Heart Failure: What It Is, How It Feels, and How to Manage It
If your doctor ever mentions "heart failure," it doesn’t mean the heart stops working like a dead engine. It simply means the heart isn’t pumping blood as efficiently as it should. That can make you feel tired, short‑of‑breath, or swollen in the legs. The good news is most people live well with proper care and lifestyle tweaks.
Common Signs You Might Miss
Early heart failure often hides behind everyday fatigue. You might notice you get winded climbing a single flight of stairs or that your shoes feel tighter because of ankle swelling. A persistent cough, especially at night, can be another clue—your lungs are holding extra fluid. Keep an eye on sudden weight gain; even a 2‑3 lb jump in a few days could signal fluid buildup.
Everyday Steps That Help Keep Your Heart Strong
Small habits make a big difference. Cutting back on salty foods reduces the amount of water your body holds, easing pressure on the heart. Aim for a brisk 30‑minute walk most days—your heart gets stronger and you burn excess calories that can strain it. If you smoke, quitting is the single best move; nicotine shrinks blood vessels and makes the heart work harder.
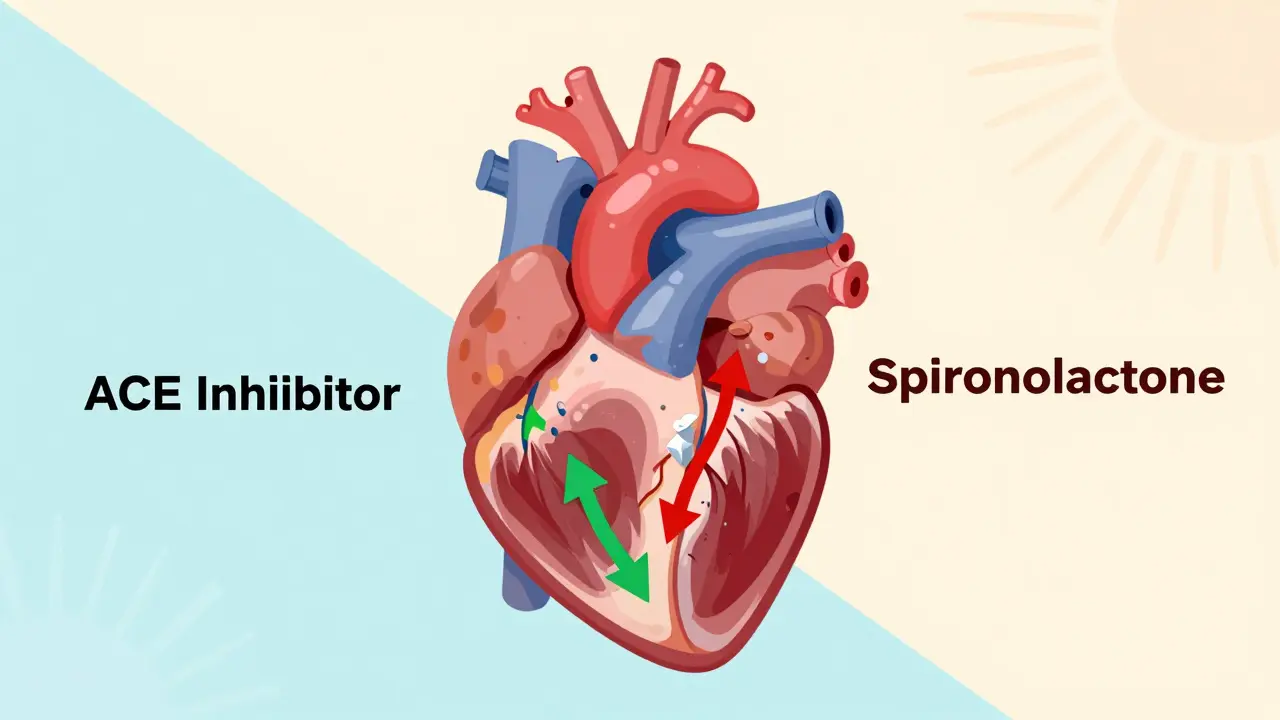
Medication is often part of the plan. Doctors commonly prescribe ACE inhibitors or beta‑blockers to lower blood pressure and reduce the heart’s workload. It’s crucial to take them exactly as directed, even if you feel fine. Skipping doses can undo progress and cause sudden worsening.
Regular check‑ups keep the picture clear. During a visit, your doctor will listen for extra sounds in the chest, measure blood pressure, and may order an echo to see how well the heart pumps. These tests help tweak treatment before symptoms flare up.
If you notice new or worsening symptoms—rapid weight gain, swelling that doesn’t go down after rest, or increasing shortness of breath—call your doctor right away. Early intervention can prevent a hospital stay and keep quality of life high.
Stress management also matters. Anxiety spikes heart rate and blood pressure, which isn’t kind to a struggling heart. Simple breathing exercises, meditation, or even chatting with friends can lower stress hormones and give your heart a breather.
Finally, think of your support network. Living with heart failure is easier when family members understand the diet changes, medication schedule, and warning signs. Sharing responsibilities—like grocery shopping for low‑sodium foods—helps you stay on track without feeling isolated.
Heart failure may sound scary, but with the right information, medicine, and daily habits, you can keep moving forward. Listen to your body, follow your doctor’s plan, and make those small lifestyle tweaks—they add up to a healthier heart over time.
ACE Inhibitors with Spironolactone: What You Need to Know About Hyperkalemia Risk
Combining ACE inhibitors with spironolactone reduces heart failure deaths by 30% but raises hyperkalemia risk. Learn who’s most at risk, how to monitor potassium safely, and when to adjust - not stop - the medication.
Read More
Beta-Blockers in Left Ventricular Dysfunction: What You Need to Know
Beta-blockers play a big role in managing left ventricular dysfunction, especially when it comes to heart failure. This article breaks down how these medications work, who benefits from them, and some tips for getting the most out of treatment. You'll also find common myths busted and hear about real experiences from patients. If you or someone you know is dealing with left ventricular issues, this guide helps cut through confusing info so you can make smarter decisions.
Read More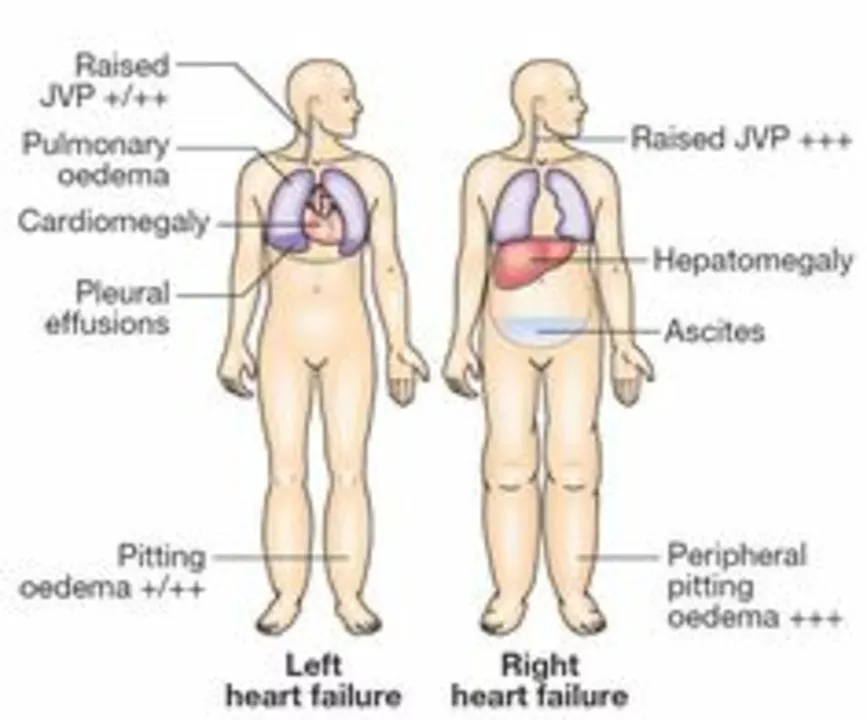
The Link Between Edema and Heart Failure: Symptoms and Treatment
As a blogger, I've recently come across some important information on the link between edema and heart failure. Edema is a condition where excess fluid accumulates in the body, often leading to swelling. I've learned that this can be a symptom of heart failure, as the heart struggles to pump blood effectively, causing fluid to build up. If you experience symptoms like swelling in your legs, ankles, or abdomen, it's crucial to seek medical attention. Treatment options for edema and heart failure may include medications, lifestyle changes, and in some cases, surgery.
Read More