Hatch-Waxman Act: How Generic Drugs Got Their Footing in the U.S. Market
When you pick up a generic pill at the pharmacy, you’re benefiting from a law passed in 1984 called the Hatch-Waxman Act, a U.S. law that created a pathway for generic drugs to be approved without repeating expensive clinical trials. Also known as the Drug Price Competition and Patent Term Restoration Act, it was designed to fix a broken system where brand-name drug makers held monopolies long after their patents expired. Before this law, companies spent years and millions developing the same drug just to prove it worked—when all they really needed to show was that it was the same as the original.
The Hatch-Waxman Act, a U.S. law that created a pathway for generic drugs to be approved without repeating expensive clinical trials. Also known as the Drug Price Competition and Patent Term Restoration Act, it was designed to fix a broken system where brand-name drug makers held monopolies long after their patents expired. Before this law, companies spent years and millions developing the same drug just to prove it worked—when all they really needed to show was that it was the same as the original.
The FDA, the U.S. agency responsible for approving drugs and ensuring their safety and effectiveness gained a clear process to review generics based on bioequivalence—not new trials. That meant a generic version of Lipitor or metformin could hit shelves in months, not decades. At the same time, the law gave brand-name companies up to five extra years of market exclusivity if they had to do new studies for pediatric use or other improvements. This wasn’t just a win for consumers—it kept innovation alive by giving companies a real reason to invest in new drugs.
It’s no accident that today, over 90% of prescriptions in the U.S. are filled with generics. The drug patent expiration, the point at which a brand-name drug’s legal protection ends, allowing competitors to produce cheaper versions became a predictable event, not a hidden cliff. Companies started planning for it. Pharmacies started stocking it. Patients started saving hundreds, sometimes thousands, per year. The brand-name drugs, originally developed and marketed by pharmaceutical companies with patent protection still exist—but now they compete on price and service, not just exclusivity.
And yet, the system isn’t perfect. Some companies game the patent system with minor changes—like switching a pill’s shape or coating—to delay generics. Others buy up competitors just to bury their generic versions. But the core of Hatch-Waxman still holds: if a drug’s patent expires, and a generic maker can prove it’s the same, it should be allowed on the market. That’s why you can now buy generic versions of everything from insulin to blood thinners for a fraction of the cost.
What you’ll find in the posts below are real-world stories and breakdowns tied to this law’s ripple effects. You’ll see how generic approval shapes what’s in your medicine cabinet, how patent tricks delay savings, and why some drugs still cost too much even after their patents expire. This isn’t just about law—it’s about your wallet, your health, and who gets to decide what’s affordable.

FDA Authorization of Generics: Legal Basis and Approval Process
Learn how the FDA approves generic drugs under the Hatch-Waxman Act, the science behind bioequivalence, and why generics cost up to 85% less than brand-name drugs - without sacrificing safety or effectiveness.
Read More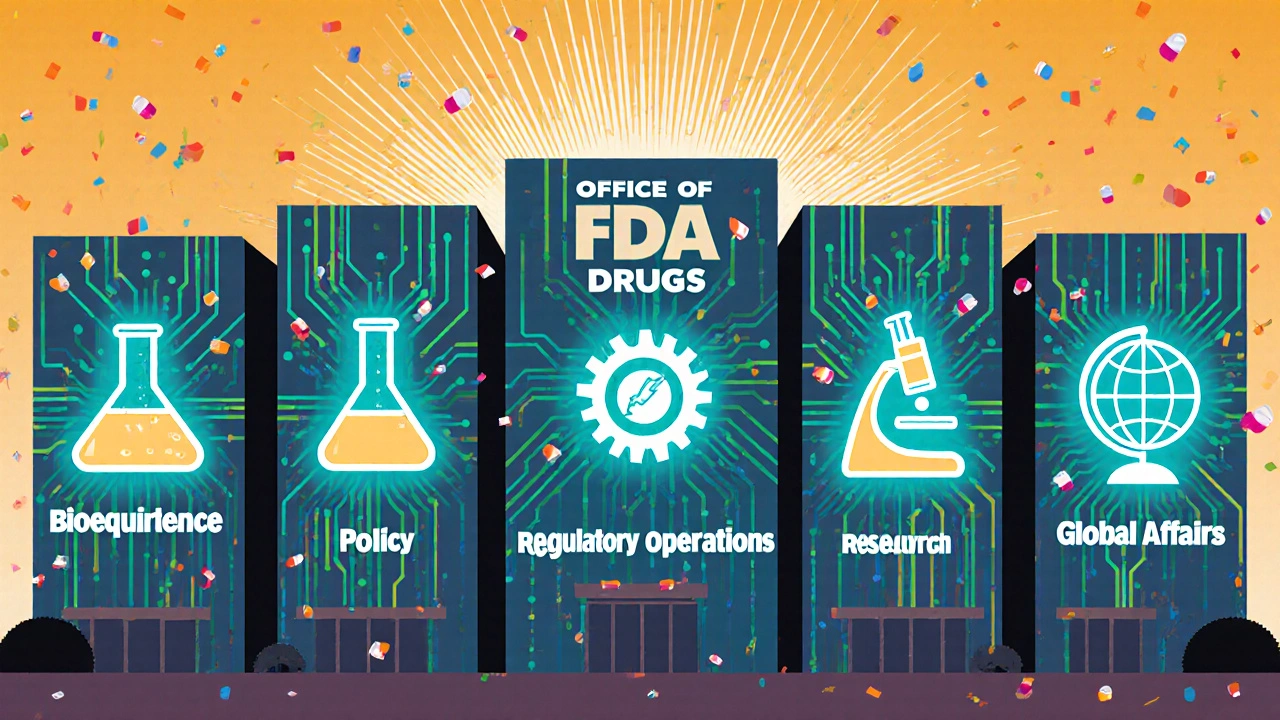
FDA Office of Generic Drugs: Role, Responsibilities, and Structure Explained
The FDA's Office of Generic Drugs ensures safe, affordable generic medications reach patients by reviewing applications, enforcing bioequivalence standards, and managing regulatory policy under GDUFA and the Hatch-Waxman Act.
Read More