Hyperkalemia Treatment Calculator
This tool helps determine appropriate hyperkalemia treatment based on your potassium level, ECG findings, and kidney function. Hyperkalemia (high blood potassium) can cause life-threatening heart arrhythmias.
When your blood potassium levels climb too high, your heart doesn’t just skip a beat-it can stop. This isn’t theoretical. Every year, thousands of people on common heart and kidney medications develop hyperkalemia, a condition where potassium in the blood rises to dangerous levels. Many don’t feel anything at first. No chest pain. No dizziness. Just a quiet, invisible threat building inside them. By the time symptoms show up, it’s often too late. But here’s the real problem: the very drugs saving their lives-medications for high blood pressure, heart failure, or kidney disease-are the ones putting them at risk.
What Exactly Is Hyperkalemia?
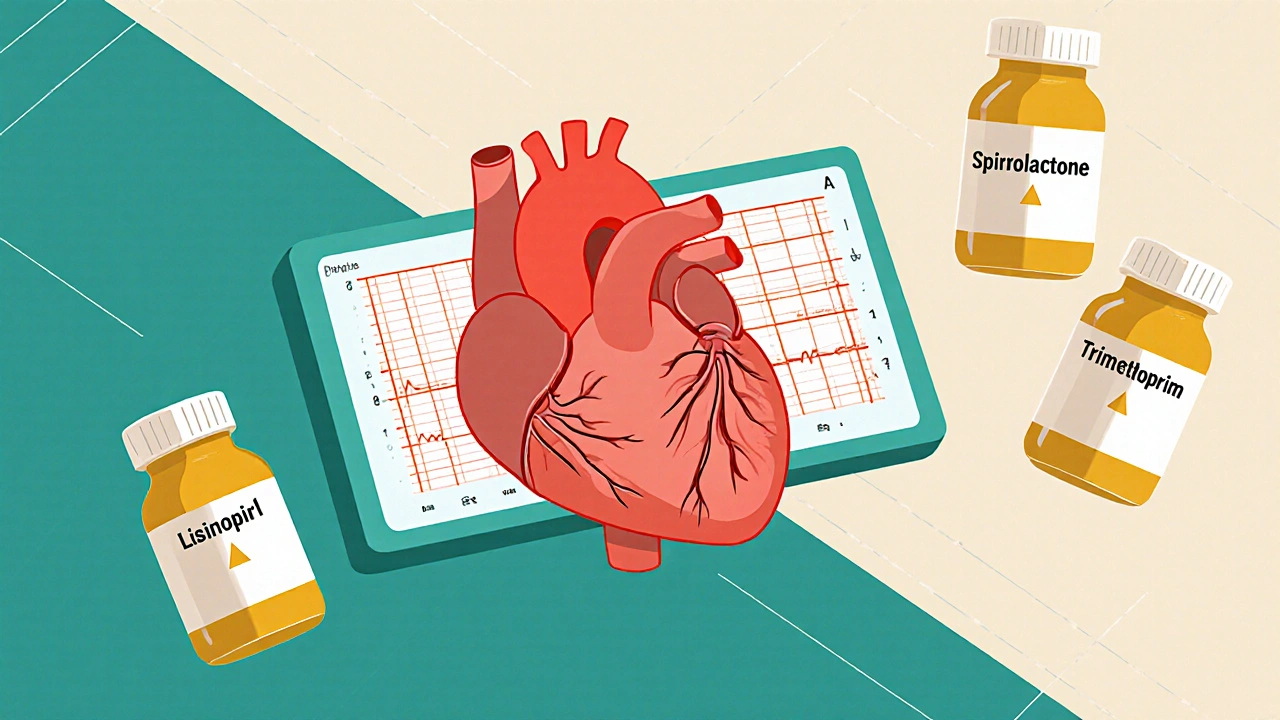
Hyperkalemia means your blood potassium level is above 5.5 mEq/L. Normal is between 3.5 and 5.0. Levels between 5.5 and 6.5 mEq/L are considered moderate. Above 6.5? That’s a medical emergency. At 7.0 or higher, your heart’s electrical system starts to fail. You won’t always feel it. Some people have no symptoms until their ECG shows dangerous changes: tall, peaked T-waves, widened QRS complexes, or worse-a sine wave pattern that precedes cardiac arrest. The scary part? This isn’t rare. In the general population, about 2-3% have hyperkalemia. But among people taking RAAS inhibitors-like lisinopril, losartan, or spironolactone-that number jumps to 10-20%. In hospitals, it’s even higher. One in ten hospitalized patients develops it. And most of them didn’t even know they were at risk.Which Medications Cause It?
It’s not just one drug. It’s combinations. The biggest culprits are medications that protect your heart and kidneys but also block potassium from leaving your body:- ACE inhibitors (lisinopril, enalapril)
- ARBs (losartan, valsartan)
- Mineralocorticoid receptor antagonists (spironolactone, eplerenone)
- Potassium-sparing diuretics (amiloride, triamterene)
- Direct renin inhibitors (aliskiren)
Why Your Heart Is at Risk
Potassium controls how your heart muscle cells recharge between beats. Too much potassium makes these cells too easy to trigger. They fire off randomly. Your heart rhythm goes haywire. That’s when you get arrhythmias-fluttering, racing, or chaotic beats that can turn into ventricular fibrillation, a deadly rhythm where the heart quivers instead of pumping. The ECG tells the story before symptoms do:- 5.5-6.5 mEq/L: Peaked T-waves (the first warning sign)
- 6.5-7.5 mEq/L: Prolonged PR interval, flattened P-waves
- 7.5+ mEq/L: Widened QRS complex, sine wave pattern

Treatment: What to Do When Potassium Spikes
If your potassium hits 6.5 mEq/L or higher-or you have ECG changes-you need treatment now. It’s not about lowering potassium right away. It’s about protecting your heart while you do. Step 1: Stabilize the heart - Give 1-2 grams of calcium gluconate intravenously. This doesn’t lower potassium. It just makes heart cells less likely to misfire. Effects start in 2-3 minutes. This is non-negotiable if ECG changes are present. Step 2: Shift potassium into cells - Two tools do this fast:- 10 units of insulin + 25 grams of glucose (lowers potassium by 0.5-1.5 mEq/L in 15-30 minutes)
- Albuterol via nebulizer (50-100 mcg, lowers potassium by 0.5-1.0 mEq/L)
- Loop diuretics (furosemide) if kidneys are still working
- Dialysis if you’re on it or kidney failure is severe
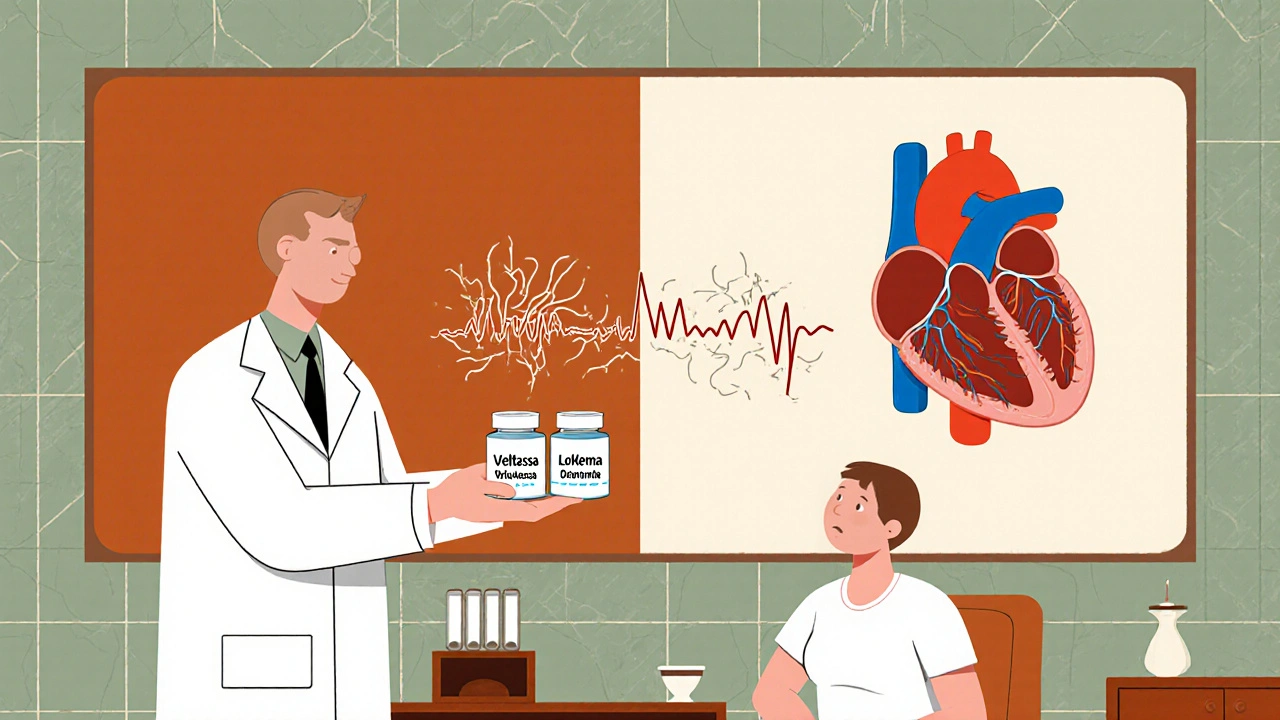
- Patiromer (Veltassa): 8.4-25.2 grams daily. Lowers potassium by 0.4-1.0 mEq/L. Common side effect: constipation (15-20% of users).
- Sodium zirconium cyclosilicate (Lokelma): 5-10 grams daily. Works faster-within hours. Side effects: diarrhea (10-15%), bloating.
Managing Hyperkalemia Long-Term
If you’re on a RAAS inhibitor and have kidney disease or diabetes, you need a plan-not just a reaction.- Monitor regularly: Check potassium every 1-4 weeks, especially after starting or changing meds.
- Watch your diet: Limit high-potassium foods-bananas, oranges, potatoes, tomatoes, spinach, beans, nuts. Aim for 2,000-3,000 mg per day. Most people don’t realize how easy it is to overshoot.
- Review all meds: Over-the-counter salt substitutes? Many are pure potassium chloride. Herbal supplements like licorice root? Can mess with aldosterone. Even some antacids contain potassium.
- Stay hydrated: Dehydration concentrates potassium in your blood. Drink enough water, especially in hot weather or after exercise.
The New Standard of Care
Ten years ago, the answer to hyperkalemia was simple: stop the drug. Today, it’s not. With potassium binders, we can keep patients on their life-saving meds. The National Kidney Foundation and American Heart Association now recommend binders as first-line for chronic hyperkalemia in patients who need RAAS inhibitors. This shift matters. Modeling studies suggest that if we reduce RAAS inhibitor discontinuation by half, we could cut major heart events in high-risk patients by 20-25%. That’s thousands of lives saved each year. The challenge? Many doctors still don’t know how to use binders. Many patients don’t know they exist. And too many pharmacies still treat them as “specialty” drugs-hard to get, expensive, confusing.What You Can Do Right Now
If you’re on any of these medications:- Ask your doctor for a recent potassium test. If it’s been over 3 months, request one.
- Ask: “Could my meds be raising my potassium? Should I be on a binder?”
- Don’t assume “no symptoms” means “no problem.”
- Keep a food log for a week. You might be surprised how many high-potassium foods you’re eating.
- If you’re prescribed a binder, take it exactly as directed. It won’t work if you skip doses.
Can high potassium from meds be reversed?
Yes, but how fast depends on severity. For mild cases, stopping the culprit medication and adjusting diet can bring levels down in days. For moderate to severe cases, you need medical treatment: calcium to protect the heart, insulin and albuterol to shift potassium into cells, and potassium binders or dialysis to remove it from the body. Without treatment, high potassium can be fatal.
Can I still take my blood pressure medicine if I have high potassium?
Absolutely-if you use a potassium binder. Medications like ACE inhibitors and ARBs are critical for protecting your heart and kidneys, especially if you have diabetes or chronic kidney disease. Stopping them increases your risk of heart attack, stroke, and kidney failure. Potassium binders like Lokelma or Veltassa let you keep taking these drugs safely. Many patients now stay on their meds long-term with this approach.
What foods should I avoid with high potassium?
Avoid or limit bananas, oranges, potatoes, tomatoes, spinach, avocados, beans, lentils, nuts, dried fruit, and salt substitutes. Even one banana can add 400-500 mg of potassium. A cup of orange juice has nearly 500 mg. If you’re on a potassium-restricted diet, aim for under 3,000 mg per day. Use a food tracking app or ask a dietitian for a low-potassium meal plan.
Do potassium binders have side effects?
Yes. Patiromer (Veltassa) commonly causes constipation (15-20% of users). Sodium zirconium cyclosilicate (Lokelma) can cause diarrhea (10-15%) or bloating. Both are generally well-tolerated, but side effects can be managed. Take them as directed-usually with food and separated from other meds by a few hours. If side effects are severe, talk to your doctor about switching binders.
How often should I get my potassium checked?
If you’re on RAAS inhibitors and have kidney disease, diabetes, or are over 65, check your potassium every 1-4 weeks after starting or changing meds. Once stable, every 3 months is usually enough. If you’re on a potassium binder, check every 2-4 weeks initially, then every 3-6 months. Never skip these tests-even if you feel fine.





Adrian Rios
22 November 2025 - 18:38 PM
Man, I didn’t realize how many of my meds could silently wreck my heart like this. I’m on lisinopril and spironolactone for my BP and heart failure-never thought about potassium until my doc mentioned it last month. I thought fatigue was just aging. Turns out, I was one banana away from a cardiac event. Now I’m on Lokelma, cut out orange juice, and check my levels every 3 weeks. This post literally saved my life. Thanks for laying it out so clearly.
Casper van Hoof
24 November 2025 - 12:36 PM
The philosophical underpinning of this clinical reality is fascinating: we have engineered interventions to prolong life, yet inadvertently constructed a paradox wherein the very mechanisms designed to preserve cardiac integrity become the agents of its potential collapse. This is not merely pharmacological side effect; it is a metaphysical tension between therapeutic intent and physiological consequence.
Richard Wöhrl
24 November 2025 - 23:21 PM
Important clarification: calcium gluconate doesn’t lower potassium-it just stabilizes the myocardial membrane. Many people confuse this. Also, insulin+glucose? Always give it with dextrose to prevent hypoglycemia. And don’t forget: albuterol works best when nebulized, not inhaled via MDI. And yes-potassium binders are game-changers. I’ve seen patients go from stopping ACEi to thriving on full RAAS blockade with patiromer. But they need to be taken 30 mins before food, and spaced 2+ hours from other meds. Don’t just pop them with your coffee.
Pramod Kumar
25 November 2025 - 21:51 PM
Bro, this is wild. In India, we treat hypertension like it’s just a number to crush-not a living system. My uncle died last year from this exact thing. Doc said ‘just stop the pill,’ but he didn’t tell him about binders. Now his widow’s crying over a prescription she never knew existed. We need to talk about this in villages, not just hospitals. Potassium isn’t the enemy. Ignorance is.
Brandy Walley
27 November 2025 - 04:37 AM
So basically, doctors are poisoning people to save them? Cool. I'm just gonna stop all meds and eat kale. Maybe I'll live longer. Also, 'Lokelma'? Sounds like a crypto coin. Who even made this stuff?
shreyas yashas
27 November 2025 - 13:40 PM
My dad’s on lisinopril. He’s 72, diabetic, CKD stage 3. Doc never mentioned potassium. We found out after he got dizzy and his ECG looked like a heart attack. Turned out his K+ was 6.8. Scared the hell out of us. Now he’s on Veltassa and avoids bananas like they’re snakes. I wish we’d known sooner. This post is a gift.
Lisa Lee
28 November 2025 - 22:27 PM
Why are we even using these American drugs? In Canada, we use safer alternatives. This whole thing is just Big Pharma selling expensive binders because they can. Just stop the meds. Done. Problem solved. No magic pills needed.
JD Mette
30 November 2025 - 17:40 PM
I’ve seen this happen too. Patient came in with no symptoms, ECG showed sine wave. Calcium gluconate saved him. He was on three meds that raised potassium. We started him on Lokelma, and now he’s hiking every weekend. It’s not about fear-it’s about awareness. Thank you for writing this.
Dalton Adams
1 December 2025 - 06:55 AM
Let’s be real: if you’re on RAAS inhibitors and you’re not monitoring potassium, you’re not a patient-you’re a liability. Also, patiromer is superior to Lokelma because it has a longer half-life and better adherence rates. And if you’re eating spinach and oranges on a low-potassium diet, you’re doing it wrong. I’ve read the NKF guidelines. You haven’t. Don’t pretend you know what you’re talking about.
Matthew Mahar
2 December 2025 - 03:40 AM
I’ve been on spironolactone for 8 years. Never knew potassium could kill me like this. I thought it was just a water pill. Now I check my levels every month. I even use a food tracker. I used to eat 3 bananas a day. Now? One every other week. My heart feels better. I’m not scared anymore. Just informed.
John Mackaill
3 December 2025 - 04:07 AM
My GP didn’t even mention potassium when I started my ACE inhibitor. I had to Google it myself. Now I’m on Veltassa and feel like I’ve been given back my life. The real tragedy isn’t the condition-it’s how little we’re told. This needs to be standard info on every prescription bottle.
Katy Bell
3 December 2025 - 23:21 PM
My mom’s on all the meds listed. She’s 78. We just started her on Lokelma last month. She hates the taste but takes it. I made her a little chart: ‘No bananas. No salt substitute. Check K+ every 4 weeks.’ She’s been doing great. This post made me cry. I didn’t know how close we were to losing her.
Ragini Sharma
4 December 2025 - 19:36 PM
so like… potassium binders are just fancy poop pills? lol. my auntie takes one and says it makes her feel like a balloon. but hey, at least she’s not dead. also, why is everyone so obsessed with bananas? i eat em all the time and my k+ is fine. maybe my kidneys are just cooler than yours 🤷♀️