Bioequivalence Requirements: What Makes Generic Drugs Safe and Effective
When you pick up a generic pill, you’re counting on it to do the same job as the brand-name version—without the high price. That’s where bioequivalence requirements, the scientific standards that prove a generic drug performs the same way in the body as its brand-name counterpart. Also known as therapeutic equivalence, these rules are the backbone of safe, affordable medicine in the U.S. The FDA doesn’t just accept claims—it demands proof. Every generic drug must show it releases the same amount of active ingredient at the same rate as the original. If it doesn’t, it doesn’t get approved.
This isn’t guesswork. It’s tested in real people using strict bioequivalence testing, a clinical process that measures how much of the drug enters the bloodstream and how quickly it’s absorbed. Researchers compare blood levels over time between the generic and brand-name versions. The numbers have to fall within a narrow range—usually 80% to 125%—to be considered equivalent. That’s not a coincidence. It’s science. And it’s why a $5 generic can treat high blood pressure just as well as a $50 brand name.
These rules exist because of the Hatch-Waxman Act, the 1984 law that created the pathway for generic drugs to enter the market without repeating expensive clinical trials. Also known as Drug Price Competition and Patent Term Restoration Act, it balanced innovation with access. Under this law, generic makers file an ANDA pathway, an Abbreviated New Drug Application that skips full safety trials because the active ingredient is already proven. All they need to prove is bioequivalence. The FDA’s Office of Generic Drugs, the team responsible for reviewing thousands of these applications each year and enforcing strict testing standards. makes sure no shortcut compromises safety.
Some people worry generics might not work as well. But the data doesn’t support that. Studies show generics perform identically in real-world use—from antibiotics to blood thinners. The difference isn’t in effectiveness. It’s in cost. And that’s the whole point. Bioequivalence requirements aren’t about cutting corners. They’re about cutting prices while keeping quality locked in.
What you’ll find in the posts below are real stories and facts about how these rules play out. From how the FDA checks for bioequivalence to why some drugs still cause confusion, you’ll see how the system works—when it’s working right, and when it’s not. No fluff. Just what matters for your health and your wallet.
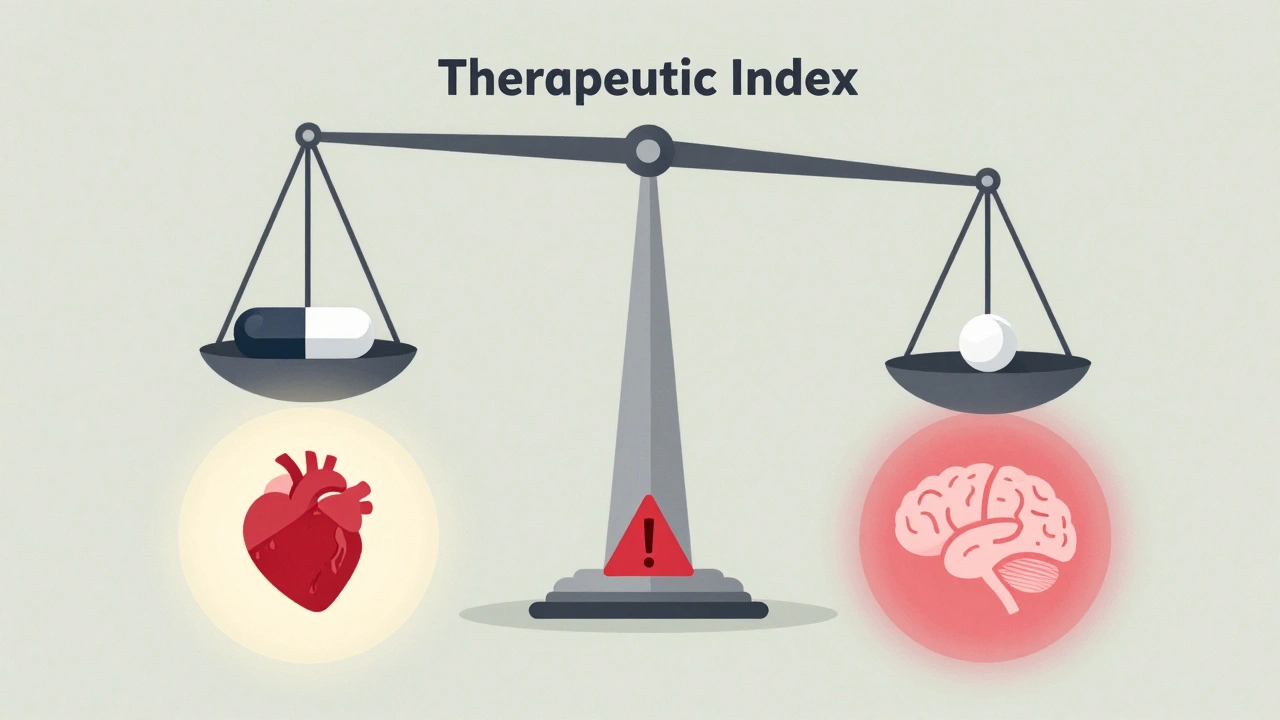
Narrow Therapeutic Index Drugs: Why Bioequivalence Standards Are Tighter for These Medications
Narrow therapeutic index drugs require stricter bioequivalence standards to ensure generic versions match the brand's safety and effectiveness. Learn why even small differences in dose can be dangerous and how regulators are protecting patients.
Read More