PMDD Symptom Tracker
Track your mood, anxiety, and physical symptoms over at least two menstrual cycles to identify patterns that can help you and your clinician make an accurate diagnosis.
Mood Symptoms
Anxiety Symptoms
Physical Symptoms
Other Factors
Key Pattern Detected
Track at least two menstrual cycles to see your symptom patterns.
Symptom Summary
Cycle Timeline
Your tracked data will appear here as you record symptoms across cycles.
When the menstrual cycle throws off the body’s chemistry, many women notice a spike in mood swings, irritability, or outright panic. That surge isn’t random - it’s often the hallmark of Premenstrual Dysphoric Disorder (PMDD) intertwining with anxiety. Understanding why these two conditions co‑occur helps you spot warning signs early and choose the right treatment.
Quick Takeaways
- PMDD affects about 5‑8% of menstruating people and is strongly linked to heightened anxiety during the luteal phase.
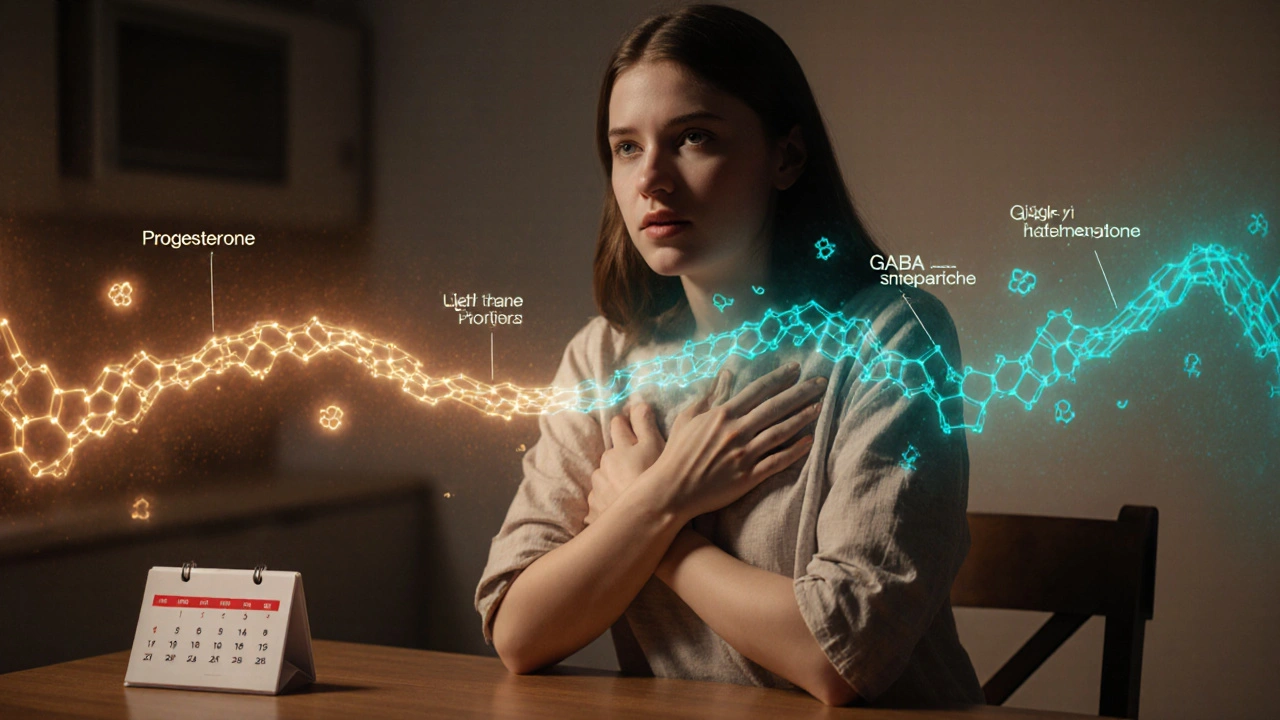
- Hormonal swings, especially progesterone and its metabolites, can disrupt serotonin and GABA pathways that regulate fear and stress.
- Symptoms overlap with Generalized Anxiety Disorder (GAD), making differential diagnosis essential.
- Evidence‑based treatments include SSRIs, cognitive‑behavioral therapy, and targeted lifestyle changes (diet, exercise, sleep hygiene).
- Tracking cycles with a symptom journal empowers you and your clinician to tailor interventions.
What Is Premenstrual Dysphoric Disorder?
Premenstrual Dysphoric Disorder is a severe form of premenstrual syndrome that causes emotional and physical symptoms that interfere with daily life. It typically emerges during the luteal phase (the two weeks after ovulation) and fades within a few days of menstruation. Key features include deep sadness, anger, anxiety, breast tenderness, and fatigue. Research from the International Society for Premenstrual Disorders (2023) estimates that up to 8% of women of reproductive age meet diagnostic criteria.
How Anxiety Fits Into the Picture
Anxiety is a natural response to perceived threat, marked by excessive worry, tension, and physical symptoms such as rapid heartbeat or shortness of breath. When anxiety spikes consistently in the days leading up to menstruation, clinicians often suspect a hormonal component. Studies published in the Journal of Affective Disorders (2024) show that women with PMDD are three times more likely to experience clinically significant anxiety compared to those without PMDD.
Hormonal Fluctuations and the Brain
During the luteal phase, progesterone rises sharply, then drops just before menstruation. Its metabolite, allopregnanolone, modulates the gamma‑aminobutyric acid (GABA) system-a major inhibitory pathway that calms neural excitement. When allopregnanolone levels fall, GABA activity can dip, leaving the brain more reactive to stress.
At the same time, estrogen’s ebb influences serotonin synthesis. Lower estrogen reduces tryptophan conversion to serotonin, weakening mood‑stabilizing signals. The combined dip in GABA and serotonin creates a perfect storm for anxiety symptoms.
Shared Neurochemical Pathways
- Serotonin: Both PMDD and anxiety disorders show altered serotonin transporter (SERT) density. SSRIs boost serotonin availability, which is why they work for both conditions.
- GABA: Allopregnanolone’s effect on GABA‑A receptors mirrors the action of some anti‑anxiety medications (e.g., benzodiazepines). A deficiency can heighten nervous system arousal.
- Stress Hormone (Cortisol): Chronic anxiety raises cortisol, which can aggravate menstrual cramps and mood swings, feeding back into PMDD severity.
Overlapping Symptoms: PMDD vs. Generalized Anxiety Disorder
| Feature | PMDD (Luteal Phase) | GAD (Any Time) |
|---|---|---|
| Onset Timing | 2-14 days before period | Persistent, >6 months |
| Core Anxiety | Feelings of tension, dread | Excessive worry about multiple domains |
| Physical Aches | Breast tenderness, bloating | Muscle tension, headaches |
| Mood Shifts | Irritability, tearfulness | Restlessness, irritability |
| Sleep Disruption | Insomnia during luteal phase | Difficulty falling or staying asleep |
Notice how PMDD’s symptoms cluster around the menstrual cycle, while GAD’s pattern is continuous. A detailed calendar can be the deciding factor for proper diagnosis.
Diagnosing the PMDD‑Anxiety Connection
- Gather a prospective symptom diary for at least two cycles. Record mood, anxiety intensity (0‑10 scale), sleep, appetite, and physical complaints.
- Use the DSM‑5‑TR criteria for PMDD (≥5 symptoms, including one mood symptom, present in the luteal phase).
- Screen for primary anxiety disorders using the GAD‑7 questionnaire. Scores ≥10 suggest moderate anxiety needing separate evaluation.
- Rule out medical confounders (thyroid disease, anemia, or chronic pain) through blood work.
- Collaborate with a gynecologist or psychiatrist experienced in female hormonal mental health.
When both sets of criteria are met, treatment must address the hormonal trigger *and* the anxiety circuitry.
Evidence‑Based Treatment Options
Because the neurobiology overlaps, many therapies help both PMDD and anxiety.
Selective Serotonin Reuptake Inhibitors (SSRIs)
SSRIs like fluoxetine, sertraline, and escitalopram are first‑line for PMDD. They can be taken continuously or in a “mini‑dose” schedule (only during the luteal phase). A 2022 meta‑analysis found a 70% response rate for anxiety reduction when SSRIs were used intermittently.
Cognitive‑Behavioral Therapy (CBT)
Cognitive‑Behavioral Therapy is a short‑term, goal‑oriented psychotherapy that teaches coping skills, thought restructuring, and exposure techniques. For PMDD‑related anxiety, CBT focuses on:
- Identifying cycle‑linked thought patterns (“I’m doomed because my period is near”).
- Developing relaxation scripts for the luteal phase.
- Building a graded exposure plan for anxiety‑provoking situations that worsen during menstruation.
Randomized trials show CBT adds a 15‑20% boost to medication response.
Lifestyle Modifications
- Nutrition: Low‑glycemic meals, omega‑3 fatty acids, and magnesium (400mg nightly) can stabilize neurotransmitters.
- Exercise: Moderate aerobic activity 3‑5 times a week lowers cortisol and improves GABA activity.
- Sleep Hygiene: Consistent bedtime, dim light exposure, and a cool bedroom help regulate melatonin, which interacts with estrogen.
- Stress Management: Mindfulness meditation (10min daily) reduces amygdala reactivity, a key anxiety hub.
Hormonal Treatments
For refractory cases, options include:
- Continuous combined oral contraceptives (COCs) that suppress ovulation, reducing luteal hormone spikes.
- Gonadotropin‑releasing hormone (GnRH) agonists, used short‑term under specialist care.
- Off‑label use of the neurosteroid brexanolone, a synthetic allopregnanolone analogue, which directly enhances GABA‑A receptors.
These interventions should be weighed against side‑effects like bone density loss or mood swings.
Managing Daily Life While Treatments Take Effect
Even with therapy, it can take 4‑6 weeks for symptom relief to become noticeable. Here are practical steps to keep functioning:
- Keep a digital symptom tracker (many apps sync with calendar alerts).
- Plan high‑stress tasks (presentations, exams) for the follicular phase when possible.
- Carry a “panic kit” - a small bottle of water, a calming essential oil (lavender), and a quick breathing script.
- Communicate with your support network: let a partner or coworker know you may need a short break during the luteal phase.
- Re‑evaluate treatment every three months with your clinician; adjust dose or timing based on diary trends.
Key Takeaway: The Cycle Is a Clue, Not a Curse
Seeing a pattern between your menstrual calendar and anxiety spikes turns a mysterious burden into a treatable condition. By combining medical therapy, psychotherapy, and smart lifestyle tweaks, most women regain control and reduce both PMDD and anxiety symptoms.
Frequently Asked Questions
Can PMDD cause panic attacks?
Yes. The rapid drop in allopregnanolone and serotonin during the luteal phase can trigger sudden surges of fear, leading to panic‑type episodes in up to 30% of women with PMDD.
Do birth control pills cure PMDD‑related anxiety?
Continuous‑use combination pills can smooth hormonal peaks, which often lowers anxiety scores. They’re not a cure for everyone, and side‑effects must be monitored.
Is it safe to take SSRIs only during the luteal phase?
Intermittent dosing is approved by the FDA for fluoxetine and sertraline. Many patients report fewer side‑effects while still achieving anxiety relief during the high‑risk window.
How long should I track my symptoms before seeing a doctor?
Two full cycles are the minimum for a reliable pattern. If symptoms are severe or disabling, seek help sooner rather than later.
Can lifestyle changes replace medication?
For mild cases, diet, exercise, and stress management can reduce both PMDD and anxiety enough to avoid meds. Moderate‑to‑severe cases typically benefit from a combined approach.



Megan Lallier-Barron
12 October 2025 - 05:03 AM
Hormones love drama, just like my ex 😒.
Kelly Larivee
15 October 2025 - 02:51 AM
Cool article, really breaks down the basics. The luteal phase stuff is something many folks overlook.
Emma Rauschkolb
18 October 2025 - 00:39 AM
Wow, the neurochemical cascade described here is like a full‑blown symphony of serotonin, GABA, and allopregnanolone 🎶. When those pathways mis‑fire, you get the classic PMDD‑anxiety overlap. Remember, the allostatic load can push you into a hyper‑vigilant state, making panic attacks feel inevitable. The article nails the mechanistic jargon, but don’t forget lifestyle modifiers – they’re the real MVPs. 😈
Kaushik Kumar
20 October 2025 - 22:27 PM
Hey there!! Great rundown!! You’ve captured the hormone‑brain link perfectly!! It’s so important to track those luteal swings – they really set the stage for anxiety spikes!! Keep sharing these insights!!
Mara Mara
23 October 2025 - 20:15 PM
While the science is solid, let’s not forget that many women are still dismissed by clinicians who underestimate hormonal contributions. It’s high time we demand comprehensive screening, not just a blanket “it’s anxiety”.
Jennifer Ferrara
26 October 2025 - 17:03 PM
Indeed, the prevailing clinical praxis oft neglects the cyclic interplay betwheen hormones and mood. A more holistic approach-incorporating both psychopharmacology and hormonal modulation-remains the gold standard. (Sorry for the typo above.)
Terry Moreland
29 October 2025 - 14:51 PM
I totally get how exhausting the cycle can be. If you’re tracking symptoms, try adding a quick 5‑minute breathing exercise each evening; it can calm the nervous system during the luteal phase.
Abdul Adeeb
1 November 2025 - 12:40 PM
The article correctly emphasizes the role of allopregnanolone in GABA modulation. However, it could benefit from a clearer distinction between continuous versus intermittent SSRI regimens.
Abhishek Vernekar
4 November 2025 - 10:28 AM
Good point about the SSRI schedules-just a reminder that proper dosing timing aligns with the luteal peak, otherwise you risk sub‑optimal symptom control.
Val Vaden
7 November 2025 - 08:16 AM
Nice summary, but honestly it feels like a rehash of stuff we already know. 🙄
lalitha vadlamani
10 November 2025 - 06:04 AM
One could argue that presenting this information without a critical lens perpetuates the myth that medication alone solves everything. A more balanced view is needed.
kirk lapan
13 November 2025 - 03:52 AM
Honestly, the majority of people just skim these articles and think "oh great, more pills". They don’t understand the nuanced interplay of neurosteroids – it’s not just about throwing SSRIs at the problem.
Vince D
16 November 2025 - 01:40 AM
Exactly, it’s a multi‑modal issue.
Ian Frith
18 November 2025 - 23:28 PM
Picture this: a woman standing at the edge of a stormy sea, each wave representing a hormonal surge, and the anxious mind trying to stay afloat. The article paints that tumult vividly, reminding us that PMDD isn’t just “bad mood” – it’s a physiological tempest that can overwhelm even the strongest psyche. By tracking the cycles, you essentially map the storm’s pattern, gaining the power to navigate it with the right tools – be it therapy, medication, or lifestyle tweaks. The science behind allopregnanolone is like discovering a hidden lever that can calm the waves. When that lever is missing, the brain’s GABA system feels the tremors, and anxiety spikes. The piece also rightly notes that serotonin pathways are compromised when estrogen dips, a cascade that many clinicians overlook. I’ve seen patients who, after logging their symptoms, finally convinced their doctors to try intermittent SSRIs, and the results were life‑changing. Remember, the luteal phase isn’t a curse; it’s a predictable phase that, once understood, can be managed. So keep the journals, talk openly with your provider, and never underestimate the power of a steady sleep schedule. Small habits compound into stability, turning the uncontrollable tides into something you can ride. In short: knowledge is the lighthouse, tracking is the map, and treatment is the vessel.
Beauty & Nail Care dublin2
21 November 2025 - 21:16 PM
Wow, the whole "hormones are secretly controlling us" narrative is a classic distraction 😏. While the article gives solid data, it conveniently ignores the big pharma agenda pushing SSRIs as the default. Remember, every time you dip into the luteal phase, the body’s trying to tell you something, not just “take a pill”. 👀
Oliver Harvey
24 November 2025 - 19:04 PM
Great read – except for the obvious omission of how lifestyle changes actually trump meds in many cases. 🙃
Ben Poulson
27 November 2025 - 16:52 PM
While the article presents a thorough overview, it would benefit from a more rigorous citation of primary research, particularly when discussing allopregnanolone’s pharmacodynamics.
Raghav Narayan
30 November 2025 - 14:40 PM
It is essential to recognize that PMDD and anxiety do not exist in a vacuum; they are embedded within a complex biopsychosocial framework. First, the neuroendocrine fluctuations that characterize the luteal phase precipitate alterations in serotonergic transmission, which in turn modulate the limbic system’s response to stressors. Second, the resultant dysregulation of the hypothalamic‑pituitary‑adrenal axis contributes to heightened cortisol secretion, further amplifying anxiety symptoms. Third, psychosocial factors such as work‑related stress, interpersonal conflicts, and cultural expectations can exacerbate the perceived severity of both mood and somatic complaints.
From a therapeutic perspective, a tiered approach yields the most robust outcomes. At the foundational level, lifestyle interventions-including regular aerobic exercise, omega‑3 fatty acid supplementation, and sleep hygiene-serve to stabilize neurochemical homeostasis. Building upon this, cognitive‑behavioral therapy provides patients with strategies to reframe catastrophic thoughts that often accompany the luteal surge. Finally, when these measures prove insufficient, pharmacologic options such as continuous‑use combined oral contraceptives or intermittent SSRIs should be considered, always with close monitoring for side‑effects.
Moreover, clinicians must employ a personalized symptom‑tracking regimen, encouraging patients to log mood, anxiety intensity, sleep quality, and physical symptoms across multiple cycles. This longitudinal data not only facilitates accurate diagnosis but also empowers patients to recognize patterns, thereby fostering self‑efficacy. In conclusion, the integration of neurobiological insight, psychosocial awareness, and individualized treatment plans constitutes the gold standard for managing the PMDD‑anxiety nexus.
Tara Phillips
3 December 2025 - 12:28 PM
Take heart – with disciplined tracking and a proactive care plan, you can reclaim control over those cyclical anxiety spikes.
Derrick Blount
6 December 2025 - 10:16 AM
One might argue that the very act of chronic symptom logging transforms the patient from passive sufferer to active researcher, thereby altering the neurochemical feedback loop itself; indeed, consciousness of one’s own physiological rhythms may modulate GABAergic tone via top‑down mechanisms, a hypothesis that warrants empirical exploration.