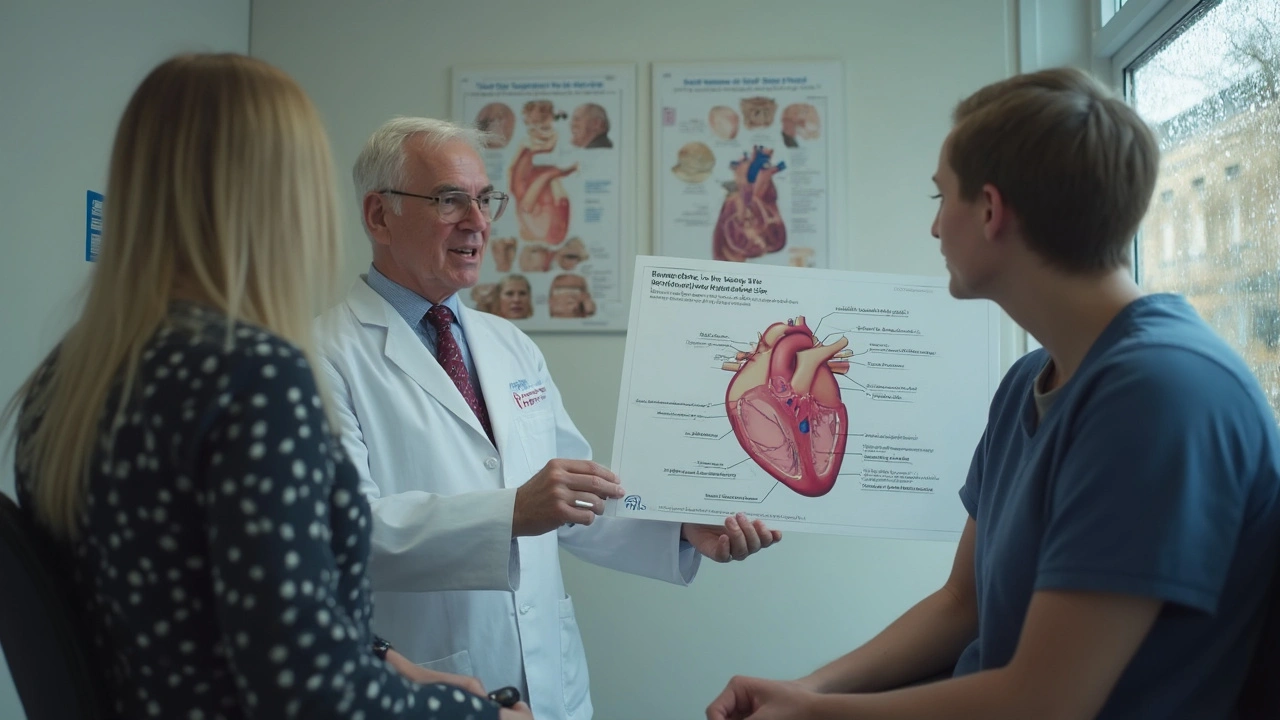
The mention of beta-blockers probably sounds familiar if you’ve ever talked to a doctor about heart issues. These meds have changed the game for people with left ventricular dysfunction, especially folks managing heart failure. But what do they actually do, and why do they matter so much?
If your left ventricle—the main pumping chamber of your heart—starts to slack off, it can't move blood around your body like it should. That sets off a domino effect: you might get tired, short of breath, or even wind up in the hospital.
Here’s the interesting part: beta-blockers don’t just fix symptoms for a few hours. They protect your heart over the long haul, lowering your risk of landing in the ER again or even dying from heart failure. But not every beta-blocker is made the same, and not every patient gets the same benefits. That’s why it’s key to know what these drugs actually do inside your body and how you can get the most mileage out of them.
- What Is Left Ventricular Dysfunction?
- How Beta-Blockers Work
- Who Should Take Beta-Blockers?
- Tips for Safe Use and Managing Side Effects
- Debunking Myths and Real-Life Stories
What Is Left Ventricular Dysfunction?
Let's get straight to the point: left ventricular dysfunction means your heart’s main pumping chamber doesn’t work like it should. The left ventricle’s job is to pump oxygen-rich blood to your entire body. When it starts to struggle, the whole system takes a hit. Think of it like a water pump that can’t keep up—everything downstream suffers.
This problem usually shows up as heart failure, which is a term that covers several different issues. With left ventricular dysfunction, the most common type is called systolic dysfunction. That means the ventricle can’t contract well enough to push blood out. It’s usually measured by something called “ejection fraction”—a percentage that shows how much blood pumps out with each beat. A normal ejection fraction is 55-70%. If yours drops below 40%, doctors know you’ve got a real problem on your hands.
| Ejection Fraction (%) | What It Means |
|---|---|
| 55-70 | Normal |
| 41-54 | Borderline |
| 40 or less | Left Ventricular Dysfunction |
Symptoms can sneak up on you, or they can hit fast. People might feel breathless walking to the mailbox, or even lying in bed. Fatigue, swelling in the ankles, trouble sleeping flat—these all point to your heart not keeping up. But here’s the frustrating part: sometimes, people don’t notice anything at all until things get bad.
According to the American Heart Association,
"Left ventricular dysfunction is one of the most common reasons for heart failure hospitalizations worldwide."That’s how serious it is. And while high blood pressure, diabetes, or past heart attacks all pile on the risk, even younger adults aren’t totally off the hook. Genetics, viral infections, or even certain cancer treatments can put a person on the fast-track to trouble.
Spotting left ventricular dysfunction early is key. Getting an echocardiogram (an ultrasound of the heart) is usually how doctors confirm the diagnosis. If you have a family history of heart issues or any of the symptoms above, talking to your doctor sooner rather than later could save a lot of hassle—and maybe your life.
How Beta-Blockers Work
If your doctor talks about beta-blockers, they're talking about a group of meds that calm down your heart. They do this by blocking certain chemical signals—namely adrenaline and noradrenaline—from attaching to beta-receptors in your heart and blood vessels. What happens next is pretty simple: your heart beats slower and with less force. This takes the edge off the workload for your left ventricle.
For people with left ventricular dysfunction, that’s huge. Letting the heart chill out lowers blood pressure, which helps prevent the heart from getting even weaker. Over time, beta-blockers can even help the heart pump better and may reverse some of the changes that come with heart failure. It’s not about instant results—think of it more like giving your heart long-term support and protection.
Some beta-blockers are proven winners: drugs like carvedilol, metoprolol succinate, and bisoprolol have a track record in serious studies for reducing hospital visits and pushing survival rates higher. Not every beta-blocker is a magic bullet though. Only certain ones are recommended if you’ve got heart failure with reduced pumping action.
- Slows heart rate: This gives the heart more time to fill and pump better.
- Lowers blood pressure: Less pressure means less strain on the heart muscle.
- Shields against more damage: Reduces the risk of future heart issues.
Check out this quick comparison of the top three beta-blockers shown to help with left ventricular dysfunction:
| Beta-Blocker | Main Benefit for Left Ventricle | Dosing Notes |
|---|---|---|
| Carvedilol | Improves survival, lowers blood pressure | Start low, double dose every 2 weeks if tolerated |
| Metoprolol succinate | Improves symptoms and survival | Extended-release form, increase slowly |
| Bisoprolol | Boosts heart function, lowers hospital visits | Titrate up carefully |
To get the most from beta-blockers, it’s all about steady and slow increases in dose (doctors call this titration). That helps avoid major dips in blood pressure or heart rate, and gives your body time to adjust. It’s a balancing act, but it pays off if you stick with the plan.
Who Should Take Beta-Blockers?
This is the million-dollar question: who actually needs beta-blockers if they have left ventricular dysfunction? It’s not everybody, but the group that benefits is pretty big.
Doctors usually recommend beta-blockers for people with left ventricular ejection fraction (LVEF) under 40%. If that sounds technical, picture this—your heart isn't pumping out at least 40% of the blood with each beat. This includes anyone diagnosed with heart failure with reduced ejection fraction (HFrEF). For these folks, taking beta-blockers can seriously cut the risk of hospital visits and even lower the chance of dying from heart issues.
But not everyone with heart problems jumps into beta-blocker therapy right away. There are some exceptions, like people who have very slow heart rates (bradycardia), severe asthma, or certain forms of heart block. Doctors will often avoid or carefully adjust beta-blockers for these patients, since the side effects could do more harm than good.
Here’s a quick breakdown of who usually gets put on beta-blockers for heart failure or left ventricular dysfunction:
- Patients with LVEF ≤ 40%. This is the main group in big clinical guidelines.
- Anyone with a history of heart attack who also has signs of heart failure — beta-blockers can help prevent another major event.
- People who feel symptoms like shortness of breath, swelling, or constant tiredness related to their failing heart.
- Some folks with high blood pressure and other heart conditions, even if their main problem isn't heart failure yet.
Here’s a stat worth knowing: in studies like MERIT-HF and CIBIS-II, adding a beta-blocker to standard heart failure treatment dropped hospital admissions and deaths by up to 30%. That’s a big deal and why these meds are so common in heart care.
| Group | Should Take Beta-Blocker? | Key Benefit |
|---|---|---|
| Low LVEF (≤40%) | Yes | Slows heart failure, cuts hospital stays |
| Heart Attack Survivors with LV Dysfunction | Yes | Reduces risk of repeat events |
| Bradycardia or Severe Asthma | No (or with caution) | Avoid major side effects |
Bottom line? If you fall into one of these groups, beta-blockers can make a real difference. Always get your heart checked, and talk openly with your doctor about your symptoms and other medical issues before starting these meds.
Tips for Safe Use and Managing Side Effects
Sticking with beta-blockers can make a major difference in your journey with left ventricular dysfunction, but you have to play it smart. Here’s what works in real life.
Always take the meds exactly as your doctor says. These aren’t the kind you can just skip for a few days and pick up again. Suddenly stopping can send your heart racing or make symptoms worse, especially if you’ve been on them for a while. If you forget a dose, don’t double up—just take the next scheduled one and let your doctor know.
Side effects with beta-blockers are common in the first couple of weeks, but most people adjust. You might feel tired, a bit dizzy, or notice your hands and feet get colder than usual. Here’s what helps:
- Take the medicine at the same time every day, with food if it upsets your stomach.
- Stand up slowly if you feel dizzy, especially when you first start or after increasing your dose.
- Check your pulse and blood pressure at home—if they dip too low, contact your doctor.
- Keep your doctor in the loop about any breathing changes, since beta-blockers can bring out asthma symptoms in rare cases.
- Mention all your current medications and supplements—some mix badly with beta-blockers. Over-the-counter cold medicines are a sneaky problem for some folks.
Want the numbers? About 60% of people with heart failure feel side effects at first, but only about 10% end up needing a switch to a different beta-blocker or another kind of medication. Usually, starting with a low dose and slowly increasing helps your body get used to the change.
| Common Side Effect | How Often It Happens |
|---|---|
| Tiredness | Up to 30% |
| Dizziness | 15-20% |
| Cold hands/feet | 10-15% |
| Worse breathing | Below 5% |
If you get worried about anything—from feeling extra sluggish to running out of pills—reach out to your health team fast. A quick check-in or dose adjustment can usually get you back on track without major drama.
Debunking Myths and Real-Life Stories
You’ve probably heard a few things about beta-blockers and might be wondering what’s legit and what’s just rumor. Let’s break down some of the biggest myths and add a few real stories from folks who’ve actually lived with left ventricular dysfunction.
Myth #1: Beta-blockers are dangerous for everyone with heart problems.
This old idea just doesn’t hold up. There was a time when people thought beta-blockers could make heart failure worse. But now, heart specialists count on them to actually help stabilize the heart. The trick is starting with a low dose and slowly increasing. Major studies like CIBIS-II and MERIT-HF proved that people with heart failure who took beta-blockers were much less likely to die or be hospitalized compared to those who didn’t take them.
Myth #2: All beta-blockers are basically the same.
This one gets people tripped up. Some beta-blockers aren’t great for treating left ventricular dysfunction. Doctors mostly use carvedilol, bisoprolol, and metoprolol succinate for heart failure because these actually improve how well the heart works. Other beta-blockers might be fine for treating blood pressure or migraines, but not for this condition.
Myth #3: Once you feel better, you can stop taking your beta-blocker.
This is risky. People sometimes feel pretty good after a few months on beta-blockers and think they can just quit. That often leads to symptoms coming right back—sometimes worse than before—and can land you back in the hospital. Beta-blockers work long-term and protect your heart over time, not just for a few weeks.
Some quick beta-blocker facts for heart failure:
- Beta-blockers can lower the risk of death in people with heart failure by up to 35%.
- Taking your meds every day—even on "good days"—is key to staying out of trouble.
- It can take weeks or even months to see real benefits, so patience is important.
Let’s make it real with a couple of stories I’ve heard from support groups:
Sarah, age 55, was worried that starting a beta-blocker would make her feel worse. She felt a bit tired for the first two weeks, but stuck with it. Three months in, her doctor said her heart function had actually improved, and she could walk up stairs again without gasping for air.
Mike, 47, thought he didn’t need his meds anymore and stopped them cold turkey. Within days, his heart failure symptoms came back hard—think swelling, tiredness, and ER visits. He learned the tough way that consistency beats quick fixes every time.
Taking beta-blockers seriously can make a huge difference for anyone dealing with left ventricular dysfunction. Don’t fall for the rumors—real results come from safe, steady use and a doctor who actually knows your story.






Jerry Erot
30 April 2025 - 14:34 PM
Look, I’ve read every guideline from the AHA and ESC, and let me tell you - beta-blockers aren’t just helpful, they’re foundational. Carvedilol’s the gold standard because it’s got alpha-blocking properties too, which means it reduces afterload AND heart rate. Most docs still start with metoprolol because it’s cheaper, but if you’ve got HFrEF and can tolerate it, carvedilol wins every time. And don’t even get me started on how many patients stop them after feeling ‘better’ - that’s how you end up back in the ICU.
Also, bisoprolol’s underrated. It’s more selective, fewer side effects, and the mortality data is just as strong. But yeah, titration is everything. You can’t just throw a 25mg tablet at someone who’s never taken one before. Slow and steady wins the race - and saves lives.
Fay naf
2 May 2025 - 01:50 AM
Let’s be real - beta-blockers are a band-aid on a ruptured aorta. You’re treating the symptom not the cause. Why aren’t we talking about myocardial remodeling? Why aren’t we pushing SGLT2 inhibitors as first-line? Beta-blockers are 1990s medicine. The PARADIGM-HF trial blew this whole paradigm wide open. ARNIs are better. SGLT2is are better. Beta-blockers? They’re just the last guy standing because nobody wants to change the script.
Also, ‘titrate slowly’ is just code for ‘we’re scared to mess with the algorithm.’ Your heart doesn’t need to be slowed down - it needs to be repaired. But hey, if you wanna keep giving people pills that make them feel like zombies, go ahead. I’ll be over here watching the real science move forward.
ANTHONY SANCHEZ RAMOS
2 May 2025 - 04:50 AM
OMG I just started carvedilol last month and I was SO scared 😅
First week I felt like a zombie, like my brain was wrapped in cotton 💤
But then - like magic 🪄 - I could walk to my mailbox without gasping?? My wife cried when I told her I didn’t need to sit down after taking out the trash 😭
DO NOT STOP. I almost did after 2 weeks because I felt ‘too tired’ but my cardiologist said ‘trust the process’ and I’m so glad I did.
Also side note: cold hands? YES. But I just wear gloves now. No big deal. This med is a GAME CHANGER. ❤️🫀
Anyone else feel like your pulse is a metronome now? 🎵
Matt Czyzewski
3 May 2025 - 06:17 AM
The paradox of beta-blockers is not merely pharmacological, but existential. We administer agents that suppress the body’s natural stress response - the very mechanism that evolved to sustain life under duress - in order to preserve a system that has already begun to fail.
Is this healing? Or is it merely postponing the inevitable through chemical restraint? The heart, after all, is not a pump to be tuned, but a living organ that remembers every strain, every surge, every silent cry for rest.
And yet - the data does not lie. Mortality drops. Ejection fraction rises. Quality of life improves. So perhaps the answer is not in rejecting the intervention, but in recognizing that medicine, at its best, is not about restoring nature, but about negotiating with it - gently, humbly, and with profound patience.
There is poetry in the slow titration. In the waiting. In the quiet dignity of a heart learning, once more, to beat without fear.
John Schmidt
4 May 2025 - 11:49 AM
So let me get this straight - you’re telling me we’re giving people drugs that lower heart rate to treat a condition caused by the heart being overworked… but we’re not asking why it got overworked in the first place?
Oh right - because Big Pharma doesn’t make money off ‘eat less sugar’ or ‘get more sleep.’
And don’t even get me started on how everyone acts like beta-blockers are the holy grail while ignoring that 40% of patients on them still get hospitalized. That’s not a cure, that’s a stopgap with side effects.
Also - ‘titrate slowly’? Yeah, because if you go too fast, people drop dead. But if you go too slow, they give up and quit. So we’re stuck in this bureaucratic limbo where the drug works… but the system doesn’t.
And Sarah from the article? She ‘felt better’? Maybe she just got used to being tired. That’s not improvement, that’s adaptation. And we’re calling it a win?
Lucinda Harrowell
5 May 2025 - 05:16 AM
It’s interesting how we treat beta-blockers like a universal fix, when really they’re just one tool in a very broken system. I’ve seen people on them for years - compliant, careful - and still struggle with fatigue, depression, isolation. The meds help the heart, but they don’t fix the loneliness that comes with chronic illness.
Maybe we need to measure success not just by ejection fraction, but by whether someone can sit on their porch and watch the sunset without feeling like a burden.
I’m not saying stop the meds. I’m saying: don’t forget the person behind the numbers.
Joe Rahme
6 May 2025 - 13:19 PM
Just wanted to say - this post is one of the clearest explanations I’ve seen. I’ve been on metoprolol for 3 years now, and honestly? I didn’t understand why I was taking it until I read this.
Thanks for breaking down the science without talking down to people. I’ve had doctors just say ‘take this, it helps’ - no context, no why.
And to the person who said ‘it’s just a band-aid’ - maybe. But sometimes a band-aid is all you need to keep walking until the real healing happens.
Keep sharing this stuff. It matters.