When women hit the menopause the natural transition that ends menstrual cycles, usually occurring between ages 45 and 55, they often notice new swelling in ankles, feet, or hands. That puffiness is most commonly edema the accumulation of excess fluid in the body’s tissues, and while it can feel harmless, it sometimes signals deeper hormonal or circulatory shifts.
Quick Takeaways
- Hormonal decline, especially lower estrogen the primary female sex hormone that helps regulate fluid balance, is a leading trigger for menopause edema.
- High dietary sodium a mineral that retains water in the bloodstream, medication side‑effects, and reduced blood pressure the force exerted by circulating blood on vessel walls control can all worsen swelling.
- Typical symptoms include puffy ankles after a day of standing, tight‑feeling hands, and a sudden weight jump of 2-5lb.
- Management blends diet tweaks, regular movement, compression wear, and-when needed-short‑term diuretics medications that help the kidneys expel excess fluid.
- Seek medical advice if swelling is painful, appears suddenly, or comes with shortness of breath.
Why Edema Shows Up During Menopause
The drop in estrogen estrogen levels typically fall by 70-80% during the menopausal transition disrupts the body’s ability to manage sodium and water. Estrogen normally promotes the production of nitric oxide, a molecule that keeps blood vessels relaxed and helps kidneys flush out excess fluid. Without that protective effect, blood vessels can become slightly tighter, and the kidneys retain more sodium, leading to fluid buildup.
Besides hormones, menopause often coincides with lifestyle shifts-less regular exercise, higher stress, or weight gain-that further strain the circulatory system. Even common prescriptions for hot flashes or bone health (like certain selective estrogen receptor modulators) can have fluid‑retaining side effects.
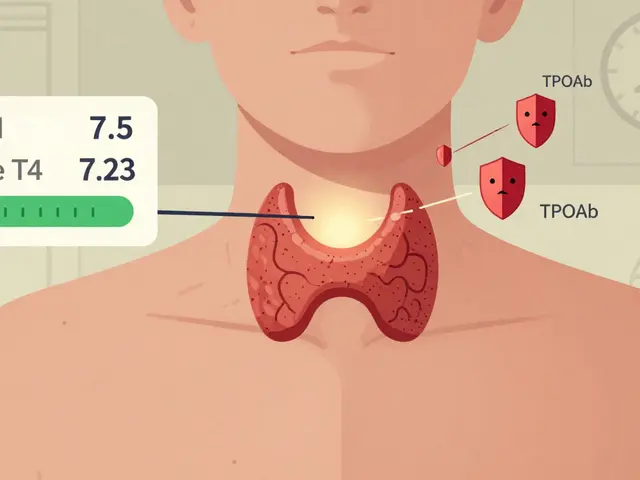
Hormonal Influence on Fluid Balance
Estrogen interacts with the renin‑angiotensin‑aldosterone system (RAAS), the hormone cascade that regulates blood volume. When estrogen drops, RAAS activity tends to rise, prompting the kidneys to retain sodium and water. Simultaneously, lower estrogen reduces the production of atrial natriuretic peptide (ANP), a hormone that tells the kidneys to excrete excess fluid. The combined effect is a subtle but steady shift toward fluid retention.
Progesterone, another hormone that wanes during menopause, also plays a role. It normally antagonizes aldosterone, the hormone that tells the kidneys to hold onto salt. With less progesterone, aldosterone’s grip strengthens, further encouraging fluid buildup. Understanding these intertwined pathways helps explain why simple sodium cuts or a short walk sometimes make a big difference.
Common Triggers of Menopausal Edema
| Cause | How it works | Typical Management |
|---|---|---|
| Estrogen decline | Reduces nitric‑oxide mediated vasodilation, increases sodium reabsorption | Phyto‑estrogen‑rich foods, hormone therapy (if appropriate) |
| High sodium intake | Encourages water retention in bloodstream | Limit processed foods, choose potassium‑rich alternatives |
| Elevated blood pressure | Raises hydrostatic pressure in capillaries, pushes fluid into tissues | Regular BP monitoring, ACE inhibitors or lifestyle control |
| Medications | Some antidepressants, NSAIDs, and calcium channel blockers impede fluid excretion | Review meds with doctor, consider alternatives |
| Venous insufficiency | Veins struggle to return blood from lower limbs, causing pooling | Compression stockings, leg‑raising exercises |
| Weight gain & inactivity | Extra tissue compresses vessels, slows circulation | Daily walking, strength training, mindful eating |

Spotting the Symptoms Early
Not every puffiness is worrisome, but paying attention can prevent complications. Look for these tell‑tale signs:
- Puffy ankles or calves that feel tight by evening and improve after lying down.
- Swollen fingers that make rings feel snug.
- A sudden, unexplained weight increase of more than 2lb within a week.
- Skin that, when pressed, leaves a dent (called “pitting”) that slowly fills back.
- Shortness of breath or chest discomfort accompanying swelling-these demand immediate medical review.
Hands‑On Management Strategies
Most women can tame menopause‑related edema with a blend of everyday tweaks and, if needed, medical support.
1. Adjust Your Diet
- Cut processed snacks, canned soups, and salty sauces. Aim for less than 1,500mg of sodium per day.
- Boost potassium an electrolyte that helps cells expel sodium and reduces fluid retention-rich foods-bananas, oranges, sweet potatoes, and leafy greens-to help the kidneys flush excess salt.
- Stay hydrated. Drinking 8‑10 glasses of water encourages kidneys to flush excess sodium.
- Limit alcohol and caffeine, which can aggravate dehydration and hormonal swings.
2. Keep Moving
Even a 15‑minute walk after meals can stimulate the calf muscle pump, pushing fluid back toward the heart.
- Incorporate calf raises: stand on a step, rise onto toes, lower slowly-3 sets of 15 reps.
- Try low‑impact cardio (swimming, cycling) 3-4 times a week.
- Take “leg‑up” breaks at work: sit, lift legs on a stool for 5 minutes every hour.
3. Wear Compression Stockings
Graduated compression (15‑20mmHg) gently squeezes the lower leg, preventing fluid from pooling. Look for breathable, knee‑high options for daily wear. The gentle pressure is especially helpful during long flights or standing shifts.
4. Review Medications
Talk to your clinician about any drugs that might retain water. Sometimes switching from an NSAID to acetaminophen, or adjusting a blood pressure pill, makes a noticeable difference.
5. Consider Hormone Therapy (HT)
For women with severe symptoms, low‑dose estrogen‑progestin therapy can restore vascular health. HT isn’t right for everyone; a risk‑benefit discussion with a health professional is essential.
6. Use Short‑Term Diuretics Carefully
Prescription diuretics like thiazides can alleviate swelling, but they also deplete electrolytes. Only use them under a doctor’s supervision and pair with potassium‑rich foods.
7. Monitor and Document
Keep a simple log: record daily weight, ankle circumference (measure at the widest point), and foods consumed. Patterns often reveal trigger foods or activity gaps.
When to Seek Professional Help
- Painful swelling that doesn’t improve with elevation.
- Sudden, severe swelling in one leg only-possible deep‑vein thrombosis.
- Shortness of breath, coughing, or wheezing.
- Swelling accompanied by fever or skin redness.
- Persistent edema despite lifestyle changes for more than three weeks.
Quick Lifestyle Checklist
- Limit sodium to ≤1,500mg/day.
- Drink at least 2L of water daily.
- Walk or stretch for 10 minutes after each meal.
- Wear compression stockings during long standing periods.
- Track weight and ankle measurements weekly.
- Review meds with pharmacy annually.
- Sleep with legs slightly elevated (use a pillow).

Frequently Asked Questions
Can menopause cause swelling only in the legs?
Leg swelling is the most common sign because gravity pulls fluid down, but many women also notice puffiness in the hands, abdomen, or even the face. The distribution often depends on personal circulation patterns and activity level.
Is it safe to use over‑the‑counter diuretics?
Most OTC “water pills” contain caffeine or herbal extracts that can interact with prescription meds or raise blood pressure. Always check with a pharmacist or physician before starting any diuretic, even if it’s labeled “natural”.
How much exercise is enough to reduce edema?
Aim for at least 150 minutes of moderate aerobic activity per week-think brisk walking, swimming, or cycling. Adding brief calf‑raise sets during the day can provide an extra boost for fluid return.
Can hormone replacement therapy eliminate edema?
HT can improve vascular tone and reduce sodium retention for many women, but results vary. It’s not a guaranteed fix, and the decision must weigh heart, bone, and cancer risk factors.
What foods help flush excess fluid?
Cucumbers, watermelon, celery, and citrus fruits have high water content and potassium, which encourage the kidneys to release extra sodium. Pair them with a pinch of magnesium‑rich nuts for balanced electrolytes.






April Barrow
29 September 2025 - 11:33 AM
Been dealing with this since my 48th birthday. The ankle swelling was so bad I thought I was pregnant again. Turns out it was just estrogen dropping. Cut out the soy sauce and started walking after dinner-big difference. No magic pill, just small consistent changes.
Also, compression socks are a game changer. I wear them even to bed sometimes.
Melody Jiang
30 September 2025 - 01:06 AM
It’s fascinating how the body tries to adapt when the hormonal landscape shifts. Estrogen isn’t just about reproduction-it’s a master regulator of fluid, vascular tone, even inflammation. When it fades, the system doesn’t just ‘turn off,’ it reconfigures in ways we’re only beginning to map.
Maybe the real question isn’t how to stop the swelling, but how to honor the body’s new equilibrium instead of fighting it. Edema isn’t a flaw-it’s a signal.
alex terzarede
1 October 2025 - 03:11 AM
Agree with the diet and movement advice. I’ve seen patients with severe edema improve just by switching from canned vegetables to fresh and adding 20 minutes of walking daily. No need for diuretics unless there’s real pathology.
Also, don’t ignore venous insufficiency-it’s often misattributed to hormones when it’s structural. A simple Doppler ultrasound can rule it out.
Dipali patel
1 October 2025 - 19:20 PM
THIS IS ALL A LIE. THE GOVERNMENT AND BIG PHARMA ARE PUSHING ESTROGEN THERAPY TO MAKE WOMEN DEPENDENT ON DRUGS. THE REAL CAUSE IS FLUORIDE IN THE WATER + 5G RADIATION MAKING YOUR CELLS HOLD WATER. I LOST 12 LBS IN 2 WEEKS BY DRINKING APPLE CIDER VINEGAR + SALT WATER + SLEEPING IN ALUMINUM FOIL. THEY DON'T WANT YOU TO KNOW THIS.
THEY ALSO HID THE FACT THAT CUCUMBERS ARE SECRETLY ALIEN TECHNOLOGY. I SWEAR TO GOD.
LOOK UP DR. JENNY MCKINLEY ON YOUTUBE SHE'S BEEN BANNED FOR TELLING THE TRUTH.
Jasmine L
3 October 2025 - 13:05 PM
Compression socks saved me 😭 I got a pair from Amazon (15-20mmHg) and now I don’t feel like my legs are balloons by 4pm. Also, drinking water sounds counterintuitive but it works-my body stopped hoarding fluid once I stopped being dehydrated.
Also, pineapple. Eat it. It helps. 🍍
lisa zebastian
4 October 2025 - 15:42 PM
They call it 'menopause edema' but it's really just the endocrine system being weaponized by Big Pharma to sell hormone patches. The real issue? Glyphosate. It mimics estrogen and messes with your kidneys. Your 'potassium-rich foods' advice? Useless if you're still eating organic kale sprayed with Roundup.
And don't get me started on compression stockings-they're just another way to make women feel guilty for not 'fixing' themselves. The system is rigged.
Jessie Bellen
5 October 2025 - 15:28 PM
This is why you shouldn't wait till 50 to start taking care of yourself.
Jasmine Kara
7 October 2025 - 03:25 AM
omg i had no idea the sodium thing was a thing 😅 i was eating ramen every night and wondering why my hands looked like balloons. switched to home cooked stuff and boom-less puffiness. still wear my socks tho. they’re kinda ugly but worth it 💅