Every year, over 1.5 million people in the U.S. suffer preventable harm from medication errors. Many of these mistakes happen because someone didn’t stop to double-check the medication name, the strength, or the dosage form before giving or taking a drug. It’s not always a pharmacist’s mistake or a doctor’s typo. Sometimes, it’s just a quick glance at a label, a rushed moment, or a confusing abbreviation. But when it comes to medication safety, there’s no room for shortcuts.
Why Checking Medication Details Matters More Than You Think
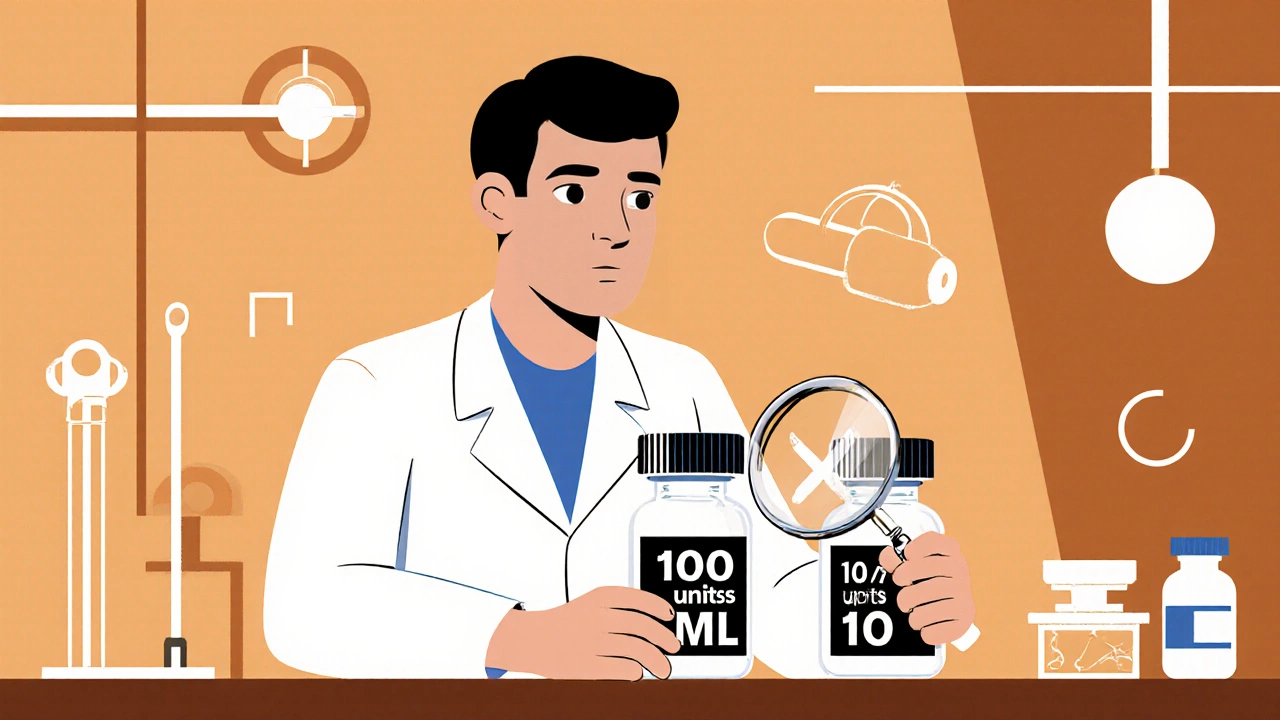
Think about this: insulin labeled as 100 units/mL looks almost identical to one labeled 10 units/mL. If you miss the "0" in the number, you could give a patient ten times the dose-and that’s deadly. Or consider "morphine sulfate" versus "magnesium sulfate." Both are abbreviated as "MS" on some charts. One calms pain. The other treats seizures. Mix them up, and someone could die. According to the Institute for Safe Medication Practices (ISMP), nearly 12% of all medication errors are caused by how the strength is written. Writing "10mg" without a space makes it easy to misread as "100 mg" or "1 mg." The FDA and ISMP both require a space between the number and unit: "10 mg." That tiny space saves lives. Dosage form matters too. A pill meant to be swallowed isn’t safe if crushed and given through a feeding tube. A liquid meant for the eye shouldn’t be taken by mouth. And a patch designed for skin absorption can be dangerous if swallowed. These aren’t rare mistakes. In a 2023 Reddit thread from pharmacy professionals, 18% of reported errors involved giving the wrong dosage form because it wasn’t clearly stated on the order.What You Need to Check Every Single Time
There are three non-negotiable things to verify before any medication is given, dispensed, or taken:- Drug name - Is it spelled right? Is it the full name or an abbreviation? Is it a look-alike or sound-alike drug?
- Strength - What’s the amount? What unit is it in? Is it written clearly?
- Dosage form - Is it a tablet, capsule, liquid, injection, patch, or inhaler?
How to Spot Dangerous Abbreviations and Typos
Some abbreviations are banned for good reason. Here’s what to watch for:- Never use "U" for units - it looks like a "0" or a "4." Always write "unit."
- Never use "μg" for micrograms - it’s easily confused with "mg." Always write "mcg."
- Avoid "QD" (daily) or "QID" (four times daily) - write out "daily" or "four times a day."
- Don’t use trailing zeros (like "5.0 mg"). That can be misread as "50 mg." Always use leading zeros: "0.5 mg."
- Watch for "MS" - it could mean morphine sulfate or magnesium sulfate. Always spell it out.
Use the "Tall Man" Lettering Trick
Some drug names are so similar, even experts mix them up. Here’s how to tell them apart:- PredniSONE vs. PredniSOLONE
- DoxoRUbicin vs. DoxoTObicin
- HYDROmorphone vs. HYDROxyzine

Verify Against the Original Source - Not Just the Screen
Electronic systems help, but they’re not perfect. A 2021 study found that 41% of pharmacists reported their EHR systems failed to flag dangerous strength combinations. And automation bias is real - when a system says "approved," people stop thinking. Always compare the medication you’re holding to the original prescription or order. Don’t rely on what’s on the screen. Don’t assume the barcode scanned correctly. Don’t trust the label if it looks faded or poorly printed. The best practice? Use the "three checks" rule:- Check when you receive the order - Is everything there? Is it clear?
- Check when you prepare the medication - Does the bottle, vial, or pill match the order?
- Check right before you give it - Confirm the patient’s name, the drug, the strength, and the form.
Read It Back - The Simplest Safety Net
One of the most effective tools in medication safety is the "read-back." It’s simple: when a nurse receives a verbal order, they repeat it back word-for-word. "You’re ordering hydromorphone 2 mg IV every 4 hours as needed?" The prescriber confirms: "Yes." This method is used in 89% of positive medication safety stories reported by nurses on the American Nurses Association forums. It works because it forces both people to slow down and confirm. It doesn’t take extra time - it prevents disaster. If you’re a patient, do this too. When a pharmacist hands you a new prescription, ask them to read the name, strength, and form out loud. Then read it back to them. If they hesitate, that’s a red flag.What to Do When Something Doesn’t Look Right
You don’t need to be a doctor or pharmacist to question a medication. If something feels off - the pill looks different, the liquid is cloudy, the dose seems too high - stop. Don’t take it. Don’t give it. Call the prescriber. Call the pharmacy. Ask for clarification. You have the right to know exactly what you’re taking. A nurse in Calgary told a story about catching a 100-fold overdose on heparin. The electronic order said "5,000 units/mL," but the vial said "50 units/mL." She didn’t assume the system was right. She checked the vial. She stopped the dose. That’s how safety works - one person paying attention.
High-Alert Medications Need Extra Steps
Some drugs are more dangerous than others. These are called high-alert medications. They include:- Insulin
- Heparin
- Opioids (morphine, fentanyl, oxycodone)
- IV potassium chloride
- Sodium chloride injections (concentrated)
- Chemotherapy agents
What Patients Can Do to Protect Themselves
You don’t have to wait for someone else to check your meds. You can do it yourself:- Always ask: "What is this medicine for? What’s the strength? How do I take it?"
- Compare the pill to the picture on the pharmacy website or the drug guide.
- Keep a written list of all your medications - name, strength, form, and why you take them.
- Use one pharmacy for all your prescriptions. That way, they can spot dangerous interactions.
- If you’re given a new medicine, ask: "Is this a high-alert drug?"
Final Thought: Safety Is a Habit, Not a Checklist
Medication safety isn’t about perfect systems. It’s about people paying attention. It’s about asking questions. It’s about saying "Wait, let me check that again." The technology is getting better. AI systems can now scan medication labels with 99.2% accuracy. But no algorithm replaces a human who cares enough to look. Whether you’re a patient, a caregiver, a nurse, or a pharmacist - your eyes, your voice, and your courage to speak up are the most powerful tools you have.What should I do if I notice a mistake on my medication label?
Stop. Don’t take the medication. Call your pharmacy or prescriber immediately. Show them the label and the prescription. Ask them to confirm the name, strength, and dosage form. If they dismiss your concern, ask to speak to a supervisor. You have the right to safe medication. Never ignore a red flag.
Can I trust the barcode on my medication?
Barcodes help reduce errors, but they’re not foolproof. Scanners can miss a label if it’s smudged, folded, or printed poorly. Always visually confirm the drug name, strength, and form on the vial or bottle matches what’s on your order. Never rely on the scanner alone - use it as a tool, not a guarantee.
Why is spacing important in medication strengths?
Writing "10mg" without a space can be misread as "100 mg" or "1 mg," especially in handwritten notes or low-quality prints. The FDA and ISMP require a space: "10 mg." This small change prevents about 12% of medication errors related to unit misinterpretation. Always use spacing - it’s a simple fix with a big impact.
What’s the difference between strength and dosage form?
Strength is how much of the drug is in each unit - like 5 mg, 10 mL, or 500 units. Dosage form is what the medication looks like - tablet, capsule, liquid, injection, patch, or inhaler. You can have the same strength in different forms. For example, 10 mg of hydrocodone can be a tablet or a liquid. Giving the wrong form can be dangerous - swallowing a patch or injecting a liquid meant for the eye can cause serious harm.
Are there any apps or tools that help verify medications?
Yes. Apps like Medscape, Epocrates, and Micromedex let you search drug names, check strengths, and verify dosage forms. Many pharmacies also offer digital pill identifiers. But these tools are for reference only. Always compare what’s in your hand to your prescription. No app replaces direct verification with the physical medication and original order.
What should I do if I’m given a medication I’ve never seen before?
Ask for the prescribing doctor’s name and the reason for the medication. Check the label for the full drug name, strength, and form. Look up the drug in a trusted source like the FDA’s website or your pharmacy’s online guide. If it still doesn’t make sense, don’t take it. Call your pharmacist or prescriber. It’s better to delay than to risk harm.
Why are some medications called "high-alert"?
High-alert medications have a higher risk of causing serious harm if used incorrectly. Examples include insulin, heparin, opioids, and IV potassium. Even small errors with these drugs can lead to death. Because of this, they require extra verification steps - like a second person checking the dose - before they’re given. Always treat these with extra caution.
Next Steps: Build Your Own Safety Routine
Start today. Make a habit of checking three things every time you handle a medication:- Is the name spelled correctly and fully written?
- Is the strength clear, with the right unit and spacing?
- Is the dosage form exactly what’s supposed to be given?





Peter Axelberg
29 November 2025 - 14:27 PM
Man, I’ve seen so many of these mistakes in the ER. Once saw a nurse hand a patient a vial of insulin labeled 100 units/mL - but the label was smudged and looked like 1000. The patient was diabetic and had no idea. She almost died. I yelled so loud the whole floor turned around. That’s when I started checking every single label, even if I’ve given the same drug a thousand times. Complacency doesn’t just kill - it kills slow, messy, and unnecessarily. Now I say it out loud: name, strength, form. If I’m not saying it, I’m not trusting it.
Monica Lindsey
29 November 2025 - 20:40 PM
If you’re not checking the three things, you’re not a professional. You’re a liability.
jamie sigler
29 November 2025 - 23:10 PM
I get it, safety’s important. But let’s be real - most of these errors happen because the system’s broken. Nurses are rushed, pharmacists are overworked, and patients are handed prescriptions like lottery tickets. No amount of ‘read-backs’ fixes a system designed to burn people out. We’re just putting band-aids on a hemorrhage.
Bernie Terrien
30 November 2025 - 23:27 PM
Ugh. ‘MS’ for morphine? That’s not a typo - that’s a death warrant with a corporate logo. And don’t even get me started on trailing zeros. Writing ‘5.0 mg’ is like handing a toddler a loaded gun and saying ‘be careful.’ This isn’t medicine - it’s a minefield with a white coat.
Jennifer Wang
1 December 2025 - 10:58 AM
It is imperative to emphasize that adherence to the Institute for Safe Medication Practices (ISMP) guidelines, particularly regarding the use of standardized nomenclature, spacing conventions, and avoidance of hazardous abbreviations, constitutes a foundational element of pharmacovigilance. The implementation of Tall Man lettering in electronic health records has demonstrated statistically significant reductions in error rates, as corroborated by multiple peer-reviewed studies published in the Journal of Patient Safety. Furthermore, the two-person verification protocol for high-alert medications is not merely a best practice - it is a non-negotiable standard of care.
stephen idiado
2 December 2025 - 05:33 AM
Western medicine overcomplicates everything. In Nigeria, we use generic names, no spacing, no tall man letters - just common sense. Most errors come from over-reliance on tech, not human error. Your system is the problem.
Subhash Singh
2 December 2025 - 08:00 AM
May I inquire whether the data regarding the 18% error rate in dosage form misidentification was derived from a randomized controlled trial or observational cohort? Additionally, are there any confounding variables such as language barriers or literacy levels among healthcare providers that were controlled for in the referenced Reddit thread analysis?
Andrew Keh
3 December 2025 - 20:27 PM
This is good stuff. I work in a small clinic and we don’t have fancy systems. But we do two things: we say the med out loud before we give it, and we keep a printed list of meds for every patient. Simple. Doesn’t cost a dime. And it works. I’ve caught three mistakes this year just by asking, ‘Wait, is this right?’
Peter Lubem Ause
4 December 2025 - 19:59 PM
Let me tell you something - safety isn’t just a checklist. It’s a mindset. I’ve seen nurses in Lagos who’ve never heard of Tall Man lettering, but they stop, look, and ask. They don’t trust the label, they don’t trust the screen, they trust their gut. And that’s the real secret. No app, no rulebook, no FDA memo can replace the courage to pause when something feels off. You don’t need to be an expert to save a life - you just need to care enough to ask. So if you’re reading this and you’ve ever thought, ‘It’s probably fine’ - stop. Don’t take it. Ask. Again. And again. Until you’re sure.
linda wood
4 December 2025 - 22:43 PM
Wow. So we’re supposed to be superheroes now? Check every label, read it back, double-check, write it down, use apps, avoid abbreviations, know which meds are ‘high-alert’ - and if you mess up? You’re a murderer. Meanwhile, my pharmacist is on her 8th shift in 48 hours and just yelled at me because I asked if this blue pill was the same as last time. So yeah. Thanks for the guilt trip, I guess. 😒
LINDA PUSPITASARI
6 December 2025 - 09:04 AM
YES YES YES 🙌 I’m a diabetic and I read every label out loud to my husband before I take anything. I even take pics of the bottle and send them to my pharmacist. I’ve caught 2 mistakes already - one was a wrong strength on my insulin. They said ‘it was just a typo’ but I said ‘nope, let me talk to your manager’ 😤 And guess what? They apologized and gave me a free month of supplies. You don’t have to be quiet to be safe. You just have to be loud enough to be heard 💪
gerardo beaudoin
6 December 2025 - 16:04 PM
I’m a pharmacy tech and I do the three checks every time. Even when I’m tired. Even when the script is messy. Even when the patient is in a hurry. I’ve had people roll their eyes. I’ve had doctors say ‘you’re overdoing it.’ But I’ve also stopped two wrong doses. One was a 10x overdose on morphine. The other was a patch meant for skin, given as a pill. I didn’t get a medal. But I got to go home knowing I didn’t hurt anyone. That’s enough.