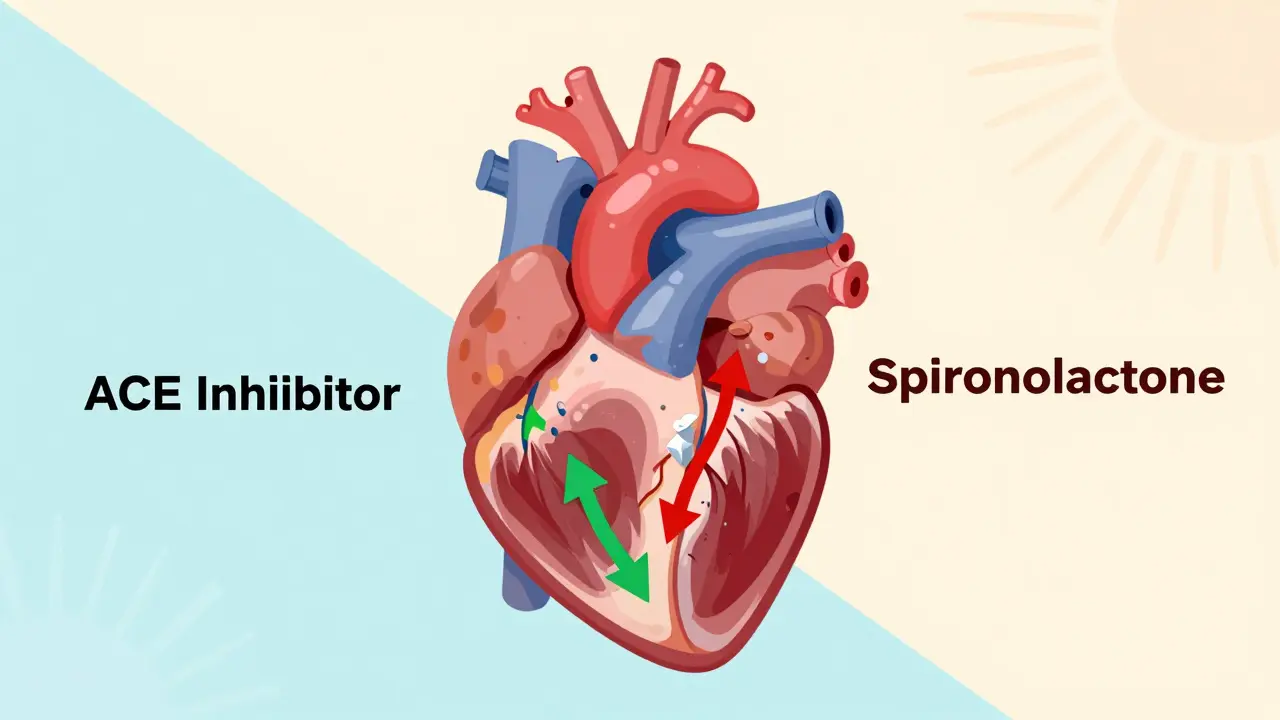
Why This Combo Works - and Why It’s Dangerous
ACE inhibitors lower blood pressure and ease heart strain by blocking a hormone called angiotensin II. That helps the kidneys get rid of salt and water. But they also reduce aldosterone, a hormone that tells your body to flush out potassium. Less aldosterone means more potassium stays in your blood.
Spironolactone does something similar - but even more directly. It blocks aldosterone receptors, so your kidneys can’t reabsorb potassium the way they normally would. When you take both drugs together, you’re hitting potassium regulation from two angles. The result? Potassium builds up faster and higher than with either drug alone.
This isn’t just a lab curiosity. The landmark RALES trial in 1999 showed that adding spironolactone to standard heart failure treatment reduced death risk by 30%. But it also showed that 13.5% of patients on spironolactone developed hyperkalemia (potassium above 5.0 mmol/L), compared to just 5% on placebo. And those numbers were from a tightly controlled trial. In real life, the risk is even higher.
Who’s Most at Risk?
If you’re on this combo, you’re not equally at risk. Some people are far more likely to develop dangerous potassium spikes. The biggest red flags:
- Age over 70 - Your kidneys don’t filter as well, and your body holds onto potassium longer.
- Chronic kidney disease - If your eGFR is below 60 mL/min/1.73m², your risk jumps 3.2 times compared to someone with healthy kidneys.
- Diabetes - High blood sugar damages kidney filters, making it harder to excrete potassium.
- Baseline potassium already above 5.0 mmol/L - Starting high means you’re closer to the danger zone.
- Severe heart failure (NYHA Class III or IV) - Your body is already struggling to balance fluids and electrolytes.
A 1996 JAMA study of 1,818 patients on ACE inhibitors alone found 11% developed hyperkalemia. Add spironolactone? That number skyrockets - especially if you have even one of those risk factors.
What Happens When Potassium Gets Too High?
High potassium doesn’t always cause symptoms. That’s the scary part. You might feel fine - until your heart starts skipping beats.
Potassium controls how your heart muscles contract. Too much, and your heart rhythm goes haywire. You could get:
- Palpitations
- Weakness or fatigue
- Numbness or tingling
- Irregular heartbeat (arrhythmia)
- Cardiac arrest (in severe cases)
Studies show that when potassium hits above 6.0 mmol/L, the risk of death spikes sharply. But here’s the twist: patients with potassium between 5.0 and 5.5 mmol/L still got the full survival benefit from spironolactone. That means stopping the drug just because your potassium is 5.2 might be doing more harm than good.

How Doctors Monitor This Risk
There’s no magic number that says “stop now.” It’s about balance - and frequent checks.
Guidelines from the American College of Cardiology and Heart Failure Society of America say:
- Check potassium and creatinine before starting the combo.
- Test again 7 to 14 days after starting - or sooner if you’re high risk.
- Test after any dose change.
- Keep checking every 4 months if you’re stable.
For high-risk patients - like those over 70, with diabetes, or kidney trouble - doctors should check potassium in just 3 to 5 days after starting. Waiting two weeks is too long.
Also, don’t panic if your creatinine rises by 30% or your eGFR drops by 25%. That’s normal with this combo. What matters is how your potassium behaves.
What to Do If Potassium Rises
Not every high potassium reading means you need to quit spironolactone.
- 5.1-5.5 mmol/L: Don’t stop. Cut spironolactone to 12.5 mg daily. Recheck in 1-2 weeks. Many patients stay here safely for years.
- 5.6-6.0 mmol/L: Pause the combo. Recheck potassium in 3-5 days. If it drops, restart at a lower dose.
- Over 6.0 mmol/L: Stop immediately. This is an emergency. You may need IV calcium, insulin, or dialysis.
Dr. Bertram Pitt, the lead researcher of RALES, says bluntly: “Don’t automatically stop MRAs just because potassium is above 5.0.” He’s seen patients live longer with controlled, moderate hyperkalemia than those who quit the drug.
Diet and Lifestyle: Do They Help?
You’ve probably heard to cut back on bananas, potatoes, and spinach. But here’s the truth: dietary potassium restriction has very limited impact on blood levels in people on this combo. Your kidneys are the problem, not your salad.
Still, if your doctor recommends limiting potassium to under 2,000 mg per day, follow it - but don’t think it’s a fix. It’s a backup plan, not a solution.
What actually helps more? Avoiding NSAIDs (like ibuprofen), staying hydrated, and not using salt substitutes (which are often full of potassium chloride).
The Newer Alternative: Finerenone
Spironolactone costs about $4 a month. But it’s old - and risky. A newer drug, finerenone, was approved in 2021 for heart failure and diabetic kidney disease. It works like spironolactone but causes far less hyperkalemia.
In the FIDELIO-DKD trial, finerenone reduced the risk of hyperkalemia leading to drug discontinuation by 6.5% compared to spironolactone. That’s a big deal. But finerenone costs $450 a month - over 100 times more. For many, spironolactone is still the only realistic option.
Why So Few Patients Get This Life-Saving Combo
Despite clear proof it cuts death risk, only 28.5% of eligible heart failure patients in the U.S. get an MRA like spironolactone. Why? The #1 reason doctors give: “Fear of hyperkalemia.”
But the 2021 ACC Expert Consensus says it plainly: “The proven mortality benefit should not be withheld solely due to mild hyperkalemia.”
The problem isn’t the drug. It’s the fear. And the lack of monitoring.
Bottom Line: Don’t Avoid It - Manage It
This combo isn’t dangerous because it’s bad. It’s dangerous because it’s powerful. And powerful things need careful handling.
If you’re on ACE inhibitors and your doctor suggests spironolactone:
- Ask: “Am I high risk?” (Age? Kidney function? Diabetes?)
- Ask: “What’s my potassium now? When will we check again?”
- Ask: “What if my potassium goes up? Will you lower the dose or stop it?”
- Don’t skip blood tests. Even if you feel fine.
Spironolactone doesn’t kill people. Ignorance does. With smart monitoring, this combo can give you years you didn’t think you’d have. But you have to be part of the plan - not just a passive patient.
Can I take ACE inhibitors and spironolactone together safely?
Yes - but only with careful monitoring. The combination reduces death risk in heart failure by up to 30%, but it also raises potassium levels. If your kidney function is normal and you get blood tests every 4-6 weeks, the benefits usually outweigh the risks. Never start or stop this combo without your doctor’s guidance.
What are the signs of high potassium?
High potassium often causes no symptoms at first. When it does, you might feel weak, tired, nauseous, or notice your heart racing or skipping beats. But the most dangerous part? You can have life-threatening levels without feeling anything. That’s why regular blood tests are non-negotiable.
Should I stop eating bananas and potatoes if I’m on this combo?
It won’t hurt to limit high-potassium foods, but don’t rely on diet alone. Your kidneys are the main issue, not your meals. A low-potassium diet might help a little, but it won’t prevent hyperkalemia if your kidneys aren’t working well. Focus on blood tests and medication management instead.
Is there a safer alternative to spironolactone?
Yes - finerenone is a newer mineralocorticoid receptor antagonist that causes less hyperkalemia than spironolactone. It’s approved for heart failure and diabetic kidney disease. But it costs over $450 a month, while spironolactone is under $5. For most people, spironolactone remains the first choice - if monitored closely.
What if my potassium is 5.3? Do I need to stop the medication?
No. A potassium level of 5.3 mmol/L is considered mild hyperkalemia. Studies show patients on spironolactone still get the full survival benefit up to 5.5 mmol/L. Instead of stopping, your doctor should reduce the spironolactone dose to 12.5 mg daily and recheck your potassium in 1-2 weeks. Stopping the drug could cost you more than it saves.
How often should I get my blood tested on this combo?
At least once before starting, then again 7-14 days after starting. After that, every 4 months if you’re stable. If you’re over 70, have kidney disease, or diabetes, get tested every 3-5 days after starting - and after any dose change. Never go longer than 6 weeks without a check.
Can I take ibuprofen or other painkillers with this combo?
Avoid NSAIDs like ibuprofen, naproxen, or celecoxib. These drugs reduce blood flow to your kidneys, making it harder for them to remove potassium. Even short-term use can trigger dangerous spikes. Use acetaminophen (Tylenol) instead for pain relief.
Why don’t more doctors prescribe spironolactone if it saves lives?
Many doctors avoid it because they fear hyperkalemia - and they’re not wrong. But the bigger issue is lack of monitoring systems. In trials, patients get frequent blood tests. In real life, many don’t. The 2021 ACC guidelines say: don’t withhold this drug for mild high potassium - but you need a plan to catch it early. Without that plan, the risk feels too high.




Diana Alime
24 December 2025 - 13:19 PM
i just started this combo last month and my potassium is 5.3... my doctor said 'eh, youll be fine' and sent me on my way. i dont even know when my next blood test is. i feel fine but now im scared to even eat a banana. what if i die in my sleep??
Adarsh Dubey
24 December 2025 - 21:07 PM
This is one of the most balanced, clinically accurate posts I've seen on Reddit. The distinction between 'dangerous hyperkalemia' and 'manageable mild elevation' is critical. Too many clinicians panic at 5.1 and stop life-saving therapy. The RALES data is clear: the benefit persists up to 5.5 mmol/L. Monitoring > fear.
Bartholomew Henry Allen
26 December 2025 - 07:42 AM
Spironolactone is a socialist drug designed to bankrupt American families with its side effects. Why dont they just give us the new expensive one like they do in Canada? This is why healthcare is broken. No one should have to risk dying from potassium just to survive heart failure. The FDA is asleep at the wheel.
Jeffrey Frye
26 December 2025 - 22:50 PM
so like... the whole 'dont stop the med' thing is cute but have you met the average patient? they dont check labs. they dont read. they take ibuprofen like water. and then they show up in the ER with a potassium of 7.2 and a EKG that looks like a seizure. the system is set up to fail. the drug works fine. the people? not so much.
Andrea Di Candia
27 December 2025 - 00:16 AM
I love how this post doesn't just scare you but empowers you. It's not about avoiding risk-it's about partnering with your body and your doctor. I used to think potassium was just some number on a paper. Now I know it's my heart's quiet alarm system. I check my labs like clockwork. I don't take ibuprofen. I eat my veggies but I don't obsess. And I feel stronger than ever. This combo didn't save my life-it helped me live it better.
bharath vinay
27 December 2025 - 19:38 PM
They don't want you to know this but finerenone is just a patent extension scam. The real reason spironolactone is underused is because Big Pharma wants you hooked on $450 pills. The potassium risk is exaggerated by the medical-industrial complex to sell more monitors and labs. Your kidneys are fine. Stop listening to doctors and start listening to nature. Salt substitutes are poison. Eat sea salt. Your body knows.
Dan Gaytan
27 December 2025 - 23:30 PM
Thank you for writing this. I’ve been on this combo for 2 years and I was terrified at first. Now I check my labs every 4 months like clockwork. I use Tylenol. I drink water. I don’t panic over 5.2. I just breathe. This isn’t about fear-it’s about awareness. And you’ve given us the tools. 🙏❤️
Usha Sundar
28 December 2025 - 14:50 PM
My dad died from this. No one told us. No one checked. Just another statistic.
claire davies
28 December 2025 - 22:14 PM
As someone who’s lived with heart failure for a decade and has seen three different healthcare systems-from the NHS to Medicare to private insurance-I can tell you this: the real tragedy isn’t the drug. It’s the gap between knowing what works and actually doing it. In the UK, we have structured monitoring pathways. In the US? It’s a lottery. Spironolactone isn’t the villain-it’s the unsung hero. But heroes need backup plans. Regular labs. Patient education. A doctor who doesn’t treat potassium like a ticking bomb. We can do better. We just have to choose to.
Wilton Holliday
29 December 2025 - 07:04 AM
You’re not alone. I was scared too when my doc first suggested this combo. But I asked the right questions, got a plan, and now I’m thriving. Here’s what helped me: write down your next lab date on your phone. Set a reminder. Print out the dosing chart. Talk to your pharmacist. This isn’t about being perfect-it’s about being consistent. You got this. 💪❤️