Gender and Pharmacology: How Sex Differences Affect Drug Response
When we talk about gender and pharmacology, the study of how biological sex influences how drugs are absorbed, processed, and affect the body. Also known as sex-based pharmacology, it explains why the same dose of a drug can work differently—or even cause dangerous side effects—in men versus women. This isn’t just about hormones. It’s about liver enzymes, body fat, kidney function, and even how stomachs empty food. For decades, medical research mostly used male subjects. That meant we didn’t fully understand how drugs like blood thinners, antidepressants, or painkillers behaved in women—until it was too late.
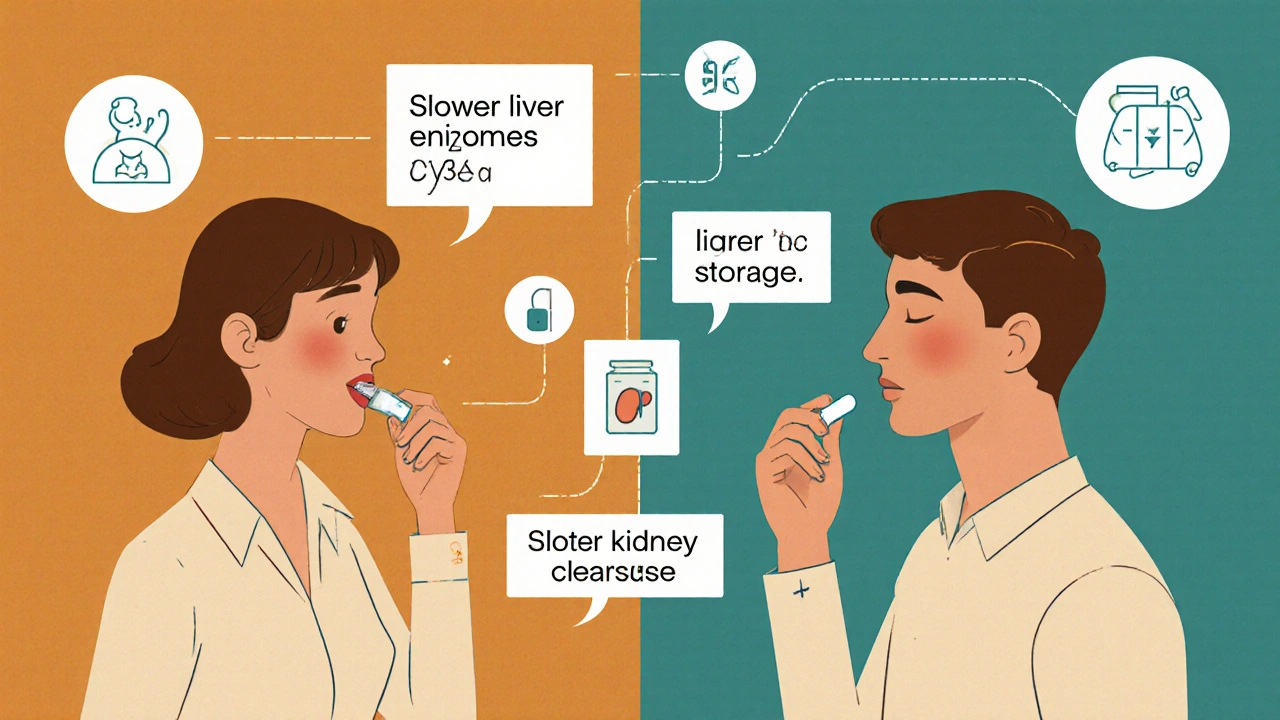
Pharmacokinetics, how the body moves a drug through absorption, distribution, metabolism, and excretion changes with sex. Women tend to have more body fat and less water, so fat-soluble drugs like benzodiazepines stick around longer. Their stomachs empty slower, which can delay how fast a pill hits the bloodstream. And their liver uses different enzymes to break down meds—like CYP3A4 and CYP2D6—which means some drugs build up to unsafe levels in women, while others get cleared too fast to work. Then there’s pharmacodynamics, how a drug interacts with its target in the body. Women often have more receptors for certain drugs, making them more sensitive. That’s why women are more likely to get dizziness from blood pressure meds or nausea from antibiotics.
These differences aren’t theoretical. Studies show women are 50-75% more likely to have adverse reactions to prescription drugs. Take zolpidem, the sleep pill Ambien: the FDA had to cut the recommended dose for women after reports of next-day drowsiness and car accidents. Or consider aspirin: it protects men from heart attacks better than women, while women get more bleeding risk. Even common painkillers like ibuprofen work differently—women often need higher doses for the same pain relief. And let’s not forget drugs like metformin or antidepressants, where women respond better but suffer more side effects like weight gain or GI upset.
None of this means one sex is "better" at handling meds. It means we need smarter, personalized dosing. Ignoring gender in pharmacology isn’t just outdated—it’s dangerous. The science is clear: if you’re taking any regular medication, your sex matters. It affects what works, what doesn’t, and what could hurt you. Below, you’ll find real-world examples from clinical studies and patient experiences that show exactly how these differences play out in daily life—and what you can do about them.
Why Women Experience More Medication Side Effects Than Men
Women experience nearly twice as many medication side effects as men due to biological differences and outdated clinical trial practices. Learn why this happens, which drugs are most affected, and what’s being done to fix it.
Read More