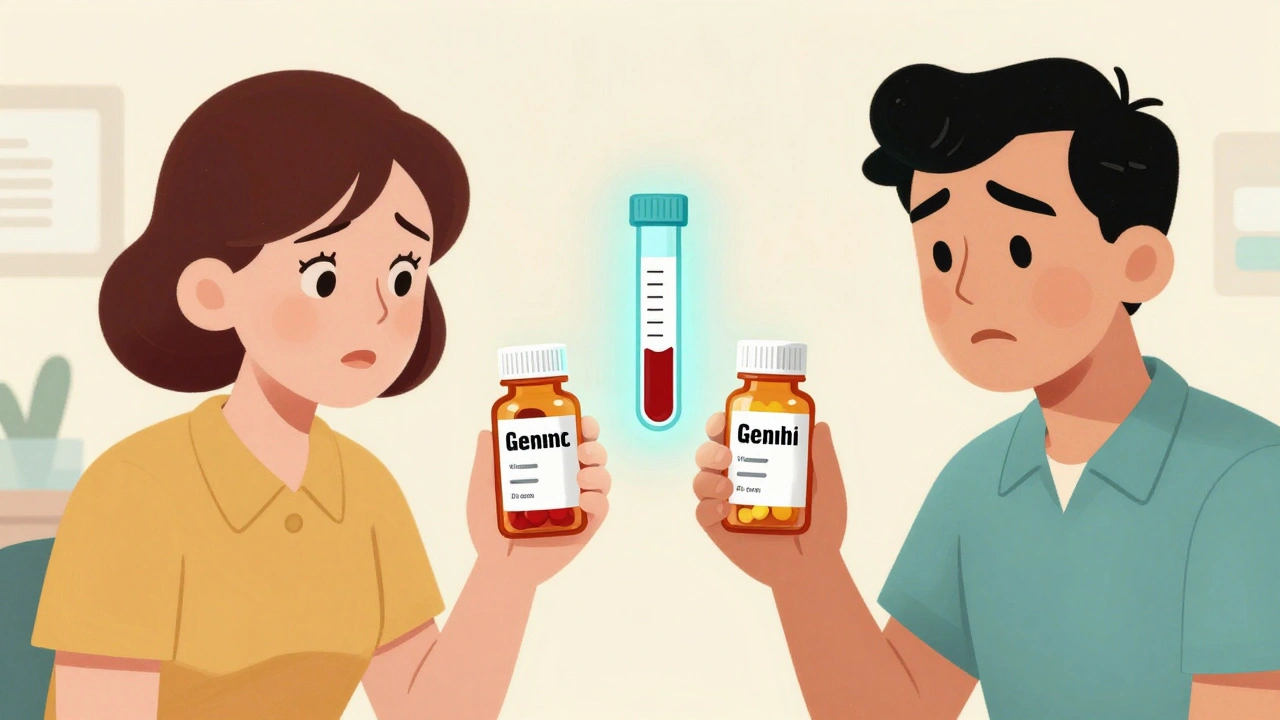
When a patient switches from a brand-name drug to a generic version, most people assume it’s a simple swap-same active ingredient, same effect. But for drugs with a narrow therapeutic index (NTI), that assumption can be dangerous. These are medications where the difference between a therapeutic dose and a toxic one is razor-thin. Even small changes in how the body absorbs or processes the drug can lead to treatment failure or serious harm. This isn’t theoretical. It’s happening right now in clinics across North America, especially with generics used for epilepsy, thyroid disorders, warfarin, and certain antiretrovirals.
What Makes a Drug an NTI?
NTI stands for narrow therapeutic index. It doesn’t mean the drug is weak-it means the margin for error is tiny. For example, warfarin (a blood thinner) has a therapeutic range of 2 to 3 on the INR scale. Go below 2, and you risk a clot. Go above 3, and you risk a bleed. One generic formulation might deliver 95% of the intended dose. Another might deliver 105%. That 10% difference? In a regular drug, it’s negligible. In an NTI drug, it’s the difference between safety and disaster.
The FDA allows generic drugs to vary by ±20% in bioavailability compared to the brand. That’s legal. But for NTI drugs, that variation isn’t just acceptable-it’s risky. The FDA acknowledges this with a special list of NTI drugs that require tighter controls. Yet, many prescribers and pharmacists don’t know which drugs fall into this category. And patients? They’re often unaware their medication was switched at the pharmacy counter.
Why Generic NTI Drugs Are a Hidden Risk
Generic manufacturers aren’t cutting corners. They follow the law. But bioequivalence testing is done on healthy volunteers, not patients with liver disease, kidney impairment, or complex drug interactions. A patient on levothyroxine for hypothyroidism might be stable for years on one brand. Then, their insurance changes, and they’re switched to a cheaper generic. Their TSH level, which was at 2.1, jumps to 7.8 in six weeks. They feel tired. Gain weight. Their doctor blames poor diet. They don’t realize the pill they’re taking now has a different filler that slows absorption.
Same thing happens with phenytoin, an antiseizure drug. A patient’s seizure control is perfect. Then they get a new prescription filled with a different generic. Within days, they have a seizure. Their blood level? Half of what it was. The generic has a different dissolution profile. The active ingredient is the same-but how fast it enters the bloodstream? Not the same.
This isn’t about quality control failures. It’s about pharmacokinetic variability. Two pills with identical chemical formulas can behave differently in the body because of binders, coatings, or manufacturing processes. For NTI drugs, those differences matter.
Therapeutic Drug Monitoring: The Safety Net
Therapeutic Drug Monitoring (TDM) is the process of measuring the actual concentration of a drug in a patient’s blood to ensure it’s in the safe and effective range. It’s not new. It’s been used for decades with drugs like digoxin, lithium, and vancomycin. But for NTI drugs, it’s becoming essential-not optional.
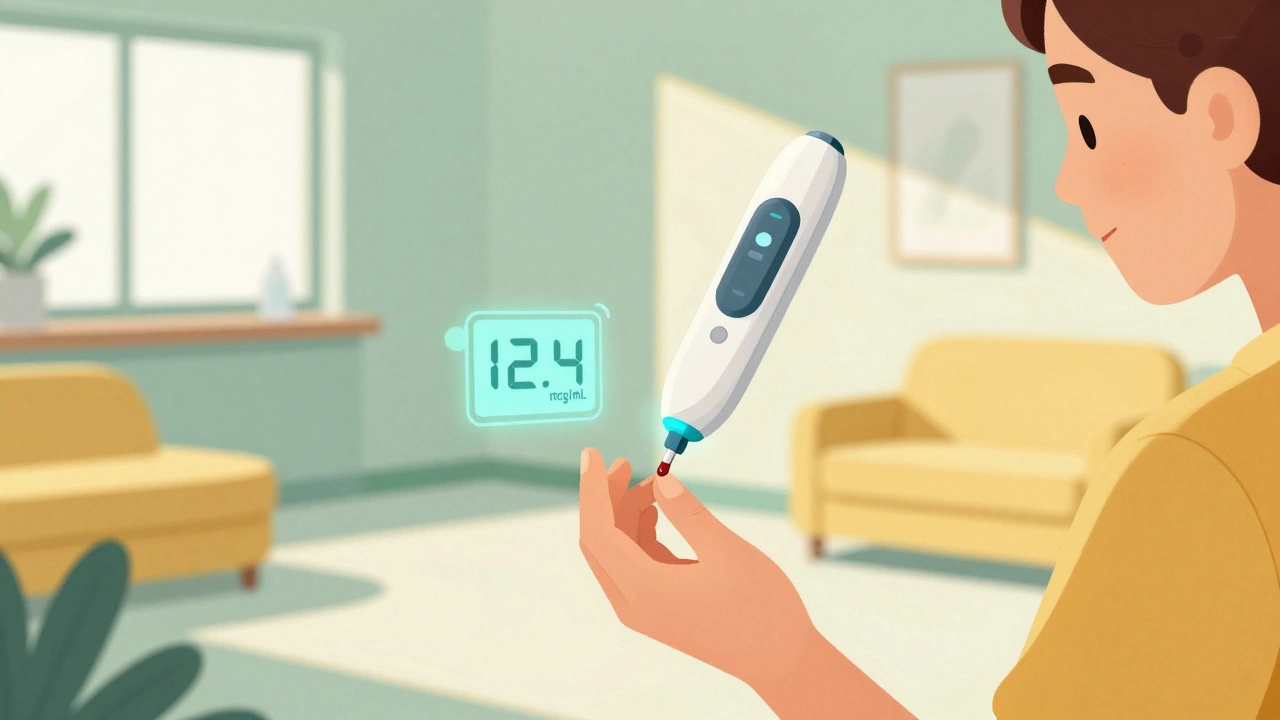
TDM works by drawing a blood sample, usually at the lowest point in the dosing cycle (trough level), and running it through a specialized lab assay. The result? A precise number: 12.4 mcg/mL for phenytoin, 0.5 ng/mL for cyclosporine, 2.3 mg/L for levothyroxine. These numbers are compared to published therapeutic ranges. If the level is too low, the dose is increased. Too high? It’s reduced.
Studies show TDM reduces adverse events by up to 30% in patients on NTI drugs. In one 2023 study of 187 patients on generic levothyroxine, those who had TDM performed after a switch had 89% fewer cases of abnormal TSH levels compared to those who didn’t. In another, patients on generic phenytoin who underwent TDM had 40% fewer emergency visits due to seizures or toxicity.
It’s not perfect. Results can take 7-14 days in public labs. Costs range from $150 to $400 per test. But compared to the cost of a hospitalization from a bleeding event or uncontrolled seizure? TDM pays for itself.
Who Needs TDM the Most?
TDM isn’t for everyone. But it’s critical for certain patients:
- Patients recently switched from brand to generic NTI drugs
- Those with kidney or liver disease (affects drug clearance)
- Older adults (altered metabolism and protein binding)
- Pregnant women (changing volume of distribution)
- Patients on multiple medications (drug interactions can alter levels)
- Anyone with unexplained treatment failure or side effects
For example, a 72-year-old woman on warfarin takes her generic version for six months. Her INR has been stable at 2.5. Then she starts a new antibiotic for a sinus infection. Within a week, her INR spikes to 6.8. She’s bruising easily. Her doctor doesn’t realize the antibiotic is inhibiting the enzyme that breaks down warfarin. TDM could have caught the rising warfarin level before the bleeding started.
Another case: a 34-year-old man on generic carbamazepine for seizures. He’s been fine for two years. Then his pharmacy switches him to a new generic. Two weeks later, he has a tonic-clonic seizure. His blood level? 3.1 mcg/mL-the therapeutic range is 4-12. He was subtherapeutic. His doctor assumed he missed doses. He hadn’t. The generic just didn’t deliver enough.
Barriers to Widespread Use
Why isn’t TDM routine for NTI drugs? Three big reasons:
- Cost and access-Many insurance plans don’t cover TDM for NTI drugs unless there’s clear clinical instability. Private labs charge more, and public labs have long waits.
- Lack of awareness-Many clinicians don’t know which drugs are NTI or how to interpret results. Pharmacists aren’t always trained to flag switches.
- Assumption of equivalence-The myth that “generic = same” is deeply ingrained. Even when guidelines say otherwise, it’s hard to change practice.
Some states, like California and New York, have passed laws requiring pharmacists to notify patients when switching NTI drugs. But most haven’t. And even when notified, patients rarely push back. They trust the system.
What Patients Can Do
You don’t need to be a doctor to protect yourself.
- Ask your pharmacist: “Is this the same brand I was on?” If it’s different, ask if it’s an NTI drug.
- Know your drug’s name and purpose. Levothyroxine, phenytoin, warfarin, digoxin, cyclosporine, tacrolimus-these are high-risk.
- If you feel different after a switch-fatigued, dizzy, having new symptoms-ask for a blood test. Don’t wait.
- Keep a log: note when you switch pills and when symptoms start or change.
- Request TDM if you’re on a high-risk drug and have a change in health, age, or other meds.
One patient in Calgary, after switching to a new generic levothyroxine, felt worse for three months. Her doctor dismissed it as stress. She asked for a TDM test herself. Her level was 30% below target. After adjusting her dose, her energy returned in two weeks. She didn’t wait for the system to fix it-she acted.
The Future: TDM as Standard Care
More hospitals and clinics are starting to offer TDM for NTI drugs. In Canada, the McGill University Health Centre and Calgary’s Foothills Medical Centre now include TDM in their protocols for patients on critical NTI regimens. Private labs offer faster turnaround-some as quick as 48 hours-for a premium.
Technology is helping too. Point-of-care devices that measure drug levels with a finger-prick blood sample are in development. Within five years, a doctor might check your phenytoin level during a 15-minute visit.
The goal isn’t to eliminate generics. It’s to make them safer. TDM doesn’t replace clinical judgment-it supports it. It turns guesswork into data. It turns assumptions into evidence.
For patients on NTI drugs, TDM isn’t a luxury. It’s a lifeline.
What drugs are considered narrow therapeutic index (NTI) drugs?
Common NTI drugs include warfarin (blood thinner), levothyroxine (thyroid hormone), phenytoin and carbamazepine (anti-seizure), digoxin (heart medication), cyclosporine and tacrolimus (immunosuppressants), lithium (mood stabilizer), and some antiretrovirals like lopinavir and ritonavir. These drugs have a small window between effective and toxic doses. Even minor changes in blood levels can cause harm.
Can I trust that all generic NTI drugs are the same?
No. While generics must meet FDA bioequivalence standards, those standards allow up to a 20% variation in absorption compared to the brand. For NTI drugs, that variation can be clinically significant. Two generics with the same active ingredient may behave differently in your body due to different fillers, coatings, or manufacturing methods. TDM is the only way to confirm you’re getting the right dose.
How often should I get therapeutic drug monitoring done?
You should get TDM done when you first switch to a new generic version of an NTI drug. After that, it’s recommended after any major change: new illness, weight change, pregnancy, starting or stopping other medications, or if you notice new symptoms. Once stable, annual checks may be sufficient-but only if your health remains unchanged.
Is therapeutic drug monitoring covered by insurance?
Coverage varies. In Canada, public plans rarely cover TDM for NTI drugs unless there’s documented instability. Private insurance may cover it if your doctor submits a letter of medical necessity. In the U.S., Medicare and many private insurers cover TDM for specific NTI drugs when ordered for approved indications. Always check with your provider before testing.
What if my doctor says TDM isn’t necessary?
Ask why. If they say, “Generics are the same,” that’s outdated thinking. Cite guidelines from the FDA or the American Society of Health-System Pharmacists (ASHP), which recommend TDM for NTI drugs when switching formulations. If your doctor is unwilling, ask for a referral to a pharmacist specializing in drug monitoring or an infectious disease or endocrinology specialist who uses TDM routinely.
Can TDM prevent hospitalizations from generic drug switches?
Yes. Studies show TDM reduces hospitalizations by up to 40% in patients on NTI drugs after a generic switch. For example, in patients on warfarin, TDM helped prevent dangerous bleeding episodes by catching rising drug levels before symptoms appeared. In epilepsy patients, it stopped seizures by identifying subtherapeutic levels early. TDM doesn’t guarantee safety-but it turns random risk into controlled management.




Vivian Amadi
12 December 2025 - 02:10 AM
This is why generics are a scam. I got switched to a cheap levothyroxine and felt like a zombie for months. My doctor laughed when I complained. TDM? He said it's 'overkill.' Bullshit. My TSH was off by 40%. They don't care until you're in the ER.
Jimmy Kärnfeldt
13 December 2025 - 10:53 AM
I get it - the system’s broken, but I’m glad someone’s finally talking about this. I used to work in a pharmacy and saw patients switch meds all the time without a word. No one tells them. No one checks. It’s not malice, it’s just... inertia. TDM isn’t fancy - it’s basic safety. Why are we still arguing about this in 2025?
Ariel Nichole
13 December 2025 - 17:50 PM
My mom’s on warfarin and switched generics last year. She didn’t notice anything until she started bruising like a toddler who fell down the stairs. We pushed for TDM and found her levels were creeping up. Saved her from a bleed. Honestly? This should be standard. No one should have to fight for a blood test just to stay alive.
matthew dendle
15 December 2025 - 08:48 AM
generic = same lol. yeah right. i got switched to some pheno thing and had a seizure on my couch. doc said i was stressed. i said no dumbass its the pill. he ordered tdm 3 weeks later. my level was half what it shoulda been. now i pay out of pocket just to not die. thanks america
Lisa Stringfellow
16 December 2025 - 21:01 PM
Wow. Another alarmist post about generics. People are so paranoid these days. If the FDA says it’s approved, why are you acting like it’s poison? Maybe you just need to stop obsessing over every little change in your body. Not everything is a crisis.
Kristi Pope
17 December 2025 - 06:33 AM
My cousin’s a nurse in Oregon and she told me they started doing TDM for all new NTI switches last year. No more guessing. No more ‘maybe it’s stress.’ Just blood tests, clear numbers, and real care. It’s not expensive - it’s just not prioritized. We treat diabetes like this. Why not epilepsy or thyroid? We’re smarter than this.
Sylvia Frenzel
17 December 2025 - 18:52 PM
Why are we letting American drug companies profit off this? In Canada, they don’t switch NTI drugs without notification. Here? You’re a number. Insurance wants the cheapest pill. Patients get the consequences. This isn’t healthcare. It’s corporate arithmetic.
john damon
19 December 2025 - 09:06 AM
bro i just want to live. 🥲 i switched to a generic cyclosporine after transplant and my levels crashed. they didn’t test me for 6 weeks. i almost lost the kidney. now i beg for tdm every time. please just listen to people who’ve been through this.
Monica Evan
20 December 2025 - 19:11 PM
As a pharmacist in rural Ohio, I see this every week. Patients don’t even know they got switched. The pharmacy system auto-substitutes and no one flags NTI drugs. I’ve started printing little cards for high-risk med patients - ‘Check your pill before you leave.’ Small thing. Maybe it saves someone. TDM isn’t luxury - it’s dignity.
Aidan Stacey
22 December 2025 - 03:43 AM
My brother’s a neurologist. He used to think generics were fine. Then his patient had a seizure after a switch. Turned out the generic had a different coating - delayed absorption. Blood level was 40% below therapeutic. He now insists on TDM for every NTI switch. No more assumptions. No more ‘probably fine.’ Data over dogma.
Jean Claude de La Ronde
22 December 2025 - 15:43 PM
in canada we call this the ‘generic gamble’ and yeah its a thing. my buddy switched to some cheap levothyroxine and his tsh went from 2.4 to 8.1. doc said ‘maybe you’re not taking it right.’ he was taking it the same way for 10 years. turned out the new pill had cellulose instead of lactose. body hates cellulose. tdm saved him. now he only takes the brand. screw the cost.
Aman deep
24 December 2025 - 03:39 AM
i live in india and we dont have this problem much because most ntis are still brand here - too expensive to copy. but i read about this and i just feel so sad. people in the us are dying because of paperwork and profit margins. we need to fix this. tdm is not expensive compared to a hospital bed. why is this even a debate?
Paul Dixon
25 December 2025 - 10:33 AM
My sister’s on carbamazepine. Switched generics. Got a seizure. TDM showed her level was 3.2 - way below 4. They blamed her for missing doses. She’s the most consistent person I know. She’s now fighting for a law that says pharmacists must notify patients before switching NTI meds. It’s not radical. It’s common sense.
Jim Irish
25 December 2025 - 15:13 PM
Therapeutic Drug Monitoring is not a luxury. It is a necessary clinical tool for medications with narrow therapeutic indices. The current regulatory framework for bioequivalence is insufficient for these agents. Clinical outcomes data consistently support the implementation of TDM in these cases. Healthcare systems must adapt to evidence, not cost-efficiency metrics.