Weight-Loss Drug Comparison Tool
Enter your details to find the most suitable weight-loss medication based on your needs and health profile.
Recommended Medication:
Quick Take
- Orlistat blocks about 30% of dietary fat, leading to modest weight loss.
- Phentermine works as an appetite suppressant but can raise blood pressure.
- GLP‑1 agonists like liraglutide and semaglutide produce the most consistent loss (10‑15% of body weight).
- Combination therapy (naltrexone/bupropion) tackles cravings and mood.
- Alli is the over‑the‑counter, low‑dose version of Orlistat for milder goals.
When it comes to prescription weight‑loss drugs, Orlistat is a lipase inhibitor that blocks about one‑third of dietary fat absorption. It’s been on the market for two decades and is sold under the brand name Xenial (prescription) and Alli (OTC). Below we compare Orlistat with the most common alternatives, focusing on how they work, typical results, side‑effect profiles, and who might benefit most.
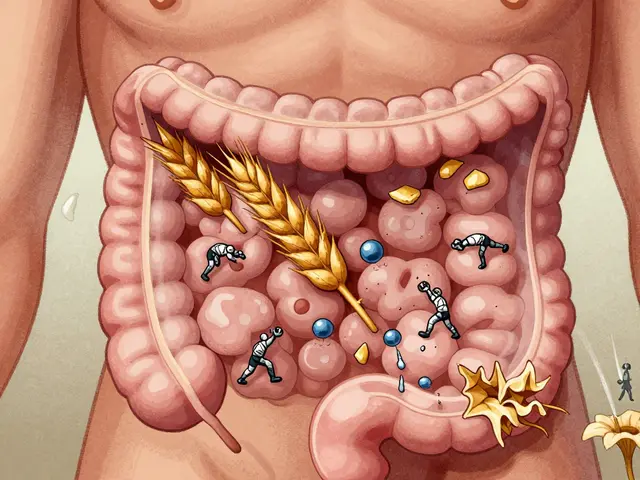
How Orlistat Works
Orlistat binds to gastric and pancreatic lipases in the stomach, preventing them from breaking down triglycerides into absorbable free fatty acids. Undigested fat passes through the intestines and is eliminated in the stool. Because it targets the fat‑calorie pathway directly, the drug doesn’t affect hunger signals or metabolism.
Orlistat is usually taken with each main meal that contains fat, at a dose of 120mg for the prescription version (Xenial) and 60mg for the OTC version (Alli). The key to success is a low‑fat diet; otherwise, users may experience oily spotting or abdominal cramping.
Prescription Alternatives at a Glance
Below are the main competitors you’ll encounter in a Canadian clinic or online pharmacy.
- Phentermine is a sympathomimetic amine that reduces appetite by stimulating the hypothalamus. It’s typically prescribed for short‑term use (up to 12 weeks) at 15‑37.5mg per day.
- Naltrexone/Bupropion (often marketed as Contrave) combines an opioid antagonist with an antidepressant to curb cravings and improve mood. The usual regimen starts at 8mg/90mg and is titrated up to 32mg/360mg daily.
- Liraglutide is a GLP‑1 receptor agonist originally developed for type‑2 diabetes. For weight loss (Saxenda), the dose climbs to 3mg subcutaneously once daily.
- Semaglutide is a newer, longer‑acting GLP‑1 agonist administered as a weekly injection (Wegovy) at 2.4mg.
- Alli is the over‑the‑counter low‑dose formulation of Orlistat (60mg) for adults with a BMI of 25‑30kg/m².
Comparing Effectiveness and Safety
| Drug | Mechanism | Typical Dose | Avg. % Body‑Weight loss | Common Side Effects | Prescription? |
|---|---|---|---|---|---|
| Orlistat | Lipase inhibition | 120mg TID (presc.) | 3‑5% | Oily stools, flatulence | Yes (Xenial) / No (Alli) |
| Phentermine | Appetite suppressant (sympathomimetic) | 15‑37.5mg daily | 5‑8% | Insomnia, tachycardia, dry mouth | Yes |
| Naltrexone/Bupropion | Opioid antagonism + norepinephrine‑dopamine reuptake inhibition | 32mg/360mg daily | 4‑6% | Nausea, headache, dizziness | Yes |
| Liraglutide | GLP‑1 receptor agonist | 3mg SC daily | 7‑8% | Nausea, vomiting, pancreatitis risk | Yes |
| Semaglutide | Long‑acting GLP‑1 receptor agonist | 2.4mg SC weekly | 10‑15% | Nausea, constipation, gallbladder disease | Yes |
| Alli | Lipase inhibition (low dose) | 60mg TID | 2‑3% | Oily spotting, abdominal cramping | No (OTC) |

Side‑Effect Profiles in Detail
Understanding the trade‑offs helps avoid surprise withdrawals. Here’s a quick rundown:
- Orlistat: Gastro‑intestinal symptoms dominate. Most are diet‑related and ease up with reduced fat intake.
- Phentermine: Cardiovascular stimulation can be problematic for people with hypertension or arrhythmias.
- Naltrexone/Bupropion: Mood changes and rare seizures mean it’s not ideal for anyone with a history of epilepsy.
- Liraglutide & Semaglutide: Nausea is common, especially during dose escalation. Both carry a boxed warning for possible thyroid C‑cell tumors (based on rodent data).
- Alli: Mirrors Orlistat’s GI side effects but at a lower intensity due to the half‑dose.
Who Should Consider Each Option?
Picking the right drug isn’t just a numbers game; personal health history matters.
- Orlistat (or Alli): Best for patients who can commit to a low‑fat diet and want a non‑systemic option without cardiovascular concerns.
- Phentermine: Suited for short‑term weight loss in otherwise healthy adults without heart disease.
- Naltrexone/Bupropion: Helpful for those who struggle with emotional eating or have a history of depression.
- Liraglutide: Ideal for individuals with obesity and pre‑diabetes, as it also improves glycemic control.
- Semaglutide: The top pick for severe obesity (BMI≥30) or when maximal weight loss is the goal, assuming the patient tolerates injectable therapy.
Practical Tips for Using Orlistat Effectively
- Take one tablet with each main meal that contains fat (up to three tablets a day).
- Spread your daily fat intake evenly across meals to avoid excess oiliness.
- Consider a daily multivitamin containing fat‑soluble vitamins (A, D, E, K) taken at a different time to compensate for reduced absorption.
- Stay hydrated; water helps move undigested fat through the GI tract.
- Monitor weight weekly and keep a simple food diary to see the fat‑calorie impact.
Next Steps: From Decision to Prescription
If you’ve identified a candidate drug, schedule a consultation with a family physician or a licensed weight‑management clinic. Bring your BMI, recent labs (lipid panel, liver enzymes), and a list of current medications-some drugs, like warfarin, can interact with Orlistat’s fat‑soluble vitamin absorption.
For those leaning toward a GLP‑1 agonist, ask about insurance coverage; many provincial plans now subsidize semaglutide for qualifying patients.
Finally, remember that medication works best alongside lifestyle changes: regular exercise, mindful eating, and sleep hygiene.
Frequently Asked Questions
Can I take Orlistat and a high‑fat diet together?
Orlistat works by blocking fat absorption, so a high‑fat diet will just increase the amount of fat passed in the stool, leading to more gastrointestinal discomfort without extra weight‑loss benefit. A moderate‑fat diet (about 30g per meal) gives the best balance.
Is Orlistat safe for people with diabetes?
Yes, it’s considered safe because it isn’t absorbed into the bloodstream. However, patients should watch blood‑sugar levels, as reduced fat intake can affect insulin dosing.
How quickly will I see results with Orlistat?
Most users notice a 1-2kg loss after the first month if they stick to a low‑fat diet. Full results (3‑5% of body weight) typically appear after 12‑16 weeks.
Can I combine Orlistat with a GLP‑1 agonist?
There’s no known pharmacologic interaction, but using both can be redundant. GLP‑1 agonists already reduce appetite and improve metabolism, so adding Orlistat offers little extra benefit while increasing GI side effects.
What should I do if I experience oily spotting?
Reduce the amount of dietary fat in the offending meal, and consider taking the dose with a lower‑fat snack. If the problem persists, talk to your pharmacist about switching to a lower dose or a different agent.





Alan Whittaker
29 September 2025 - 22:43 PM
From a macro‑pharmaceutical meta‑analysis standpoint, the proliferation of GLP‑1 agonists is less about metabolic science and more about a coordinated market‑share hijack orchestrated by the “Big Fat” consortium. Their patented lipase‑inhibition patents for Orlistat were quietly shelved in favor of injectable revenue streams, while regulatory bodies turned a blind eye under the guise of “public health”. The data you see in the tables is filtered through algorithmic bias, deliberately suppressing the modest yet sustainable outcomes that Orlistat delivers when paired with disciplined dietary adherence. In short, the narrative you’re fed is a controlled variable in a larger profit equation.
Michael Waddington
2 October 2025 - 11:38 AM
Look, the numbers don’t lie – Orlistat chops off about 3‑5% of body weight in a solid three months, which is respectable if you’re cool with cutting fat and handling the occasional oily after‑taste. The GLP‑1 drugs might give you double‑digit loss, but they also come with injection hassle and pricey insurance hoops. If you’re just starting out, the OTC Alli is a decent low‑risk entry point, just keep your meals light on the butter.
HAMZA JAAN
5 October 2025 - 00:33 AM
Honestly, tossing a prescription pill at your waistline feels like a quick‑fix romance that inevitably ends in heartbreak, especially when the side‑effects act up like an unwanted plot twist. The drama around semaglutide’s weight‑loss miracles has everyone glued to the hype, yet many forget the underlying cardiovascular risks lurking in the shadows. If you’re looking for a steady, low‑drama solution, Orlistat’s GI quirks are predictable, even if they’re a bit… messy.
April Rios
7 October 2025 - 13:29 PM
Weight loss, in essence, is an existential negotiation between the self’s aspirations and the body’s biochemical constraints; thus, each pharmacologic agent serves as a symbolic contract. Orlistat represents a pact grounded in external limitation-blocking exogenous lipids-while GLP‑1 agonists embody an internal re‑calibration of appetite pathways. The choice, therefore, is not merely clinical but a reflection of one’s willingness to confront the external versus internal determinants of desire.
byron thierry
10 October 2025 - 02:24 AM
From a cross‑cultural health perspective, the variance in drug adoption reflects differing societal attitudes toward medical intervention. In regions where injectable therapies enjoy higher acceptance, patients gravitate toward semaglutide, whereas nations with strong over‑the‑counter markets see broader use of Alli. This underscores the importance of aligning prescribing practices with local patient preferences while maintaining rigorous safety standards.
bob zika
12 October 2025 - 15:19 PM
Indeed, the epidemiological data, spanning multiple cohorts, illuminates a clear correlation-patients, when offered a choice that respects cultural proclivities, demonstrate improved adherence; consequently, therapeutic outcomes, particularly in weight‑reduction metrics, are markedly enhanced, suggesting that cultural competence, alongside pharmacologic efficacy, constitutes a pivotal axis of treatment success.
Aditya Satria
15 October 2025 - 04:15 AM
Let’s keep it simple: if you stick to a modest‑fat diet and take Orlistat as directed, you’ll likely shed those stubborn pounds without the need for injections. It’s a straightforward, cost‑effective option that works hand‑in‑hand with disciplined eating habits.
Joanne Myers
17 October 2025 - 17:10 PM
That concise approach is both practical and encouraging.
Oscar Brown
20 October 2025 - 06:06 AM
The philosophical underpinnings of pharmacologically induced weight loss demand a rigorous epistemological inquiry. When one juxtaposes the mechanistic inhibition of lipase by Orlistat with the receptor-mediated appetite modulation of GLP‑1 agonists, a dichotomy emerges between external caloric blockade and internal neurohormonal recalibration. This dichotomy is not merely a clinical consideration but a metaphysical debate about agency and corporeal autonomy. Orlistat, by preventing the hydrolysis of triglycerides, offers a tangible, observable effect that manifests in the form of steatorrhea, a phenomenon that, while inconvenient, provides immediate feedback to the patient. In contrast, semaglutide’s delayed weight‑loss trajectory, mediated through satiety signals, operates covertly within the hypothalamic circuitry, rendering its efficacy less perceptible to the lay observer. The linguistic framing of “fat‑blocking” versus “appetite‑suppressing” influences patient perception, often biasing expectations toward rapid, albeit superficial, results. Moreover, the socioeconomic stratification of drug access further complicates this discourse, as injectable therapies impose financial barriers that oral agents like Orlistat largely circumvent. Yet, one must not overlook the gastrointestinal sequelae associated with chronic lipase inhibition, which, if unmanaged, can precipitate nutritional deficiencies, particularly in fat‑soluble vitamins A, D, E, and K. Comprehensive supplementation protocols, therefore, constitute an essential adjunct to Orlistat therapy, reinforcing the need for holistic patient education. Conversely, the risk profile of GLP‑1 analogues encompasses concerns ranging from pancreatitis to potential thyroid neoplasia, underscoring the necessity for vigilant monitoring. From a statistical standpoint, meta‑analyses reveal average weight losses of 3‑5% for Orlistat versus 10‑15% for semaglutide, a disparity that is both clinically significant and ethically salient. However, the magnitude of weight loss alone should not dictate therapeutic choice; patient preference, comorbid conditions, and lifestyle compatibility remain paramount. In essence, the clinician acts as a mediator, translating complex pharmacodynamics into individualized treatment plans that honor both scientific evidence and patient autonomy. This mediatory role is amplified in multidisciplinary settings where dietitians, endocrinologists, and behavioral therapists collaborate to optimize outcomes. Ultimately, the decision matrix reflects a synthesis of efficacy, safety, cost, and personal values, each component worthy of deliberate contemplation before committing to a particular pharmacologic pathway.
Tommy Mains
22 October 2025 - 19:01 PM
If you’re new to weight‑loss meds, start by checking your BMI and any heart issues, then talk to your doctor about whether a low‑fat diet plus Orlistat could work for you before moving to stronger injections.
Alex Feseto
25 October 2025 - 07:56 AM
While your pragmatic recommendation holds merit for the lay populace, it neglects the nuanced pharmacokinetic superiority of GLP‑1 agonists, which, when scrutinized through a lens of evidentiary rigor, supersede mere dietary adjuncts in engendering sustained adipose diminution.
vedant menghare
27 October 2025 - 19:52 PM
Imagine the journey of a tiny molecule navigating the digestive highway, magically sidestepping the greedy lipases like a stealthy ninja, and that’s essentially what Orlistat does-turning the kitchen into a battlefield where only the brave, low‑fat warriors triumph.
Kevin Cahuana
30 October 2025 - 08:47 AM
That vivid analogy really captures the spirit of the drug; just remember to pair it with balanced meals and a splash of patience, and the results will follow at their own pace.
Artie Alex
1 November 2025 - 21:42 PM
Don’t be fooled by poetic platitudes-Orlistat’s lipase inhibition is a double‑edged sword, delivering caloric deficit while unleashing a cascade of oily excretions that can psychologically unhinge patients, especially when the media glorifies “miracle” injections without disclosing the visceral reality of steatorrhea.