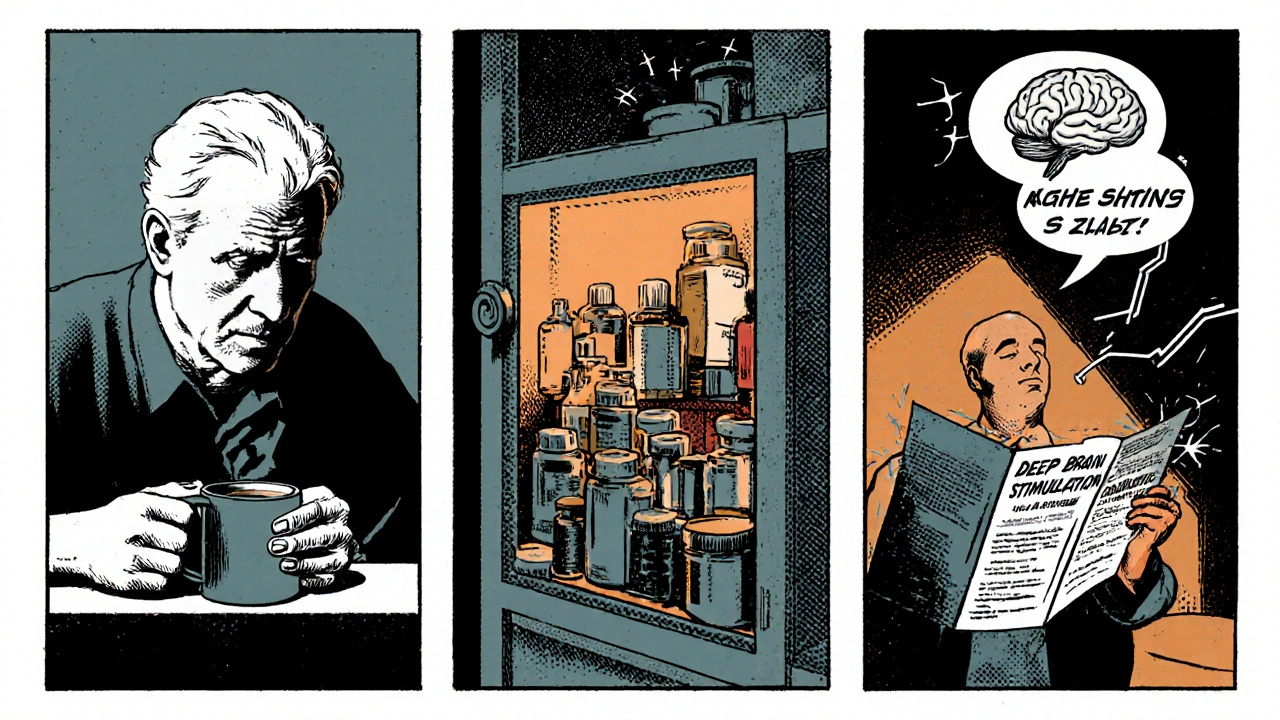
DBS Surgery: What You Need to Know
When talking about DBS surgery, a surgical technique that places electrodes in precise brain regions to modulate abnormal electrical activity. Also known as Deep Brain Stimulation, it provides a reversible, adjustable way to control symptoms of neurological conditions.
This approach relies heavily on neuromodulation, the use of electrical signals to influence nerve pathways. Neuromodulation enables clinicians to fine‑tune brain circuits without destroying tissue, which distinguishes DBS from older lesion‑based surgeries. The technology DBS surgery uses a programmable implantable pulse generator (IPG) that sits under the chest and delivers pulses through leads anchored in the brain.
How DBS Surgery Connects to Key Conditions
One of the most common targets for DBS is Parkinson's disease, a progressive movement disorder marked by tremor, rigidity, and slowed movement. Patients who no longer respond adequately to medication often see significant improvement in motor symptoms after the procedure. The same hardware can also address essential tremor, dystonia, and, in select cases, severe obsessive‑compulsive disorder. In each scenario, the surgery allows clinicians to adjust stimulation settings as the disease evolves, creating a personalized treatment plan.
Behind the scenes, the operation depends on stereotactic surgery, a precision technique that uses 3‑D imaging to guide instruments to targets within the brain. By overlaying MRI or CT scans with a frame or robot, surgeons can place the leads within millimeters of the intended nucleus. This accuracy ensures that the electric field reaches the right neurons, minimizing side effects and maximizing therapeutic benefit. The combination of stereotactic precision and neuromodulation flexibility makes DBS a unique therapeutic bridge between medication and irreversible brain surgery.
Recovery after DBS surgery follows a clear but patient‑specific path. Most people spend a few hours in a recovery room, then a short hospital stay to monitor the implant and perform initial programming of the IPG. Follow‑up visits are crucial because the device’s settings are tweaked over weeks or months to find the optimal balance between symptom control and side‑effects. Physical therapy, occupational therapy, and sometimes speech therapy support patients in regaining function and adapting to the new stimulation patterns.
Beyond the clinical side, cost and access are practical concerns. In many countries, insurance plans cover the procedure when strict criteria are met, but out‑of‑pocket expenses can still be high. Patients should verify that the surgical center is accredited, that the programming team has experience with their specific condition, and that the device manufacturer offers reliable warranty and support. Understanding these factors helps avoid unexpected hurdles and ensures a smoother journey from consultation to long‑term management.
Below you’ll find a curated collection of articles that dive deeper into each aspect of DBS surgery— from dietary tips that support recovery, to comparisons of different IPG models, and real‑world experiences from patients living with the technology. Whether you’re a prospective patient, a family member, or a healthcare professional, these resources will give you practical insights and actionable information to navigate the world of deep brain stimulation.
Deep Brain Stimulation for Parkinson’s Disease: What You Need to Know
Explore how Deep Brain Stimulation works, who qualifies, the surgical steps, benefits, risks, and how it compares to medication for Parkinson's disease.
Read More