Statin Intolerance Assessment Tool
Statin Intolerance Assessment
Answer these questions to determine if you might have statin intolerance and what steps to take next.
Your Assessment Results
Your Likely Situation
Recommended Next Steps
- Consult a lipid specialist or statin intolerance clinic
- Get basic labs: thyroid function, vitamin D, CK levels, liver enzymes
- Consider a statin rechallenge with a different statin
- Explore non-statin alternatives if needed
Important Considerations
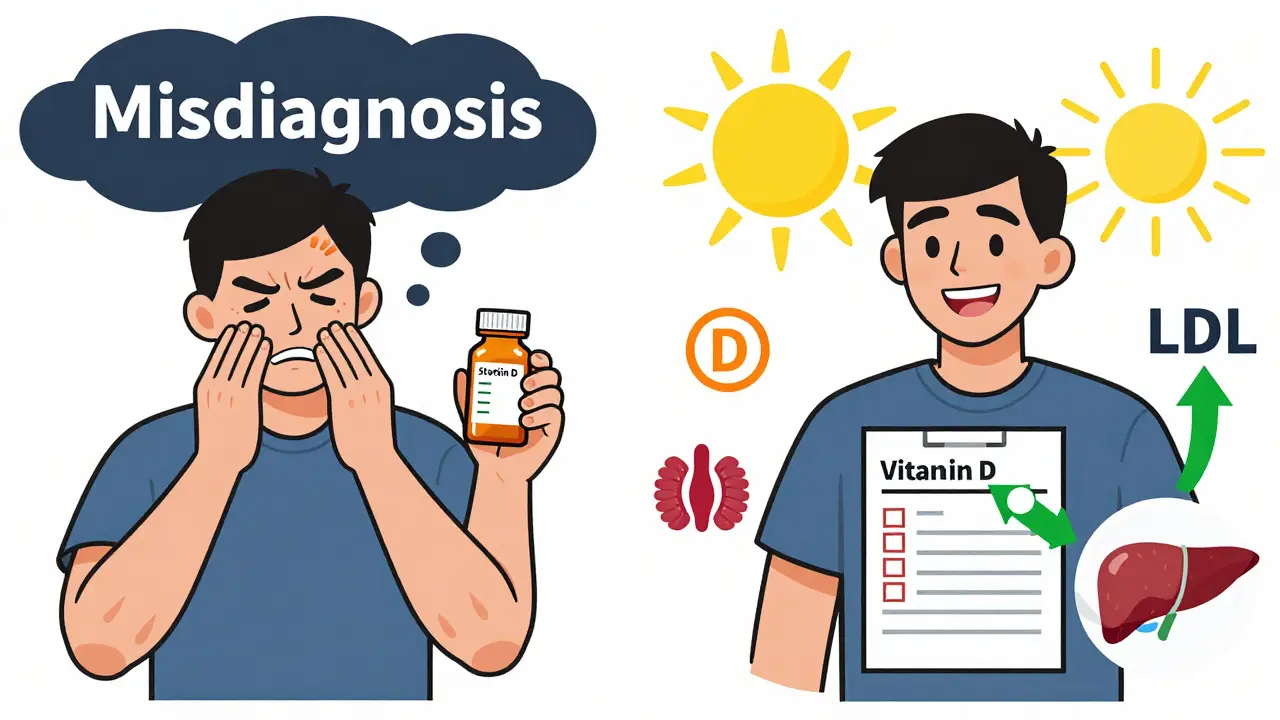
Only 15% of reported statin intolerance cases are actually caused by the statin itself. The majority (85%) are due to other factors like low vitamin D, thyroid issues, or medication interactions. Proper evaluation is crucial to avoid unnecessary discontinuation.
For millions of Americans taking statins to lower cholesterol, the drugs work exactly as planned-until they don’t. Muscle pain, weakness, or cramps start showing up. Some people blame the statin. Others are told it’s just aging. But what if the real issue isn’t the statin itself, but how it’s being handled?
Statin intolerance isn’t rare. Between 7% and 29% of people on statins report muscle symptoms. But here’s the twist: only about 5% to 15% of those cases are actually caused by the statin. The rest? Often misdiagnosed. That’s where specialized statin intolerance clinics come in. These aren’t just another doctor’s office. They’re structured, step-by-step systems designed to keep people on life-saving therapy without the side effects.
What Exactly Is Statin Intolerance?
Statin intolerance isn’t a single diagnosis. It’s a pattern. The National Lipid Association (NLA) defines it clearly: you can’t tolerate at least two different statins-one at the lowest dose, another at any dose-because of side effects. But here’s what most doctors miss: symptoms must be tied to the statin, not something else.
Think about it. Muscle aches happen for a lot of reasons: low vitamin D, thyroid problems, overtraining, even certain supplements like red yeast rice. If you stop a statin because your legs hurt, but you never check your thyroid or vitamin levels, you’re not solving the problem-you’re just avoiding it.
True statin-associated muscle symptoms (SAMS) have a clear pattern. They start 2 to 4 weeks after starting or increasing the statin. They’re symmetric-both legs, not just one. They’re in the large muscles: thighs, shoulders, back. And they go away within 2 to 4 weeks after stopping the drug. If your pain doesn’t follow that timeline, it’s probably not the statin.
The Problem with the Old Way
Traditionally, if a patient complained about muscle pain on a statin, the answer was simple: stop the statin. No rechallenge. No testing. No alternatives. Just cut it out.
That approach is broken. Studies show that 45% of patients who report statin intolerance end up stopping the drug for good. But here’s the scary part: statins reduce heart attacks and strokes by 20% to 25% for every 1 mmol/L drop in LDL cholesterol. That’s not a small benefit. That’s life or death.
When patients are permanently taken off statins without proper evaluation, they’re left with high cholesterol-and higher risk. The Cholesterol Treatment Trialists’ Collaboration analyzed data from 170,000 patients. The message was clear: lowering LDL saves lives. But if you don’t know how to handle intolerance, you’re denying people that protection.
How Statin Intolerance Clinics Work
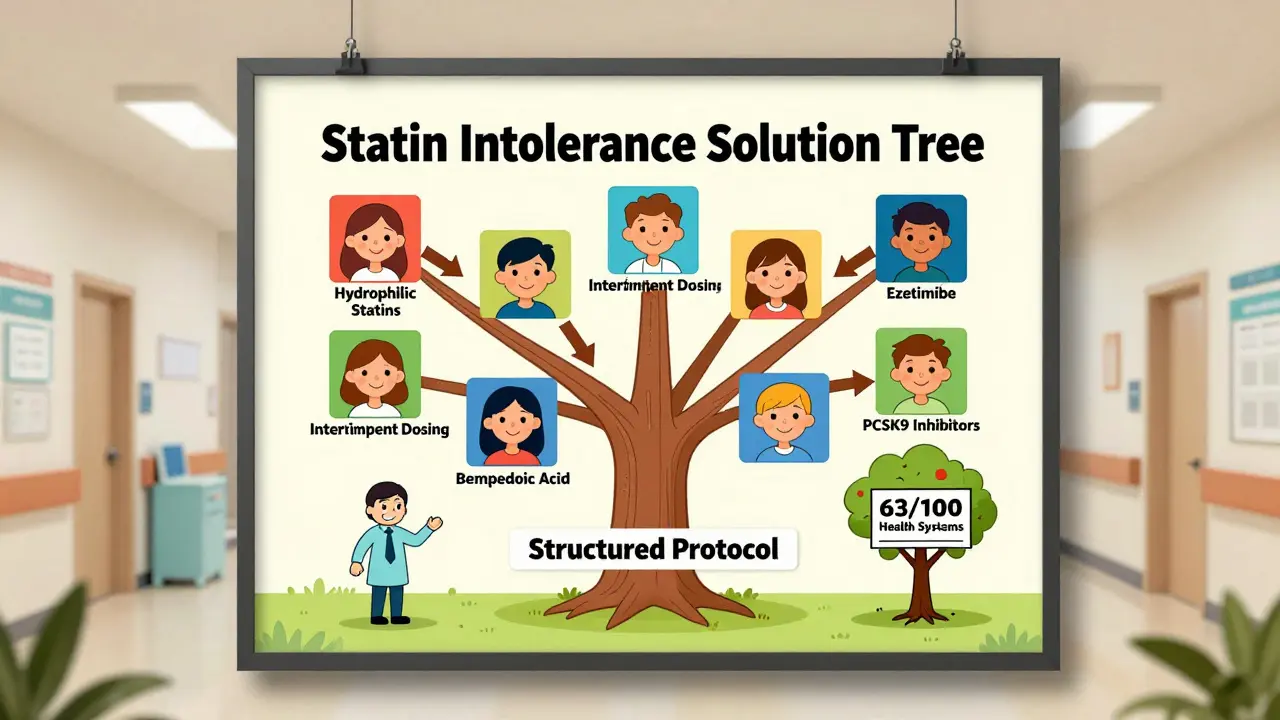
These clinics don’t guess. They follow protocols. And they’re built on four pillars: rule out other causes, rechallenge carefully, switch smartly, and add non-statin options when needed.
Step 1: Stop the statin and wait. Patients are taken off the statin for at least two weeks. Symptoms are tracked daily-location, intensity on a 0 to 10 scale, whether it worsens with activity. If the pain fades, that’s a clue.
Step 2: Check the basics. Before blaming the statin, labs are run: thyroid function, vitamin D, creatine kinase (CK), and liver enzymes. Alcohol use and drug interactions (like with fibrates or certain antibiotics) are reviewed. Many patients find out their muscle pain was from low vitamin D or an underactive thyroid-not the statin.
Step 3: Rechallenge with a different statin. This is where most clinics succeed. Instead of quitting statins entirely, patients try a different one. Hydrophilic statins like pravastatin or rosuvastatin are less likely to enter muscle tissue. Studies show switching to rosuvastatin works for 72% of people who couldn’t tolerate simvastatin or atorvastatin.
Step 4: Try intermittent dosing. For those who still react, dosing every other day or twice a week can work. Rosuvastatin, with its long half-life, is ideal for this. A Cleveland Clinic study of 1,247 patients found 76% tolerated intermittent dosing and still lowered LDL by 20% to 40%.
Step 5: Add non-statin options. If all else fails, ezetimibe (cost: $35/month) reduces LDL by about 18% and cuts heart events by 6%. Bempedoic acid (Nexletol) is newer-approved in 2020-and lowers LDL by 18% without muscle side effects. PCSK9 inhibitors like evolocumab are powerful but expensive ($5,850/year), and insurance often blocks them without multiple appeals.
What the Data Shows
Structured clinics don’t just feel better-they work better.
Kaiser Permanente’s program found 82% of patients who went through their statin intolerance protocol were able to resume some form of lipid-lowering therapy. Compare that to 45% in regular care.
Cleveland Clinic’s data shows 68% of patients hit their LDL goals using their protocol. The most successful method? Switching to a hydrophilic statin. Second? Intermittent dosing.
Even the VA system, which runs statin intolerance clinics across 170 medical centers, cut false diagnoses by 38% by forcing clinicians to rule out other causes first. That’s huge. It means fewer people are being told they can’t take statins when they actually can.
Real Patient Stories
One Reddit user, HeartPatient87, had been told he was statin intolerant for five years. He was off all cholesterol meds. His LDL hovered around 142. He joined a lipid clinic at Johns Hopkins. They switched him to rosuvastatin 5mg twice a week and added CoQ10. Within months, his LDL dropped to 89. No muscle pain. He said: “I finally feel like I’m not just surviving-I’m managing.”
Another patient on the Inspire forum spent 11 weeks fighting insurance to get access to PCSK9 inhibitors after three statins failed. She finally got approval. Her LDL went from 160 to 68. “I thought I’d be on meds forever,” she wrote. “Now I’m not scared of a heart attack.”
But not all stories are positive. Long wait times-6 to 8 weeks for an appointment-are common. Insurance denials for non-statin drugs still block 44% of high-risk patients. And some patients are too afraid to rechallenge, even when the odds are in their favor.
Who Needs This Clinic?
You might need a statin intolerance clinic if:
- You stopped a statin because of muscle pain but never tried another one
- You were told you’re “intolerant” but your symptoms started after a new medication or illness
- Your LDL is still high, and your doctor says you can’t take statins
- You’ve tried one statin and quit-without trying others
If you’ve been told you can’t take statins, you’re not alone. But you’re also not out of options. The key is structure. No guessing. No rushing. Just a clear path.
What’s Changing in 2025
The field is evolving fast. The ACC’s Statin Intolerance Tool, launched in 2023, gives doctors a checklist to follow-symptoms, labs, risk scores, alternatives-all in one place. It’s free, online, and updated quarterly.
Genetic testing is now available at places like Mayo Clinic. A variant in the SLCO1B1 gene makes some people way more likely to get muscle pain from simvastatin. If you have it, you’re better off avoiding that drug entirely.
And new treatments are coming. Nanoparticle statins, still in trials, are showing 92% tolerability in early tests. They deliver the drug straight to the liver, bypassing muscle tissue. If approved, they could change everything.
Right now, 63 of the 100 largest U.S. health systems have formal statin intolerance protocols. Academic centers lead the way-87% have them. Community hospitals? Only 42%. That gap needs to close.
What You Can Do Today
If you’re on a statin and having side effects:
- Don’t quit cold turkey. Talk to your doctor about a rechallenge plan.
- Ask for a CK test and thyroid/vitamin D check before assuming it’s the statin.
- Request a switch to rosuvastatin or pravastatin-they’re less likely to cause muscle issues.
- If you’re still having trouble, ask about ezetimibe or bempedoic acid. They’re affordable and effective.
- Seek out a lipid specialist or statin intolerance clinic. Your local hospital might not have one, but a nearby university medical center probably does.
Statin intolerance isn’t a dead end. It’s a puzzle-and there’s a method to solve it. You don’t have to live with high cholesterol because you were told you can’t take the medicine. With the right approach, you can take it safely.
Can statin intolerance be reversed?
Yes, in most cases. Many people who think they’re intolerant are misdiagnosed. Up to 80% of reported cases turn out to be caused by other factors like low vitamin D, thyroid issues, or drug interactions. Even among true cases, switching to a different statin or using intermittent dosing helps 65% to 75% of patients tolerate therapy again.
Is it safe to stop statins if I have muscle pain?
Only after ruling out other causes. Stopping statins without evaluation increases your risk of heart attack or stroke. Always consult a specialist before quitting. A two-week break to see if symptoms resolve is standard, but never assume the statin is the culprit without testing.
What’s the best statin for someone with muscle side effects?
Hydrophilic statins like rosuvastatin and pravastatin are preferred. They’re less likely to enter muscle tissue because they’re actively transported into the liver. Simvastatin and atorvastatin are lipophilic and more likely to cause muscle symptoms. Switching from one to the other often solves the problem.
How long does it take for muscle pain to go away after stopping a statin?
Typically 2 to 4 weeks. If pain persists beyond that, the cause is likely something else-like arthritis, nerve compression, or another medication. True statin-related muscle symptoms resolve quickly after stopping the drug.
Are non-statin cholesterol drugs as effective as statins?
Not as powerful, but still effective. Ezetimibe lowers LDL by about 18% and reduces heart events by 6%. Bempedoic acid lowers LDL by 18% without muscle side effects. PCSK9 inhibitors can drop LDL by 50% or more. Statins are still the gold standard for lowering risk, but these alternatives are proven and life-saving for those who can’t take statins.
Why aren’t statin intolerance clinics more common?
They require time, training, and coordination. Most primary care doctors don’t have the resources to run rechallenge protocols. Insurance barriers for non-statin drugs also discourage clinics from expanding. But adoption is growing-63 of the top 100 U.S. health systems now have formal programs, and academic centers lead the way.
Can CoQ10 help with statin muscle pain?
Some patients report relief, but studies are mixed. CoQ10 levels drop slightly on statins, and muscle cells need it for energy. While it’s not a cure, adding 100-200 mg daily is low-risk and may help in combination with other strategies like switching statins or intermittent dosing.
What’s the difference between statin intolerance and statin myopathy?
Statin intolerance is a broad term for any adverse reaction that prevents continued use. Statin myopathy is a specific muscle condition confirmed by elevated CK levels (over 10 times the upper limit) and muscle damage. Most people with intolerance don’t have myopathy-they have mild muscle pain without lab abnormalities. The diagnosis matters because treatment differs.
Statin intolerance doesn’t mean you’re out of options. It means you need a smarter approach. With the right protocol, most people can stay on therapy-and stay protected from heart disease.






Jeanette Jeffrey
27 December 2025 - 02:45 AM
Oh great, another ‘statin intolerance clinic’-because clearly the problem isn’t that we’re overmedicating everyone and ignoring lifestyle. I’ve seen 70-year-olds on 4 statins while eating fast food daily. The real solution? Stop prescribing like it’s a magic bullet and start teaching people how to eat. But sure, let’s spend $5k on PCSK9 inhibitors instead of telling someone to walk more. Classic medicine.
Shreyash Gupta
28 December 2025 - 11:23 AM
Bro… i just took rosuvastatin 5mg once a week and my legs feel like jelly 😅. Is this normal? Or am i just weak? I’ve been doing yoga and eating only rice for 3 months. Maybe i need more protein? 🤔
Ellie Stretshberry
30 December 2025 - 08:02 AM
i had muscle pain too and just stopped the statin. then my doc said check your vit d. turns out i was at 18. took supplements for 2 months and the pain went away. no statin needed. i feel like so many people dont even get tested first. just quit. easy fix but no one tells you.
Zina Constantin
31 December 2025 - 21:32 PM
Let me tell you something-I’m from a small town in Texas where the only doctor is the guy who runs the Walmart Clinic. We don’t have ‘statin intolerance clinics.’ We have ‘stop taking the blue pill’ and ‘here’s a coupon for fish oil.’ The system is broken, and it’s not the patients’ fault. If you’re going to prescribe life-saving drugs, at least give people a fighting chance to use them safely. This article? It’s a lifeline. Thank you.
Dan Alatepe
1 January 2026 - 11:32 AM
Y’all really think this is about statins? Nah. This is about Big Pharma selling pills instead of fixing the root cause-our food, our stress, our sleep. My cousin was on statins for 8 years. Then he started sleeping 8 hours, eating greens, and walking 10k steps. His LDL dropped 40 points. No meds. He’s now a ‘wellness influencer.’ The system fears this. That’s why they keep pushing pills.
Angela Spagnolo
2 January 2026 - 22:52 PM
i read this whole thing... and i cried a little. my mom was told she couldn't take statins... and she had a heart attack last year. i wish we'd known about this sooner. thank you for writing this. i'm printing it out for my dad's doctor.
Jay Ara
3 January 2026 - 00:00 AM
my doc switched me to pravastatin after simvastatin wrecked my legs. worked like magic. no more pain. ldl down. just try a different one. dont give up. also coq10 helped a bit. not magic but no harm.
Kuldipsinh Rathod
4 January 2026 - 22:14 PM
my brother took rosuvastatin every other day and it worked fine. he was scared at first but now he says it's the best thing he ever did. no pain no problem. just ask your doc about intermittent dosing. it's a game changer.
SHAKTI BHARDWAJ
6 January 2026 - 13:31 PM
THIS IS A SCAM. THEY WANT YOU TO STAY ON DRUGS FOREVER. WHY NOT JUST EAT LESS MEAT AND DO YOGA? I SAW A VIDEO WHERE A MAN GOT HIS LDL TO 70 WITH JUST OATS AND WALKING. NO PILLS. NO CLINICS. JUST COMMON SENSE. THEY MAKE MONEY OFF YOUR FEAR. DON'T BE A SHEEP.
david jackson
8 January 2026 - 13:29 PM
Okay, let’s break this down. Statins reduce heart attacks by 20–25% per 1 mmol/L drop in LDL. That’s not ‘kinda helpful.’ That’s ‘you live longer or you die sooner.’ And yet, we’ve got doctors who stop statins at the first mention of muscle pain without checking thyroid, vitamin D, CK, drug interactions, or even alcohol use. We’re not just misdiagnosing-we’re actively endangering people. And then we wonder why heart disease is still the #1 killer. This isn’t about statins. It’s about lazy medicine. And clinics like these? They’re the antidote. I’m so tired of people treating complex biology like it’s a TikTok trend.
wendy parrales fong
8 January 2026 - 20:10 PM
i never knew you could take statins every other day. i thought if you missed a day you were just wasting it. i tried it after reading this and my legs feel normal. my ldl is still down. it’s like magic. i feel so much better. thank you for sharing this.
carissa projo
10 January 2026 - 19:57 PM
There’s something deeply human here. We’re not just talking about cholesterol-we’re talking about fear. Fear of dying. Fear of being told you’re broken. Fear of being abandoned by your doctor. These clinics don’t just test labs-they restore dignity. The woman who waited 11 weeks for PCSK9 approval? That’s not healthcare. That’s a bureaucracy that treats life like a spreadsheet. But when she got her treatment? She didn’t just lower her LDL. She lowered her fear. And that’s worth more than any number.
josue robert figueroa salazar
10 January 2026 - 22:37 PM
statins are overprescribed. period. if you're 40 and your ldl is 140? you don't need a pill. you need a new diet. stop eating donuts and start walking. clinics like this just keep the machine running.
Jody Kennedy
11 January 2026 - 16:52 PM
OMG I just found out my muscle pain was from my thyroid-NOT the statin! I’ve been off meds for 2 years and my doctor never checked it. I’m going back to rosuvastatin next week. This changed my life. Thank you for posting this!
christian ebongue
11 January 2026 - 17:51 PM
so u just switch statins? wow. i thought i was doomed. i'll try rosuvastatin. thanks for the tip. no more leg pain hopefully lol