More than 90% of prescriptions filled for older adults in the U.S. are for generic drugs. That’s not because they’re cheaper-though they are-but because they’re widely available, covered by insurance, and trusted by doctors. But here’s the thing: generic drugs aren’t always as simple as they seem when you’re over 65. What works for a 40-year-old might be dangerous for an 80-year-old, no matter if it’s brand-name or generic.
Why Age Changes How Drugs Work
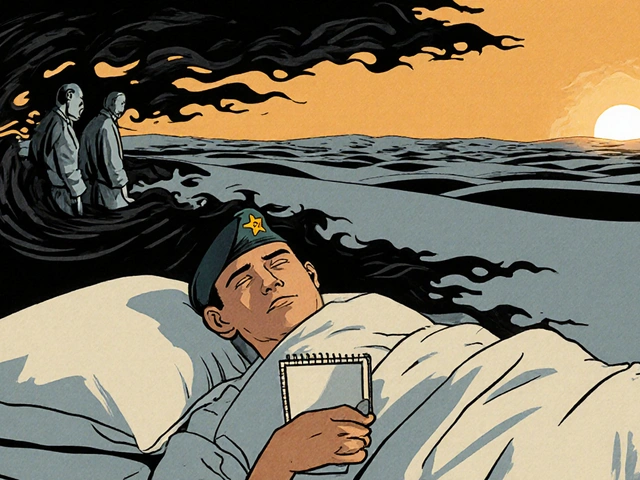
Your body doesn’t process medicine the same way at 75 as it did at 45. As you age, your liver slows down. Your kidneys don’t filter as well. Your body holds onto more fat and less water. These aren’t just minor changes-they change how long a drug stays in your system, how strong its effect is, and whether it builds up to dangerous levels. A 2023 study found that drug metabolism can drop by up to 30% in people over 75. That means a normal dose of a blood pressure pill, sleep aid, or painkiller might be a full overdose. The Caregiver.org guide puts it plainly: "A 'normal dose' of a medication can be an overdose for many older persons." This is especially true for drugs that affect the brain. Sedatives, antidepressants, and muscle relaxants like cyclobenzaprine (Flexeril) can cause dizziness, confusion, or falls. Falls are the leading cause of injury-related death in older adults. And it doesn’t matter if the drug is generic or brand-name-what matters is the dose and the person’s body.Polypharmacy: The Silent Killer
The average Medicare beneficiary fills 48 prescriptions a year. Nearly 9 out of 10 are generics. Many of those are for different conditions-high blood pressure, arthritis, diabetes, depression, acid reflux. But when you take five or more drugs at once, your risk of a bad reaction jumps from 13% to 58%. With seven or more, it’s 82%. This isn’t about one bad pill. It’s about how they interact. A blood thinner like warfarin might work fine alone, but add a common antibiotic like ciprofloxacin, and suddenly your blood won’t clot right. Or mix an opioid painkiller with a sleep aid like benzodiazepine, and your breathing could slow to a stop. A 2015 JAMA study found that combination increases overdose risk by 154%. The American Geriatrics Society’s Beers Criteria-updated in 2023-is the gold standard for spotting dangerous drug combinations in older adults. It doesn’t care if a drug is generic or brand. It only asks: Is this the right drug for someone this age, with these other conditions?Generic vs. Brand: Is There a Real Difference?
The FDA says generic drugs are just as safe and effective as brand-name ones. They must have the same active ingredient, strength, and route of delivery. And for most drugs, that’s true. But there’s one big exception: drugs with a narrow therapeutic index (NTI). These are medicines where even a tiny change in blood level can cause harm. Warfarin (Coumadin) is the classic example. Too little, and you get a clot. Too much, and you bleed internally. A 2021 study in the Journal of Thrombosis and Haemostasis found generic warfarin is 98.7% equivalent to brand-name. But a 2023 survey of seniors showed 42% still believed the brand was safer. That fear isn’t just irrational-it’s real. One woman on Reddit reported her 82-year-old mother’s thyroid levels went wild after switching from brand-name Synthroid to generic levothyroxine. It took three dosage tweaks over six months to stabilize. The problem isn’t always the drug. It’s the pill. Generic versions can look different-color, shape, size. For someone with poor eyesight or memory issues, that’s a recipe for error. A 2023 MedShadow.org analysis found 28% of medication errors in older adults involved confusion between similar-looking generic pills. That’s more than double the rate for brand-name drugs.
Drugs to Watch Out For (Even If They’re Generic)
The Beers Criteria 2023 update lists specific drugs that should be avoided or used with extreme caution in older adults. These rules apply whether the drug is generic or brand:- NSAIDs (like ibuprofen or naproxen): Can cause kidney failure, stomach bleeding, or worsen heart failure. Even over-the-counter ones.
- Benzodiazepines (like diazepam or lorazepam): Increase fall risk by 40%. Often prescribed for anxiety or sleep-but rarely safe long-term for seniors.
- Anticholinergics (like diphenhydramine/Benadryl): Cause confusion, dry mouth, constipation, and urinary retention. Found in many sleep aids and allergy meds.
- SNRIs (like venlafaxine): Linked to a 37% higher fall risk due to dizziness and low blood pressure.
- Direct oral anticoagulants (like rivaroxaban): Higher risk of stomach bleeding in people over 75 compared to warfarin.
- Insulin and sulfonylureas: Can cause dangerous low blood sugar, leading to falls, confusion, or brain injury. Risk is 20-25% higher in older adults.
What You Can Do to Stay Safe
You don’t have to give up your meds. You just need to manage them smarter.- Keep a current list of every pill, supplement, and over-the-counter drug you take. Include doses and why you take them. Bring it to every doctor visit.
- Ask for a medication review every three to six months if you’re on five or more drugs. Pharmacists can spot interactions, duplicate prescriptions, and outdated meds. A 2022 meta-analysis showed this reduces adverse events by 27%.
- Use pill organizers. Color-coded weekly dispensers cut medication errors by 34%, according to the Journal of the American Geriatrics Society.
- Ask about size and ease. Many generics come in large, hard-to-swallow tablets. Ask your pharmacist if there’s a smaller, easier version. In 2022, the FDA approved 37 new age-friendly generic formulations, including crushable tablets and liquid versions.
- Check expiration dates. One in five medication errors in seniors comes from using expired or improperly stored drugs.
- Read the label. If you can’t read the print, ask for large-type labels. Sixty-five percent of adults over 65 have vision problems that make small print hard to read.

When to Question a Generic Switch
Switching from brand to generic is usually fine. But if you’ve been stable on a brand-name drug for years-and then you get a generic version that makes you feel off-don’t ignore it. You’re not imagining it. Your body might be reacting to a different filler, dye, or coating. That’s not the FDA’s fault. It’s just how generics work. If your blood pressure, thyroid levels, or mood suddenly change after a switch, tell your doctor. You might need to go back to the brand-or adjust the dose. A 2022 study showed that when pharmacists took time to explain generics to seniors, 37% more of them accepted and used them correctly. Knowledge reduces fear.The Bottom Line
Generic drugs aren’t dangerous. But older adults aren’t just small adults. Their bodies handle medicine differently. The real risk isn’t whether a pill is generic or brand-it’s whether the right drug is being used at the right dose for the right person. The goal isn’t to avoid generics. It’s to use them wisely. That means regular reviews, clear labeling, careful dosing, and never assuming a pill is safe just because it’s cheap or covered by insurance. Your life depends on it-and so does your independence.Are generic drugs really as safe as brand-name drugs for older adults?
Yes, for most medications, generic drugs are just as safe and effective as brand-name versions. The FDA requires them to have the same active ingredient, strength, and absorption rate. But for drugs with a narrow therapeutic index-like warfarin, levothyroxine, or phenytoin-even tiny differences in absorption can matter. Older adults, due to changes in metabolism and kidney function, are more sensitive to these small variations. Always monitor how you feel after a switch and report any changes to your doctor.
Why do older adults have more side effects from medications?
As we age, our bodies change. The liver and kidneys process drugs more slowly, so medications stay in the system longer. Body fat increases and water decreases, which affects how drugs are distributed. The brain also becomes more sensitive to certain drugs, especially sedatives and antidepressants. This means a dose that’s safe for a 50-year-old can be toxic for an 80-year-old-even if it’s the same generic pill.
What’s the Beers Criteria, and why does it matter?
The Beers Criteria is a list of medications that are potentially inappropriate for older adults, updated every three years by the American Geriatrics Society. It’s not about brand vs. generic-it’s about whether a drug’s risks outweigh its benefits for someone over 65. For example, it warns against using benzodiazepines, NSAIDs, and certain antipsychotics because they increase fall risk, confusion, or organ damage. Doctors use it to avoid harmful prescriptions, no matter the drug’s price or label.
Can I switch from a brand-name drug to a generic without problems?
For most drugs, yes. But if you’re on a medication with a narrow therapeutic index-like warfarin, levothyroxine, or seizure drugs-talk to your doctor first. Some people experience changes in how they feel after switching, even if lab tests look normal. If you notice new dizziness, fatigue, or mood changes after a switch, don’t assume it’s just aging. It could be the medication. Ask for a review.
How can I reduce the risk of dangerous drug interactions?
Keep a complete list of every medication, supplement, and over-the-counter drug you take-including vitamins and herbal products. Bring it to every appointment. Ask your pharmacist to review it at least twice a year. Avoid starting new drugs without checking for interactions. And never take two drugs that both cause drowsiness or low blood pressure-like an opioid plus a sleep aid. That combo can be deadly.
Should I avoid all generic drugs if I’m over 75?
No. Most older adults safely take generic drugs every day. The problem isn’t generics-it’s inappropriate prescribing. Many seniors take drugs they don’t need, at doses too high for their age, or in combinations that are dangerous. The solution isn’t to avoid generics. It’s to use the right drugs, at the right dose, with regular reviews. Generic drugs save money and improve access-when used correctly.






Alex LaVey
3 February 2026 - 22:55 PM
My dad’s on six meds, and we just got him a color-coded pill organizer last month. He swears it’s the first time in years he hasn’t missed a dose. Seriously, these little changes matter more than we think. No magic bullet, just common sense.
rahulkumar maurya
4 February 2026 - 13:14 PM
Let’s be honest-most of these ‘generic’ switches are cost-cutting maneuvers disguised as healthcare efficiency. The FDA’s standards are laughably lax when it comes to bioequivalence thresholds for NTI drugs. If you’re over 70 and on warfarin, you’re playing Russian roulette with a pill that looks like a M&M.
Demetria Morris
5 February 2026 - 13:28 PM
I don’t care what the studies say-when my aunt switched from Synthroid to generic and started zoning out at family dinners, I knew it wasn’t just ‘getting older.’ Her TSH went from 2.1 to 8.9 in six weeks. No one listened until we went back to brand. Don’t let them gaslight you into thinking it’s all in your head.
Susheel Sharma
6 February 2026 - 14:17 PM
Generic drugs are fine for the masses, but let’s not pretend this is science-it’s economics wrapped in regulatory lipstick. 🤡 The real tragedy? Elderly patients are being turned into human pharmacokinetic experiments. And no, I don’t care if it’s ‘covered by insurance.’ If your kidneys can’t filter it, you shouldn’t be swallowing it.
Roshan Gudhe
7 February 2026 - 19:03 PM
There’s a deeper question here: Why do we treat aging like a disease to be medicated rather than a natural phase to be honored? We’ve turned elders into pill-counting automatons. The Beers Criteria isn’t just a list-it’s a mirror. Are we prescribing for longevity… or just avoiding the hard conversations about quality of life?
Rachel Kipps
7 February 2026 - 21:34 PM
i read this and thought of my mom-she takes 8 meds and cant read the labels anymore. we got her a big print version last week. its so simple but no one ever thinks to ask. thanks for reminding us to pay attention to the little things.
Prajwal Manjunath Shanthappa
8 February 2026 - 02:40 AM
Oh, please. You think the FDA cares? They’re busy approving ‘generic’ versions of insulin that cost $20… and then wonder why people die. This isn’t about safety-it’s about corporate greed, masked in clinical jargon. You’re not ‘managing’ your meds-you’re surviving a system designed to exploit you.
Wendy Lamb
9 February 2026 - 01:13 AM
My grandma uses a pill box and never misses a dose. She also refuses to take anything new without checking with her pharmacist first. Simple habits save lives.
Alex LaVey
11 February 2026 - 00:22 AM
Wendy, you just summed up everything I’ve been trying to say for years. My dad’s pharmacist even gave him a little card with his med list printed in 18pt font. That’s the kind of care that actually helps. Not just prescribing, but *seeing* the person.