Every time you pick up your prescription, you might be getting a different pill-even if the name on the bottle hasn’t changed. That’s because generic medications from different manufacturers can look, size, color, and even taste different. For many drugs, this doesn’t matter. But for others, switching between generic versions can have real consequences. You might not know it, but your pharmacy may be swapping out your generic medication every few weeks based on what’s cheapest or in stock. And if you’re taking something like warfarin, levothyroxine, or an epilepsy drug, that switch could affect how you feel-or even put you at risk.
Why Do Generic Medications Keep Changing?
Generic drugs aren’t just cheaper copies-they’re approved by the FDA to have the same active ingredient, strength, and dosage form as the brand-name version. But they don’t have to be identical in every way. The inactive ingredients-like fillers, dyes, and coatings-can vary between manufacturers. That’s why a pill from Teva might be oval and white, while the same drug from Mylan is round and blue. The reason these switches happen? Money. Insurance companies and pharmacy benefit managers push for the lowest-cost generic option. Hospitals and pharmacies buy in bulk, and the manufacturer offering the best price wins the contract. So if Teva drops their price next month, your pharmacy will switch your prescription to theirs-even if you’ve been taking Mylan for years. In the U.S., over 90% of prescriptions are filled with generics. That’s great for savings-generics cost 80% to 85% less than brand-name drugs, saving consumers $8-10 billion a year. But with more than four generic makers competing for each off-patent drug, the chances of switching keep rising.When Switching Can Be Risky
Not all drugs are created equal when it comes to switching. For most medications-like statins, antibiotics, or blood pressure pills-switching between generics causes no noticeable difference. But for drugs with a narrow therapeutic index (NTI), even small changes in blood levels can lead to serious problems. NTI drugs have a very small window between a dose that works and a dose that’s toxic. A few percentage points of variation in absorption can mean the difference between control and crisis. These include:- Levothyroxine (for hypothyroidism): Even tiny changes in thyroid hormone levels can cause fatigue, weight gain, or heart palpitations. Patients report feeling awful for weeks after a manufacturer switch.
- Warfarin (a blood thinner): Too little, and you risk a clot. Too much, and you could bleed internally. INR levels often fluctuate after a generic switch, requiring frequent blood tests.
- Tacrolimus (for transplant patients): A drop in blood levels can trigger organ rejection. Many transplant centers now lock patients into one specific generic brand.
- Antiepileptic drugs: Patients switching generics report breakthrough seizures. One study found 20.8% to 44.1% of epilepsy patients switched back to their original brand after problems.
What Patients Are Reporting
Real people are noticing the difference. On Reddit, a user wrote: “My seizure med switched from Mylan to Teva. Two breakthrough seizures later, my neurologist checked my blood levels-they dropped sharply.” On Drugs.com, someone with hypothyroidism said: “Every time my levothyroxine changes, my TSH goes wild. I feel like garbage for weeks until my doctor adjusts the dose.” But it’s not all bad. Many people report no issues. A GoodRx reviewer said: “I’ve been on generic lisinopril for five years. Five different manufacturers. My blood pressure never budged.” A review of 1,247 patient reports showed:- 68% noticed no difference
- 22% said the new generic didn’t work as well
- 10% developed new side effects
Why Your Doctor Might Not Know
Here’s the kicker: your doctor probably doesn’t know when your generic switches. Pharmacies don’t notify prescribers when they swap manufacturers. In a 2023 survey, 62% of doctors said they only found out about a switch when a patient came in with symptoms. That’s a problem. If you’re on levothyroxine and your TSH spikes after a refill, your doctor might think you missed doses or changed your diet-not that your pill is now made by a different company. And because most generics look different, patients get confused. One study found 67% of people identify their meds by shape and color. When those change, they think they’ve been given the wrong drug. Some even double up, thinking the new pill is “stronger.” That leads to 11.5% of cases where patients accidentally take two doses.What You Can Do
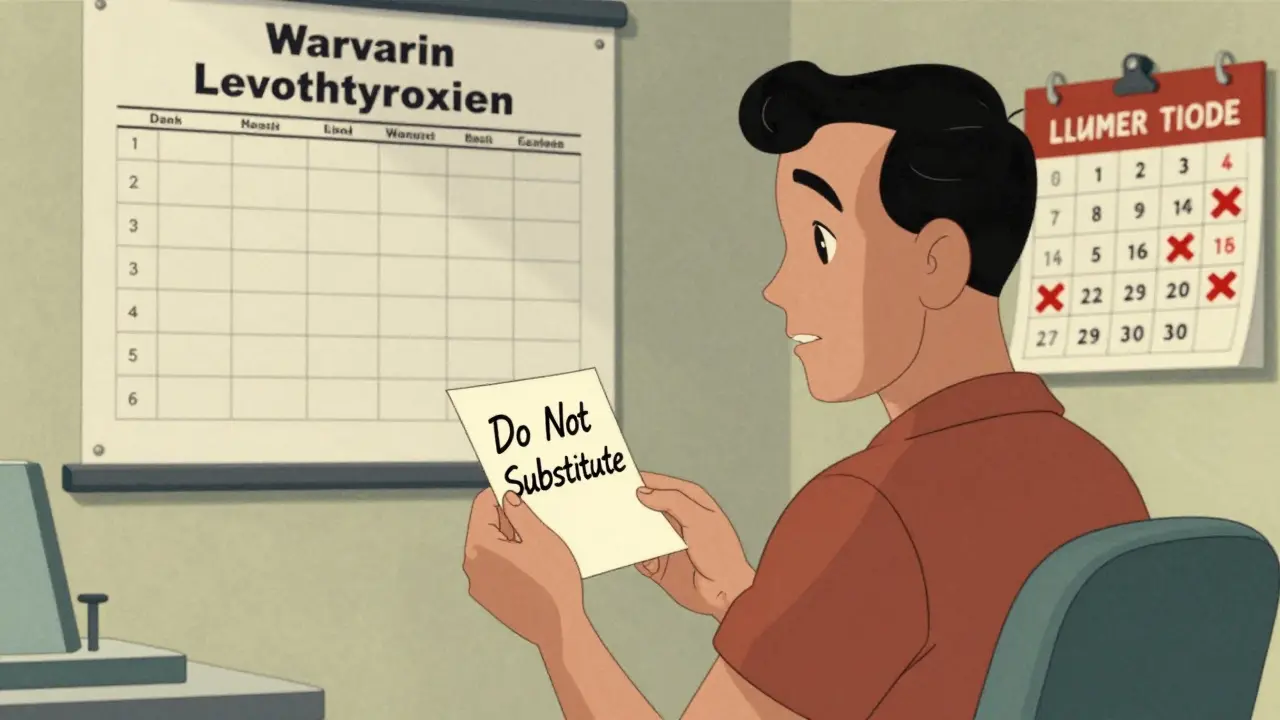
You don’t have to accept random switches as normal. Here’s what works:- Ask your pharmacist which manufacturer made your last refill. Write it down. If it changes, ask why.
- Request a specific generic if you’ve had problems before. Say: “I’ve had issues with Teva’s version. Can I stay on Mylan?”
- Ask your doctor to write “Dispense as Written” or “Do Not Substitute” on your prescription. This legally prevents the pharmacy from switching without your doctor’s approval.
- For NTI drugs, ask about a “lock-in” program. Some clinics and insurers now designate one generic brand for patients on warfarin, levothyroxine, or tacrolimus to avoid constant changes.
- Check your blood levels after any switch. If you’re on warfarin, get an INR test within a week. If you’re on thyroid meds, ask for a TSH test in 4-6 weeks.
- Use a pill organizer and keep a list of your meds with manufacturer names. That way, you’ll notice if something changes.

What’s Changing in the System
The FDA is starting to pay attention. In 2023, they launched a pilot program requiring generic makers to report major formulation changes. In 2024, Medsafe (New Zealand’s drug regulator) issued new guidance advising against switching levothyroxine brands unless absolutely necessary. The Generic Pharmaceutical Association is also working on standardized pill designs to help patients recognize their meds, no matter the manufacturer. And by 2028, experts predict that while 78% of prescriptions will still be generic, there will be stricter rules on switching for high-risk drugs.Bottom Line
Generic drugs save money. That’s a good thing. But not all generics are interchangeable-and that’s not always obvious. For most people, switching between manufacturers is harmless. But if you’re on a drug with a narrow therapeutic index, or you’ve noticed changes in how you feel after a refill, don’t brush it off. Your health isn’t a cost-saving experiment. If your pill looks different, ask questions. If you feel off, get tested. And if you’re on a critical medication, ask your doctor to lock you into one brand. It’s your right to know what you’re taking-and to make sure it works the way it should.Can I ask my pharmacy to keep giving me the same generic brand?
Yes. You can ask your pharmacist to fill your prescription with the same generic manufacturer each time. If they say they can’t, ask your doctor to write “Dispense as Written” or “Do Not Substitute” on the prescription. This legally prevents the pharmacy from switching without your doctor’s approval.
Why do generic pills look different every time?
Generic drug manufacturers are not required to make their pills look like the brand-name version or each other. They can use different colors, shapes, sizes, and coatings. This is why your pill might change every refill-it’s just a different company making the same active ingredient.
Are all generic drugs the same quality?
All FDA-approved generics must meet the same safety and effectiveness standards as brand-name drugs. But they can differ in inactive ingredients and how quickly the active ingredient is absorbed. For most drugs, this doesn’t matter. For drugs with a narrow therapeutic index, these small differences can have real effects.
Which medications are most affected by switching generics?
Drugs with a narrow therapeutic index are most sensitive to changes. These include levothyroxine (for thyroid), warfarin (blood thinner), tacrolimus (transplant), and antiepileptic drugs like phenytoin or carbamazepine. Patients on these medications are more likely to experience side effects or loss of effectiveness after a switch.
Should I get blood tests after switching generics?
If you’re on a drug with a narrow therapeutic index-like warfarin, levothyroxine, or tacrolimus-yes. Get your blood levels checked 1-2 weeks after switching to make sure the new generic is working the same way. For example, INR for warfarin or TSH for thyroid meds should be retested to confirm stability.
Is it safe to switch between generic manufacturers for blood pressure or cholesterol meds?
For most people, yes. Drugs like lisinopril, atorvastatin, and metformin are generally stable across generic brands. Studies show less than 10% of patients report issues with switching these. But if you notice new side effects or changes in how you feel, it’s still worth checking with your doctor.






Pawan Chaudhary
16 December 2025 - 21:38 PM
Love this post! I’ve been on generic levothyroxine for years and never thought twice until my pill switched from white oval to blue round. Felt like a zombie for three weeks. Took me forever to connect the dots. Glad someone’s talking about this.
BETH VON KAUFFMANN
17 December 2025 - 11:35 AM
Let’s be clear: the FDA’s 80–125% bioequivalence window is a regulatory farce. For NTI drugs, that’s not variability-it’s pharmacological roulette. The fact that pharmacies are permitted to swap manufacturers without clinical oversight is a systemic failure of risk governance. We’re treating life-sustaining meds like commodity widgets.
Donna Packard
18 December 2025 - 06:53 AM
I’m so glad this is getting attention. My mom’s on warfarin and had a scary bleed after a switch. Her INR spiked overnight. We didn’t know why until we checked the pill. Now we always ask the pharmacist. Small things matter.
Patrick A. Ck. Trip
19 December 2025 - 14:51 PM
This is an important topic. I’ve noticed that many patients don’t realize generics can vary, and that’s not their fault. The system is confusing. I think doctors and pharmacists need to do more to educate. Maybe even label the manufacturer on the bottle. It’s a simple fix for a big problem.
Sam Clark
21 December 2025 - 00:17 AM
Thank you for outlining actionable steps. The ‘Dispense as Written’ directive is underutilized. Clinicians should be proactively discussing this with patients on NTI medications during refill counseling. A standardized patient handout from pharmacy chains could significantly reduce adverse events.
Jessica Salgado
21 December 2025 - 18:15 PM
Wait-so my seizures weren’t ‘stress-related’? I switched from Mylan to Teva and had two breakthrough seizures in two weeks. My neurologist said ‘it’s probably coincidence.’ I printed out this article and handed it to him. He finally ordered a level check. My drug concentration dropped 37%. Turns out, I’m not crazy. I’m just a patient who got treated like a statistic.
Salome Perez
22 December 2025 - 11:12 AM
As someone who’s lived in three countries, I’ve seen how differently this is handled. In Germany, generics are locked by prescription unless the doctor approves a switch. In the U.S., it’s a free-for-all. I get the cost savings, but we’re trading safety for savings. Maybe it’s time to treat NTI meds like insulin or vaccines-no substitutions without consent.
Kaylee Esdale
24 December 2025 - 09:10 AM
My dad takes levothyroxine. He stopped trusting his meds after the color changed. He’d skip doses because he thought the new pill was fake. We started keeping a little card with the pill’s shape and color. Now he knows it’s the same drug, just a different face. Small habits save lives.
Anna Giakoumakatou
24 December 2025 - 10:33 AM
Oh wow. So the FDA lets drug companies play Russian roulette with our hormones and seizures… and we’re supposed to be grateful for the 85% discount? Next they’ll say it’s fine to swap out insulin brands because ‘they’re both glucose regulators.’ How is this still legal?
CAROL MUTISO
24 December 2025 - 15:29 PM
It’s not just about the pills. It’s about the quiet erosion of patient autonomy. We’re told to trust the system, but the system doesn’t trust us enough to tell us what we’re taking. The real scandal isn’t the variability-it’s the silence. No one warns you. No one asks. We’re just expected to adapt. That’s not healthcare. That’s compliance training.
Meghan O'Shaughnessy
25 December 2025 - 10:52 AM
I work in a pharmacy. We switch generics based on what’s cheapest that week. We don’t track who’s on what. We don’t get training on NTI drugs. We just scan and dispense. This system isn’t broken-it was never built for patients.
Philippa Skiadopoulou
25 December 2025 - 20:50 PM
UK handles this better. We have a ‘brand name’ flag on prescriptions for NTI drugs. Pharmacists must notify the prescriber if they can’t supply the branded version. Simple. Effective. Why can’t the US adopt this?
Jonathan Morris
26 December 2025 - 19:12 PM
This is all a controlled distraction. The real issue? The FDA is captured by Big Pharma. The 80–125% range was designed by manufacturers to allow variability while still getting approval. They profit from the chaos. They know patients won’t notice until it’s too late. This isn’t negligence. It’s profit-driven design.
Linda Caldwell
26 December 2025 - 22:31 PM
You’re not alone. I’ve been there. My TSH went from 3.2 to 12.8 after a switch. I cried in the pharmacy parking lot. But I spoke up. I asked for my old brand. I got it. You have power. Use it. Don’t let them make you feel like you’re overreacting. Your body knows. Trust it.