When you’re 70, a pill that once helped you sleep through the night might leave you dizzy, confused, and on the floor. That’s not just bad luck-it’s biology. As we age, our bodies change in ways that make medications behave differently, often turning helpful treatments into dangerous ones. The same dose that worked perfectly at 50 can cause serious harm by 75. This isn’t rare. Age is one of the biggest risk factors for bad reactions to medicines, and it’s happening to millions of people right now.
Why Older Bodies Handle Medicines Differently
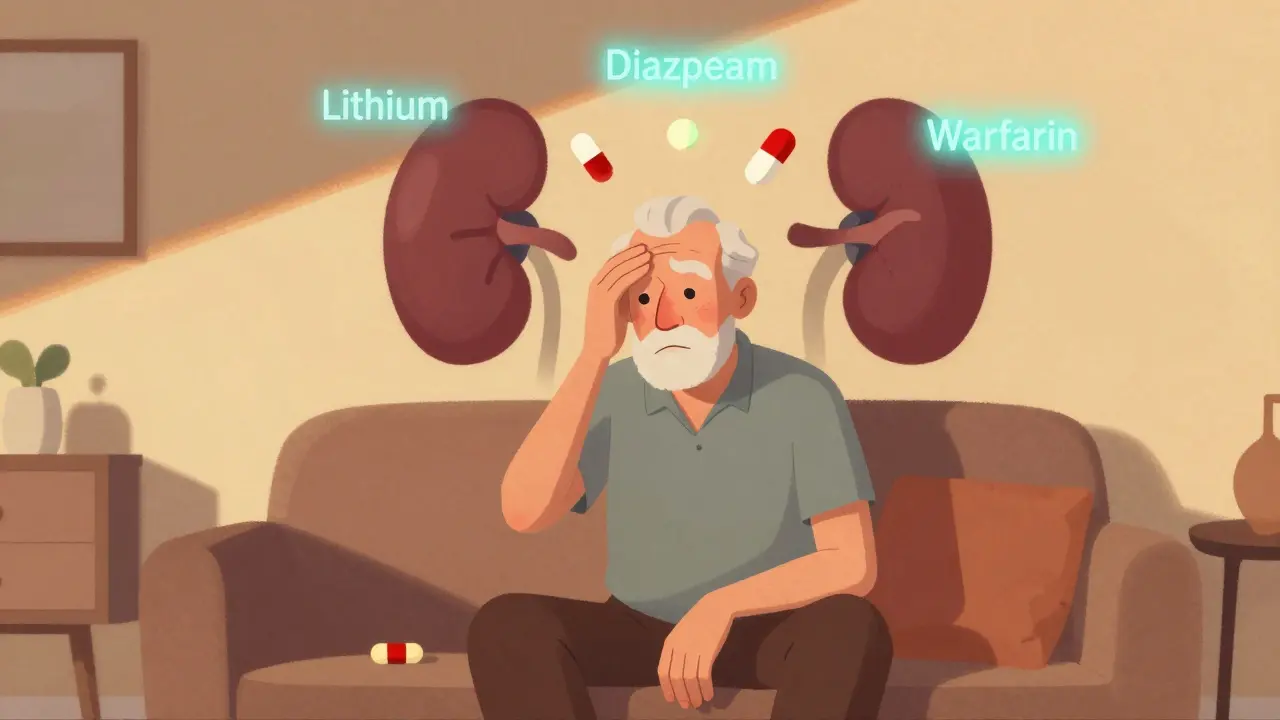
Your body doesn’t just slow down as you get older-it reorganizes. Between ages 25 and 80, total body water drops by about 15%, while body fat climbs from 25% to nearly 50% in women. That changes how drugs spread through your system. Water-soluble drugs like lithium get concentrated in less fluid, raising their levels dangerously. Fat-soluble drugs like diazepam stick around longer because they’re stored in extra fat tissue, slowly leaking back into the bloodstream. Your kidneys, which filter out most drugs, lose about 0.8 mL/min of function every year after 40. By 70, many people have lost half their kidney filtering power. That means drugs like digoxin, warfarin, and antibiotics stay in the body longer. Even if your blood test looks normal, your kidneys might be working at 40% capacity. Doctors who don’t check estimated glomerular filtration rate (eGFR) are flying blind. Your liver, which breaks down medications, also slows down. Blood flow to the liver drops by 20-40% between ages 25 and 65. That affects drugs like propranolol and verapamil, which rely on liver metabolism. Less breakdown means higher drug levels. And with less albumin-the protein that binds drugs in the blood-more of the active drug floats freely. That’s why warfarin, which is 99% bound to albumin, becomes much more potent in older adults. A normal dose can turn into a bleeding risk.Brain and Heart Changes Make Side Effects Worse
It’s not just about how your body handles drugs-it’s about how your brain and heart respond to them. Older brains are more sensitive. A dose of diazepam that causes mild drowsiness in a 30-year-old can cause deep sedation, memory loss, and confusion in a 75-year-old-even at the same blood level. That’s pharmacodynamics: the drug’s effect on the body, not just how the body processes it. Beta-blockers like propranolol need 50% higher doses in younger people to slow the heart. But in older adults, the heart doesn’t respond the same way. That means doctors might keep increasing the dose, thinking it’s not working-when in reality, the body can’t respond even with more drug. Meanwhile, blood pressure meds like amlodipine or doxazosin can cause sudden drops in pressure when standing. One in four people over 80 experience this, leading to falls, fractures, and hospitalizations. Anticholinergic drugs-common in sleep aids, allergies, and bladder meds-block acetylcholine, a brain chemical critical for memory and focus. In older adults, even small amounts can trigger delirium. A 2023 University of Florida study found people over 75 were 4.2 times more likely to go into delirium from these drugs than those under 65. Diphenhydramine (Benadryl) and oxybutynin are classic offenders. Yet they’re still sold over the counter and often prescribed without warning.Medicines That Should Be Avoided or Dosed Differently
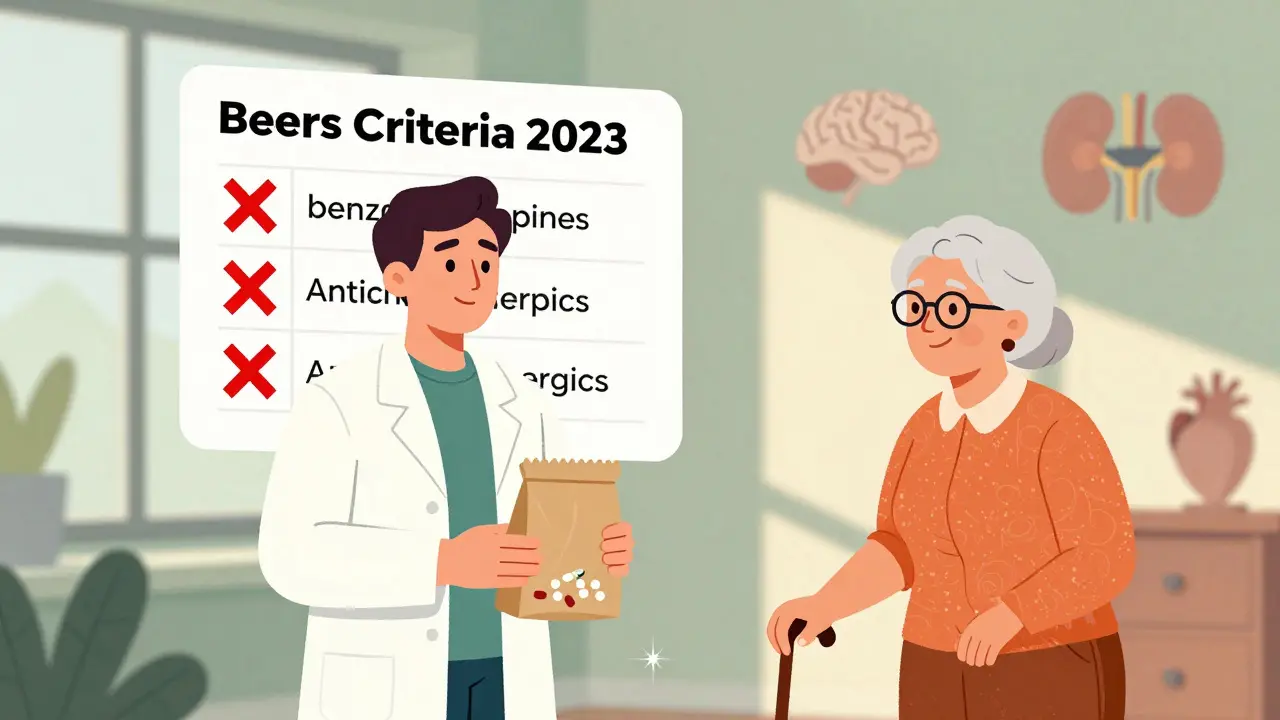
The American Geriatrics Society updates the Beers Criteria every two years to list drugs that are risky for older adults. The 2023 version flags 56 medications with high danger levels. These aren’t just “maybe dangerous”-they’re known to cause more harm than benefit in seniors.- Benzodiazepines (like lorazepam, alprazolam): 2-3 times higher risk of falls and hip fractures. Zolpidem causes 80% more next-day drowsiness in seniors.
- Anticholinergics (diphenhydramine, oxybutynin, tricyclic antidepressants): Linked to dementia-like symptoms, urinary retention, constipation, and confusion.
- NSAIDs (ibuprofen, naproxen): Increase risk of stomach bleeds and kidney failure. In older adults, even short-term use can be dangerous.
- Proton pump inhibitors (omeprazole): Long-term use raises risk of bone fractures, kidney disease, and C. diff infections.
- Antipsychotics (haloperidol, risperidone): Used for agitation in dementia-yet increase stroke risk by 30% and death risk by 1.6 times.
Polypharmacy: When More Pills Mean More Danger
Nearly half of adults over 65 take five or more prescription drugs monthly. One in five take ten or more. That’s polypharmacy-and it’s a ticking time bomb. Each new drug adds interaction risk. A blood thinner plus an NSAID? Bleeding risk spikes. A beta-blocker plus a diuretic? Electrolyte imbalance. A sedative plus an opioid? Respiratory depression. A 2022 JAMA study found that patients bringing all their meds-prescription, OTC, supplements-to a pharmacist review had an average of 3.2 medication errors uncovered per person. One man was taking three different sleep aids. A woman was on a blood pressure drug that worsened her kidney function and caused dizziness. Neither knew they were interacting. The CDC’s “Brown Bag Review” program-where patients bring all their pills to appointments-is one of the most effective tools we have. It’s simple. It’s cheap. And it works. Hospitals using it reduced medication errors by 31%.Real Stories Behind the Numbers
Behind every statistic is a person. One Reddit user, 78, started amitriptyline for nerve pain. Within three days, he couldn’t urinate. He needed a catheter. Amitriptyline is a strong anticholinergic. It’s listed in the Beers Criteria. His doctor didn’t know-or didn’t care. A caregiver on AgingCare.com shared that her 82-year-old mother fell and broke her hip after being prescribed the same blood pressure dose used for 50-year-olds. The doctor said, “It’s standard.” But standard doesn’t mean safe. Her mother’s eGFR was 42. Her kidneys were failing. The dose should’ve been cut in half. A 2022 survey of 1,200 older adults found:- 68% had dizziness or falls linked to meds
- 54% had memory problems or confusion
- 41% had unintended weight loss or gain

What Can Be Done? Practical Steps for Safer Medication Use
You don’t have to accept this as normal. There are clear, proven steps to reduce risk:- Ask for a full medication review every 6 months. Bring every pill, patch, vitamin, and herbal supplement. Ask: “Is this still necessary?”
- Check eGFR annually. If it’s below 60, ask if your meds need adjusting. Don’t rely on serum creatinine alone.
- Use the Beers Criteria as a checklist. Search “Beers Criteria 2023” online. Know what drugs to question.
- Ask about deprescribing. This isn’t stopping meds because you’re old-it’s stopping meds that no longer help. Studies show 30-50% of meds in nursing homes are unnecessary.
- Watch for red flags: New dizziness, confusion, constipation, falls, urinary problems, or mood changes. These aren’t “just aging.” They’re warning signs.
The Bigger Picture: Why This Matters Now
By 2040, 1 in 5 Americans will be over 65. Right now, preventable drug reactions cost the U.S. $30 billion a year. That’s not just money-it’s lives. Falls, hospitalizations, dementia-like symptoms, and early deaths are all tied to outdated prescribing. The FDA is finally pushing for older adults in clinical trials. Only 10% of drug studies include people over 75. That means we’re prescribing based on data from 30-year-olds. That’s like building a car for a teenager and expecting it to work for a 70-year-old driver. New tools are emerging: AI systems like MedAware reduce errors by 42%. Pharmacogenomic testing (checking your genes for how you metabolize drugs) cuts adverse reactions by 35% in seniors on antidepressants. These aren’t sci-fi-they’re here now. The future isn’t about more pills. It’s about smarter prescribing. Less is often more. And stopping a drug can be just as important as starting one.Why do older adults have more side effects from the same medication dose?
As people age, their bodies change: kidneys filter drugs slower, liver metabolism drops, body fat increases, and brain sensitivity rises. These changes mean drugs stay longer in the body and have stronger effects-even at the same dose. A pill that’s safe for a 40-year-old can be dangerous for a 75-year-old because their body handles it differently.
What are the most dangerous medications for seniors?
The 2023 Beers Criteria lists benzodiazepines (like lorazepam), anticholinergics (like diphenhydramine), NSAIDs (like ibuprofen), proton pump inhibitors (like omeprazole), and antipsychotics (like risperidone) as high-risk. These drugs increase fall risk, confusion, bleeding, kidney damage, and death in older adults. Many are still prescribed routinely despite known dangers.
How can I tell if a medication is causing side effects?
Look for new symptoms that started after beginning a new drug: dizziness, confusion, memory lapses, constipation, urinary trouble, unexplained falls, or sudden weight changes. These aren’t normal aging-they’re red flags. If you notice them, write down when they started and talk to your doctor or pharmacist right away.
Should I stop taking my meds if I feel side effects?
Never stop a medication suddenly without talking to your provider. Some drugs, like blood pressure or antidepressants, can cause dangerous withdrawal. But do bring all your pills to your next appointment and ask: “Could this be causing my symptoms? Is it still necessary?” Many older adults can safely stop one or more drugs with proper guidance.
What is deprescribing, and is it safe?
Deprescribing means carefully stopping medications that are no longer helping-or that do more harm than good. It’s not about quitting treatment; it’s about simplifying care. Studies show it reduces side effects, falls, hospitalizations, and even improves quality of life. It’s done gradually, under medical supervision, and is especially important for seniors on five or more drugs.
Can pharmacists help with medication safety?
Yes-pharmacists are trained to spot dangerous interactions and inappropriate prescriptions. Many offer free “Brown Bag Reviews,” where you bring all your pills (including vitamins and OTC meds), and they check for problems. This simple step finds an average of 3.2 errors per person. Ask your pharmacy if they offer this service.
Is it true that most clinical trials don’t include older adults?
Yes. About 90% of drug trials exclude people over 75, even though they’re the ones most likely to take the medicine. That means doctors often prescribe based on data from young, healthy adults. This creates a huge knowledge gap. The FDA now encourages including more older adults in trials, but progress is slow.
Next Steps: What to Do Today
If you or someone you care for is over 65 and taking multiple medications:- Make a list of every pill, patch, vitamin, and supplement.
- Call your pharmacy and ask if they do Brown Bag Reviews.
- Ask your doctor: “Based on my kidney function and current health, is each of these still necessary?”
- Download the Beers Criteria app or print the 2023 list from the American Geriatrics Society website.
- Track any new symptoms-write them down before your next visit.





Erwin Kodiat
20 January 2026 - 09:34 AM
Man, I saw my uncle go through this last year. Doc kept him on ibuprofen for his back, and he ended up in the ER with a bleed. No one asked about his kidney numbers. Just assumed he was ‘getting older’ and that’s that. We need better systems-like mandatory eGFR checks before prescribing anything to folks over 70.
Jacob Hill
20 January 2026 - 12:01 PM
It’s not just the drugs-it’s the culture. Doctors are trained to ‘fix’ things, not to question whether the fix is still needed. And patients? We’re conditioned to take pills like they’re candy. I’ve seen grandmas on five different sleep aids, three blood pressure meds, and a proton pump inhibitor… all because ‘it was prescribed.’ It’s not medicine-it’s maintenance by inertia.
Lewis Yeaple
20 January 2026 - 13:56 PM
While the general sentiment expressed herein is laudable, the underlying premise remains inadequately contextualized within the broader epidemiological framework of geriatric pharmacokinetics. The Beers Criteria, while useful, are not universally applicable; individual variability in cytochrome P450 enzyme activity, polypharmacy burden, and comorbid conditions necessitate case-by-case evaluation rather than blanket recommendations. Furthermore, the conflation of correlation with causation in the cited studies-particularly regarding anticholinergics and dementia-requires more rigorous longitudinal analysis.
Jackson Doughart
22 January 2026 - 09:33 AM
I’ve worked in home care for 18 years. I’ve held the hands of people who couldn’t remember their own names after taking Benadryl for allergies. I’ve seen the guilt on caregivers’ faces when they realize their mom’s ‘confusion’ was just a pill she didn’t need. This isn’t about blame. It’s about awareness. And sometimes, the most powerful thing you can do is say, ‘Let’s stop this one.’
Malikah Rajap
23 January 2026 - 11:09 AM
Wait-so you’re saying we should just stop giving people meds? Like… what if they need them? I mean, I get it, but isn’t this just fear-mongering? My auntie takes all these pills and she’s fine! She’s 83 and still does yoga! Maybe we’re just being too paranoid? Like, isn’t aging supposed to be messy? I just feel like… we’re making people scared of their own bodies.
Aman Kumar
23 January 2026 - 17:29 PM
You’re all missing the fundamental truth: this is the inevitable consequence of Western medical capitalism. Pharma companies design drugs for profit, not for human longevity. They target the elderly because they’re the most profitable demographic. Doctors are paid to prescribe, not to deprescribe. And patients? They’re conditioned to believe that pills equal care. This isn’t a medical crisis-it’s a moral failure. Stop taking your pills. Stop funding the machine.
Jake Rudin
24 January 2026 - 13:12 PM
There’s a quiet wisdom in aging, isn’t there? We forget that the body isn’t broken-it’s evolving. We treat it like a machine that needs tuning, but maybe it’s just… changing its rhythm. The same dose that once soothed now stirs chaos-not because the drug is evil, but because the vessel is different. Maybe the real question isn’t ‘what should we stop?’ but ‘what should we learn to let go of?’
Lydia H.
26 January 2026 - 06:06 AM
My grandma took amitriptyline for ‘nerve pain’ and turned into a zombie. She stopped talking for two weeks. We found out later it was on the Beers list. I showed her doctor. He shrugged and said, ‘Well, it was helping with sleep.’ I asked him what good is sleep if you’re not awake to enjoy it. He didn’t answer. So I took her off it. She started laughing again within a week.
Astha Jain
27 January 2026 - 07:48 AM
so like… why do we even have meds if they just make old people confused? like, why not just let them chill? i mean, if ur 80 and ur brain is slow, maybe its just time to stop fighting it? also, i think doctors are just lazy and dont wanna talk to old people
Phil Hillson
27 January 2026 - 15:30 PM
Look, I get it, but this whole post is just another ‘old people are fragile’ narrative. Why don’t we stop acting like seniors are broken toys that need to be fixed? They’ve lived. They’ve earned the right to take a pill if they want to. Who are we to say what’s ‘safe’ for someone else’s life? This isn’t medicine-it’s paternalism wrapped in a Beers Criteria hoodie
Josh Kenna
29 January 2026 - 12:37 PM
My dad’s on 11 meds. We did the brown bag thing. Found out he was taking two different blood pressure pills that canceled each other out, plus melatonin and trazodone and a weird herbal thing from Amazon. His doctor had no idea. I cried in the parking lot. But then we cut five of them. He’s got more energy now. He’s not dizzy. He’s sleeping better. And he’s still alive. So yeah, this isn’t just theory. It’s real. And it’s worth fighting for.