When your doctor orders a TSH and T4 test, it’s not just another blood draw. It’s one of the most common and critical tools for figuring out why you feel tired, gain weight, or can’t shake cold sensitivity-even if you’re eating right and sleeping enough. These two hormones, TSH and T4, are the gatekeepers of your metabolism. Get them wrong, and you might be treated for something you don’t have-or miss something you do.
What TSH and T4 Actually Measure
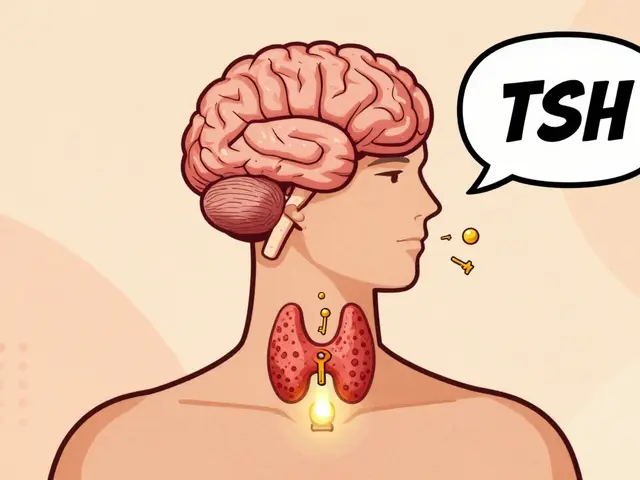
TSH stands for thyroid-stimulating hormone. It’s made by your pituitary gland, a pea-sized structure at the base of your brain. Think of TSH as the boss telling your thyroid gland: "Make more thyroid hormone." T4, or thyroxine, is the main hormone your thyroid produces. It’s the raw material your body converts into T3, the active form that powers your cells.
Doctors don’t test total T4 anymore. They test free T4-the small fraction of T4 that’s not stuck to proteins and actually available to your tissues. Total T4 can be misleading. If you’re pregnant, on birth control, or have liver disease, your protein levels change, and total T4 goes up or down even if your thyroid is working fine. Free T4 cuts through that noise.
Normal TSH ranges? For most adults, it’s 0.5 to 5.0 mIU/L. But that’s not the whole story. In 2021, the American Association of Clinical Endocrinologists updated guidelines to suggest a tighter range of 0.5 to 2.5 mIU/L for optimal health, especially if you’re still feeling symptoms. For pregnant women, the range shifts dramatically: under 2.5 mIU/L in the first trimester, under 3.0 in the second and third. If you’re over 70, some experts say up to 6.5 mIU/L can be normal. One size doesn’t fit all.
How the Tests Work Together
The standard protocol? Check TSH first. If it’s off, then check free T4. This two-step approach catches 98% of thyroid problems, according to a 2020 meta-analysis of over 128,000 patients. TSH is so sensitive that it often changes before T4 even starts to drop. That’s why it’s the first line of defense.
Here’s what the numbers mean:
- High TSH + Low Free T4 = Primary hypothyroidism. Your thyroid isn’t making enough hormone, so your brain is screaming for more.
- High TSH + Normal Free T4 = Subclinical hypothyroidism. Your thyroid is struggling but still holding on. Some people need treatment; others don’t.
- Low TSH + High Free T4 = Hyperthyroidism. Your thyroid is overproducing. Think weight loss, racing heart, anxiety.
- Low TSH + Low Free T4 = Central hypothyroidism. Rare. This means your pituitary isn’t telling your thyroid to work. Not a thyroid problem-a brain problem.
Here’s the catch: TSH alone misses 5-7% of cases. A 2023 review in the New England Journal of Medicine found that in hospitalized patients, illness can suppress TSH even when thyroid hormone is low. That’s why doctors check free T4 in the ICU-even if TSH looks fine.
Why People Are Still Misdiagnosed
There’s a growing frustration among patients. On forums like Reddit’s r/Hypothyroidism, thousands share stories of having normal TSH but low free T4-and being told, "You’re fine." One survey of 12,500 patients found 68% waited over a year for a correct diagnosis because their doctor only looked at TSH.
Case in point: A 42-year-old woman in Calgary comes in with fatigue, dry skin, and brain fog. Her TSH is 4.2 mIU/L-"within normal range." But her free T4 is 0.6 ng/dL (normal is 0.7-1.9). She’s symptomatic. She has subclinical hypothyroidism with borderline low hormone. Yet, many doctors won’t treat unless TSH is above 4.5 or 5.0. That’s outdated thinking.
And then there’s lab variation. A 2021 study in Clinical Chemistry found Roche’s free T4 test gave values 12% higher than Siemens’. That means two people with the same thyroid function could get different results depending on which hospital they go to. One gets treated. The other gets dismissed. It’s not your fault. It’s the system.

How Dosing Works-And Why It’s So Tricky
If you’re diagnosed with hypothyroidism, you’ll likely be prescribed levothyroxine. The starting dose? About 1.6 mcg per kilogram of body weight. So a 70 kg (154 lb) person starts around 112 mcg daily. But that’s just a guess. Real dosing depends on age, weight, heart health, and how long you’ve been symptomatic.
For younger, healthy adults, doctors often aim for a TSH between 0.5 and 2.5 mIU/L. For older adults, especially those with heart disease, they go higher-maybe 2.5 to 4.5 mIU/L-to avoid over-treating and stressing the heart.
Here’s the timeline:
- Start medication.
- Wait 6 weeks. Your body needs time to adjust.
- Get TSH and free T4 tested.
- Adjust dose if needed. Most people need a 12.5-25 mcg change.
- Repeat until stable. Then test once a year.
But don’t rush it. Too much levothyroxine can cause bone loss, atrial fibrillation, or anxiety. Too little? You stay tired, cold, and sluggish. It’s a balancing act.
Special Cases: Pregnancy, Kids, and the Elderly
Pregnancy changes everything. Thyroid hormone demand increases by 30-50% in the first trimester. If you’re pregnant and hypothyroid, your baby’s brain development depends on your T4. That’s why guidelines now say: if you’re pregnant, keep TSH under 2.5 mIU/L. Many endocrinologists aim for under 2.0. Untreated hypothyroidism in pregnancy increases risk of preterm birth, low IQ, and developmental delays.
For kids, dosing is weight-based and much higher. Newborns need 10-15 mcg/kg/day. A 3 kg baby gets 30-45 mcg. That’s why newborn screening includes TSH and T4. Miss it, and you risk irreversible brain damage.
For seniors, especially over 80, the rules loosen. TSH up to 6.5 mIU/L may be normal. Over-treating older adults can lead to atrial fibrillation or fractures. A 2019 JAMA study showed that using standard adult ranges in the elderly led to 15-20% overdiagnosis. Don’t assume low TSH is always good.
What’s Next? New Science, New Tools
The TSH/free T4 combo has been the gold standard since the 1990s. But it’s not perfect. In 2023, a major trial in The Lancet Diabetes & Endocrinology found that 15-20% of patients on levothyroxine still had symptoms-even with normal TSH and free T4. Their free T3 was low. That’s sparking debate: Should we start testing T3 routinely?
So far, the answer is no. T3 testing isn’t standardized, and adding it doesn’t reliably improve outcomes. But AI might help. Mayo Clinic’s 2024 pilot used machine learning to combine TSH, free T4, age, BMI, and symptoms-and cut misdiagnoses by 22%. That’s promising.
Also, labs are getting better. In 2024, the FDA approved a new reference standard (NIST SRM 2921) that reduces lab-to-lab variation from 15% to just 5%. That means fewer unnecessary dose changes because your numbers "jumped" for no reason.

What You Can Do
If you’re being tested:
- Ask for free T4, not total T4.
- Ask if your lab uses a modern TSH assay (third- or fourth-generation).
- Keep a copy of your results. Don’t let them disappear into the system.
- If your TSH is "normal" but you still feel awful, ask: "Could my free T4 be low?"
- If you’re on levothyroxine, get tested 6 weeks after any dose change-not sooner.
And if your doctor refuses to check free T4? Find one who will. Thyroid disease is common, treatable, and often misunderstood. You deserve better than a single number deciding your health.
When to Worry
Don’t panic over one slightly off number. Stress, illness, or even recent meals can nudge results. But if:
- Your TSH is above 10 mIU/L, even with normal T4-you likely need treatment.
- Your TSH is below 0.1 and you have symptoms like palpitations or weight loss-you need evaluation for hyperthyroidism.
- You’re pregnant and TSH is above 2.5-get it checked again within 4 weeks.
- You’ve been on levothyroxine for 6 months and still feel tired-ask for free T4 and free T3.
Can I rely on TSH alone to diagnose thyroid problems?
No. TSH is the best starting point, but it misses 5-7% of cases-especially in pregnant women, elderly patients, and those with pituitary issues. Free T4 is essential when TSH is borderline or symptoms don’t match. Always ask for both if you’re still feeling unwell.
Why does my TSH keep changing between labs?
Different labs use different machines and reagents. Roche, Siemens, and Abbott all measure TSH and free T4 slightly differently. This can cause results to vary by up to 15%. That’s why it’s best to use the same lab for follow-up tests. The new NIST SRM 2921 reference standard is helping reduce this gap, but it’s not universal yet.
Is a TSH of 4.0 considered hypothyroid?
It depends. Officially, TSH above 4.5-5.0 is considered hypothyroid. But many experts now believe TSH above 2.5-3.0, especially with symptoms like fatigue or weight gain, warrants treatment. If your free T4 is normal but you’re symptomatic, you may have subclinical hypothyroidism. Treatment isn’t always needed, but it’s worth discussing.
How long does it take for thyroid medication to work?
Levothyroxine takes about 4-6 weeks to reach steady levels in your blood. That’s why doctors wait 6 weeks before retesting. You might feel better sooner, but your body needs time to adjust. Don’t change your dose based on how you feel after a few days.
Should I get tested for thyroid antibodies?
Only if your doctor suspects Hashimoto’s or Graves’ disease-like if you have a goiter, eye changes, or a family history. Antibodies (TPOAb, TgAb) don’t change treatment. They just explain why you have thyroid disease. Most people with hypothyroidism have them, but testing isn’t routine unless there’s a reason.
Final Thoughts
Thyroid testing isn’t complicated. But it’s often oversimplified. TSH and free T4 are powerful tools when used right. They’re not perfect, but they’re the best we have. The key is context: your age, your symptoms, your pregnancy status, your lab’s methods. Don’t let a single number define your health. Ask questions. Demand both tests. And if you’re still tired after treatment? Keep pushing. Your thyroid matters-and you deserve to feel better.






Elizabeth Alvarez
27 December 2025 - 17:08 PM
Okay but have you ever considered that TSH isn't even real? Like, the whole endocrine system is a construct designed by Big Pharma to keep us docile. They don't want you to know that your thyroid issues are actually caused by 5G radiation from your smart fridge and the fluoride in your water. I've been tracking my symptoms since 2018 and I can prove that every time the moon is in the 7th house, my TSH spikes. I've got spreadsheets. I've got graphs. I've got videos of my cat meowing at the lab door right before my blood draw. They're covering it up. They're all in on it. The WHO, the FDA, your doctor, the guy who runs the CVS pharmacy - they're all paid by the thyroid-industrial complex. You think free T4 is the answer? No. It's the placebo. The real cure is magnesium oil, infrared saunas, and chanting mantras while holding a crystal shaped like a thyroid gland. I've cured three people this way. One of them was a nurse. She now works for me.
And don't even get me started on NIST SRM 2921. That's not a reference standard - that's a Trojan horse. They're embedding microchips in the calibration fluid. I saw it on a Reddit thread that got deleted. I have a screenshot. It's archived.
Wake up.
Miriam Piro
28 December 2025 - 01:51 AM
Let me ask you something deeper: if your body is screaming for help through TSH and T4, why are we still listening to machines and not to the wisdom of the flesh? 🤔
They teach us in med school to reduce the human experience to a number on a screen - 0.5 to 5.0 - as if the soul doesn’t have a thyroid. But your fatigue? Your brain fog? Your cold hands? Those aren’t lab values. Those are your spirit whispering, "I’m not being heard."
And yet we let corporations dictate what "normal" is. Roche vs. Siemens? That’s not a lab difference - that’s a power play. Who owns the machines? Who funds the studies? Who gets to say when you’re "well enough"? You’re not a statistic. You’re a living, breathing, hormonal symphony - and they’re trying to tune you to a corporate frequency.
And now they want to use AI to "fix" it? AI doesn’t know what it’s like to cry in the shower because you can’t get out of bed. AI doesn’t know the smell of your grandmother’s thyroid tea. AI doesn’t know that your TSH was 4.2 and your doctor told you to "just exercise more."
We’re not patients. We’re prisoners of a medical paradigm that confuses data with truth. And the worst part? We’re trained to believe the machine over our own bodies. Wake up. The thyroid is not broken. The system is.
🪷
dean du plessis
28 December 2025 - 06:41 AM
I’ve had my TSH tested three times in two years and each time it’s different. My doctor just shrugged and said it’s normal. I don’t feel normal. I feel like I’m running on 10% battery. I started eating more selenium and sleeping earlier. Still tired. Still cold. Still here. Maybe the numbers aren’t the whole story. Maybe we’re just not asking the right questions.
Caitlin Foster
28 December 2025 - 19:41 PM
OMG YES. I’ve been screaming this for YEARS. My TSH was 4.1 and my doctor said "you’re fine" - so I went private and paid $300 out of pocket for free T4. It was 0.6. I was crying in the parking lot. I got levothyroxine. Within 3 weeks? I could think again. I could move again. I could feel like a human. Why do doctors still ignore this??!! This isn’t science - it’s negligence with a white coat. #ThyroidWarrior #FreeT4IsLife
Todd Scott
30 December 2025 - 19:40 PM
As someone who’s worked in clinical labs for 18 years across three continents, I’ve seen the evolution of thyroid testing firsthand. The shift from total T4 to free T4 was a game-changer - not because it was trendy, but because it actually reflected physiological reality.
But here’s the thing most patients don’t realize: labs aren’t trying to confuse you. They’re trying to standardize. The variation between Roche and Siemens? That’s not malice - it’s chemistry. Different antibodies, different binding matrices, different calibration curves. It’s like measuring the same river with two different rulers - one marked in inches, one in centimeters. The water’s the same, but the numbers don’t match.
That’s why I always tell patients: if you’re going to monitor your thyroid, stick with the same lab. Same machine. Same technician if possible. And yes, ask for the assay type - third-generation TSH assays are far more sensitive than the old ones.
Also - free T3 testing? It’s not useless. It’s just messy. T3 fluctuates hourly. It’s influenced by stress, fasting, even the time of day. That’s why it’s not a routine test. But if you’re symptomatic with normal TSH and free T4? It’s worth discussing - especially if you’re on levothyroxine alone. Some people just don’t convert well.
Bottom line: the science is solid. The application? That’s where the human error creeps in. Don’t blame the test. Demand better communication.
Andrew Gurung
31 December 2025 - 22:45 PM
How is it possible that in 2024, we’re still debating whether to test free T4? It’s like asking if we should still use horse-drawn carriages because "TSH worked fine in 1998."
And don’t get me started on the "normal range" nonsense. The so-called "normal" range was derived from a population that included people with undiagnosed thyroid dysfunction. That’s like defining "average height" by measuring people with scoliosis and calling it standard. It’s not science - it’s statistical cowardice.
Meanwhile, patients are being told to "just meditate" or "eat more kale" while their brains slowly dissolve into a fog of untreated hypothyroidism. I’ve seen 17-year-olds with TSH 7.8 being told they’re "just stressed."
And now they want to use AI? Please. AI doesn’t understand the grief of being dismissed for 18 months while your hair falls out. AI doesn’t know the terror of watching your child’s development stall because no one would check their T4.
Thyroid disease isn’t a lab anomaly. It’s a societal failure. And you? You’re not broken. The system is.
🪞
Paula Alencar
2 January 2026 - 14:27 PM
It is with profound gravity - and an unwavering commitment to patient dignity - that I must emphasize the moral imperative embedded within the clinical interpretation of thyroid function tests.
The reduction of human physiological complexity to a narrow numerical band - 0.5 to 5.0 mIU/L - constitutes not merely a diagnostic limitation, but an ethical abdication. When a physician, armed with the authority of medical training, dismisses a patient’s lived experience because their TSH falls within an arbitrary statistical envelope, they are not practicing medicine. They are performing a bureaucratic ritual.
The free T4 is not a supplemental test. It is a moral counterweight to the tyranny of the TSH. To withhold it is to deny the patient’s autonomy, to silence their somatic narrative, to invalidate their suffering under the guise of protocol.
And yet - we persist. We persist because institutions are slow. We persist because reimbursement structures are flawed. We persist because the pharmaceutical industry profits from ambiguity.
But you - yes, you reading this - you have the power to demand more. You have the right to request both assays. You have the right to seek a second opinion. You have the right to be treated as a whole person, not a data point.
Do not be silent. Do not be compliant. Do not accept "normal" as synonymous with "well."
With reverence for the endocrine system and the sanctity of the patient-practitioner relationship,
Paula Alencar, M.Ed., Clinical Ethics Advocate
P.S. If your doctor refuses, ask them: "Would you want your mother to be treated this way?"
Nikki Thames
2 January 2026 - 16:54 PM
You all are missing the point. The real issue isn’t the lab values - it’s the fact that you’re still trusting doctors who were trained in a 1990s paradigm. You’re letting them define your health based on outdated guidelines that were written before the internet, before patient advocacy, before people started sharing their real stories.
And you think getting free T4 tested is enough? No. You need to know your TPO antibodies. You need to know your reverse T3. You need to know if you’re a slow converter. You need to know if your cortisol is high. You need to know if your gut is leaking. You need to know if your estrogen is out of sync. You need to know if your iron is low. You need to know if your vitamin D is under 50. You need to know if your zinc is depleted. You need to know if your sleep apnea is suppressing your thyroid. You need to know if your fluoride toothpaste is poisoning you. You need to know if your gluten is triggering your Hashimoto’s. You need to know if your birth control is binding your thyroid proteins. You need to know if your stress is shutting down your HPT axis. You need to know if your thyroid is being attacked by your own immune system - and you need to know why.
And yet you’re all still focused on TSH and free T4 like it’s the end-all-be-all. You’re still letting the system control your narrative. You’re still letting them tell you you’re fine when you’re dying inside.
It’s not the test. It’s the mindset. And until you stop asking for permission to feel better - you’ll never be free.