PMDD Anxiety Link – Understanding the Connection
When working with PMDD anxiety link, the relationship between premenstrual dysphoric disorder and anxiety symptoms. Also known as PMDD‑anxiety connection, it shows how hormone swings can magnify nervous feelings.
First, let’s define Premenstrual Dysphoric Disorder (PMDD), a severe form of premenstrual syndrome that brings intense mood swings, irritability, and physical pain. Next, Anxiety, a feeling of worry or fear that can become chronic and disrupt daily life often spikes in the luteal phase of the cycle. Finally, two treatment classes matter: Selective Serotonin Reuptake Inhibitors (SSRIs), medications that boost serotonin to ease both mood and anxiety and Beta blockers, drugs that blunt the physical signs of anxiety like rapid heartbeat. These entities link together in a clear chain: PMDD creates hormonal turbulence, turbulence fuels anxiety, and the right meds can break the loop.
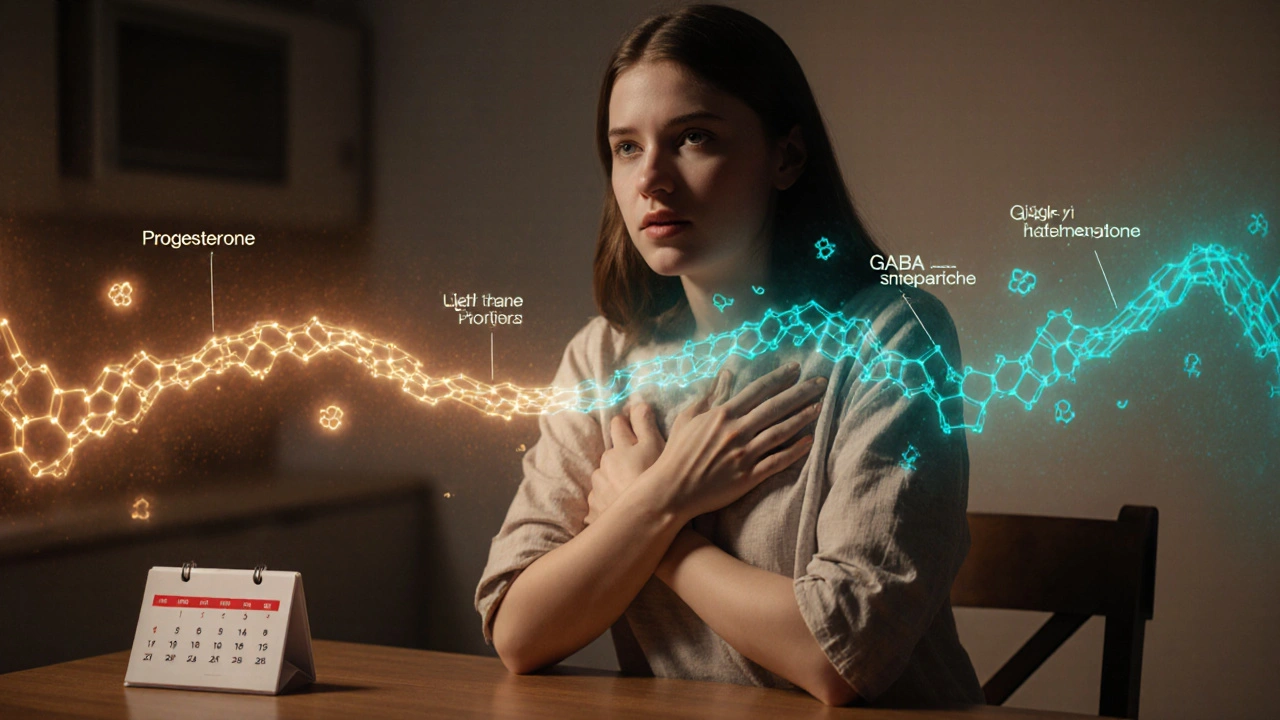
Why does the link exist? The brain’s serotonin system reacts sharply to fluctuations in estrogen and progesterone. When progesterone rises, it can lower serotonin, which in turn lifts anxiety levels. This is why many people notice “that time of the month” when nerves feel louder than usual. In scientific terms, PMDD anxiety link embodies a hormone‑neurotransmitter feedback loop. The loop triggers both emotional and somatic symptoms, so a treatment that only tackles one side often falls short.
Key Factors and Treatment Options
Understanding the loop helps you pick tools that hit the right spot. Lifestyle tweaks—regular exercise, balanced diet, and stress‑reduction practices—moderate hormone swings and keep serotonin steady. Nutrition matters: foods rich in magnesium, B‑vitamins, and omega‑3 fatty acids have shown modest anxiety‑lowering effects during the luteal phase. Sleep hygiene is another cornerstone; poor sleep amplifies both PMDD and anxiety, creating a vicious cycle.
When lifestyle changes aren’t enough, medication steps in. SSRIs like paroxetine (generic Paxil) and duloxetine (generic Cymbalta) are first‑line because they act quickly on both mood and anxiety. Clinical data shows they can reduce PMDD symptoms by up to 60% when taken continuously or only during the luteal phase. If serotonin‑focused therapy clashes with other meds or causes side effects, beta blockers such as propranolol provide a non‑psychiatric option. They don’t change mood directly but calm the body’s fight‑or‑flight response, making it easier to cope with the emotional surge.
Some women benefit from a combination approach: an SSRI for the emotional core plus a beta blocker for the physical jitters. This dual strategy mirrors the multi‑component nature of the PMDD anxiety link, the intertwined hormonal and nervous‑system pathways that drive symptoms. The idea is simple—treat the brain chemistry and the body’s stress response together.
Beyond prescription meds, over‑the‑counter supplements have carved out a niche. Ingredients like calcium‑D‑glucarate, vitamin B‑6, and St. John’s wort are frequently discussed in forums, though evidence varies. If you explore supplements, look for products that have been third‑party tested and start with low doses to gauge tolerance. Always check with a healthcare provider, especially if you’re already on SSRIs or beta blockers.
Another practical angle is timing. Some clinicians recommend starting SSRIs a few days before the expected onset of PMDD symptoms and stopping after menstruation ends. Others prefer a continuous daily dose. The best schedule depends on how severe the anxiety spike is and whether you experience side effects. Tracking your cycle with a simple app or journal helps you spot patterns and fine‑tune medication timing.
In summary, the PMDD anxiety link, the hormonal‑driven surge of anxiety that many women face each month isn’t a mystery—it’s a predictable physiological response. By addressing hormone fluctuations, serotonin balance, and the body’s stress signals, you can break the repeating pattern. Below you’ll find articles that dive deeper into diet tips, medication guides, supplement comparisons, and real‑world buying advice for the drugs mentioned. Let’s explore those resources and give you actionable steps to manage the cycle more confidently.
PMDD and Anxiety: How Hormonal Changes Trigger Anxiety Symptoms
Explore how hormonal shifts in Premenstrual Dysphoric Disorder trigger anxiety, learn to differentiate symptoms, and discover proven treatments and daily coping strategies.
Read More