When your TSH is high but your thyroid hormone levels are normal, you’re not necessarily sick. But you’re not completely fine either. This is subclinical hypothyroidism - a gray area in medicine that leaves doctors and patients stuck between doing something and doing nothing. It’s not rare. About 1 in 5 adults in North America has it. And the big question isn’t whether it exists - it’s whether you need to take a pill for it.
What Exactly Is Subclinical Hypothyroidism?
Subclinical hypothyroidism means your pituitary gland is sending out more thyroid-stimulating hormone (TSH) because it thinks your thyroid isn’t working hard enough. But your thyroid is still producing enough free T4 to keep your body running. Your blood test shows a TSH above the lab’s normal range - usually over 4.0 to 4.5 mIU/L - but your free T4 stays in the normal zone. No weight gain. No fatigue. No dry skin. At least, not yet.
This isn’t a diagnosis you get from symptoms. It’s a lab finding. And that’s what makes it tricky. Some people feel awful with a TSH of 6.2. Others feel fine with a TSH of 9.0. The numbers alone don’t tell the full story.
The definition has stayed mostly the same since the 1970s, when sensitive TSH tests became available. But what we do with that information has changed - and still hasn’t settled. Different guidelines give different advice. And that confusion trickles down to your doctor’s office.
When Does a High TSH Actually Need Treatment?
There’s no universal rule. But most experts agree on this: if your TSH is above 10 mIU/L, treatment with levothyroxine is usually recommended. The evidence is clear here - people with TSH this high are much more likely to develop full-blown hypothyroidism within a few years. Studies show about 70% of people with TSH over 8 mIU/L will progress to overt hypothyroidism within four years.
But what about TSH between 5 and 10? That’s where the debate gets loud.
The American Thyroid Association says: don’t treat unless TSH is over 10. The American Association of Clinical Endocrinologists says: consider treatment if it’s over 7. The Endocrine Society says: maybe treat if you have symptoms or heart disease. The Royal Australian College of General Practitioners says: don’t treat at all in this range.
Why the mess? Because the data is messy. A 2017 JAMA study of 737 older adults found no improvement in energy, mood, or quality of life after a year of levothyroxine for TSH levels between 4 and 10. But a 2020 study of younger patients under 50 with positive thyroid antibodies showed a 32% drop in fatigue and brain fog after treatment.
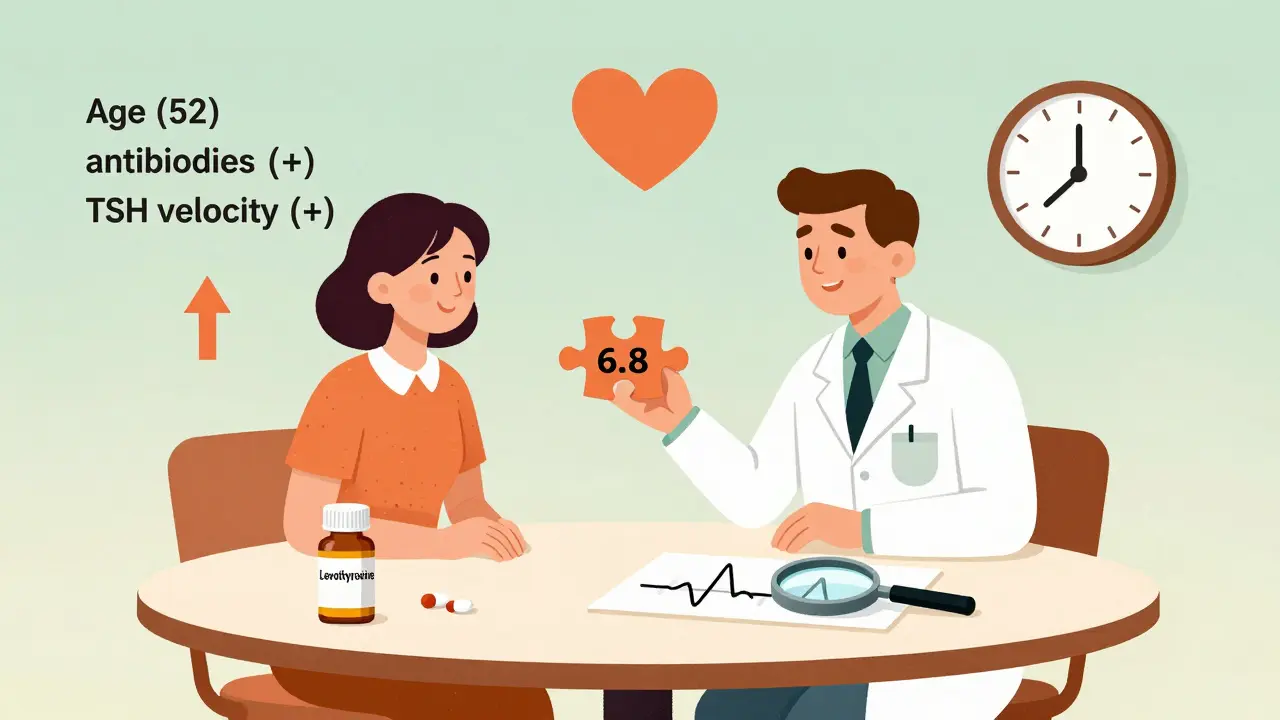
So age matters. Antibodies matter. Symptoms matter. And so does your heart.
The Role of Thyroid Antibodies
Not all elevated TSH is the same. If you test positive for thyroid peroxidase antibodies (TPOAb), your immune system is already attacking your thyroid. That’s Hashimoto’s in its early stage. These patients are far more likely to progress - 2.3 times more likely, according to a 2019 review.
For someone under 50 with TPO antibodies and a TSH of 7.5, waiting to treat until it hits 10 might mean missing a window to prevent long-term damage. The Cleveland Clinic now recommends considering treatment at TSH levels above 7-8 mIU/L in antibody-positive patients. It’s not about fixing symptoms yet. It’s about stopping the decline before it starts.
That’s why TPO testing isn’t optional. It’s the single most important factor in deciding whether to start medication for borderline TSH levels.
Who Should Avoid Treatment?
Not everyone benefits. In fact, for some people, treatment can be harmful.
Older adults - especially those over 65 - are at higher risk of side effects. A 2021 meta-analysis found that treating people over 65 with TSH under 10 increased their risk of death by 12.3%. Why? Because too much thyroid hormone can trigger atrial fibrillation, bone loss, and muscle weakness. In older patients, a slightly elevated TSH might be the body’s way of slowing down - not breaking down.
Also, don’t treat just because your TSH is high and your doctor is nervous. Many people with TSH between 5 and 7 never progress. Their levels stay stable for years. Treating them means lifelong medication, regular blood tests, and potential side effects - for no clear benefit.
That’s why guidelines now stress shared decision-making. Not just, “Here’s your pill.” But, “Here’s what we know. Here’s what we don’t. What matters to you?”

What About Symptoms?
“I’m tired all the time. My hair is falling out. I can’t lose weight.” These are the complaints that bring people in. But here’s the hard truth: studies show 30-40% of people with subclinical hypothyroidism report these symptoms - and so do 30-40% of people with perfectly normal thyroid function.
That doesn’t mean their symptoms aren’t real. It means they’re not necessarily caused by their thyroid. Fatigue can come from sleep apnea, low vitamin D, depression, or just aging. Brain fog? Could be stress, dehydration, or too much screen time.
So don’t treat based on symptoms alone. Use a tool like the 10-item Thyroid Symptom Rating Scale or the Thyroid-Related Quality of Life Patient-Reported Outcome (ThyPRO) questionnaire. These help separate thyroid-related symptoms from everything else. If your score is high and your TSH is over 7 with positive antibodies, treatment might help. If your score is low? Watch and wait.
The Treatment: Levothyroxine Basics
If you and your doctor decide to treat, levothyroxine is the only recommended medication. It’s a synthetic version of T4. Your body converts it to T3 as needed.
Start low: 25-50 mcg daily. Older adults or people with heart disease start at 25 mcg. Most people don’t need more than 75 mcg for subclinical hypothyroidism - unlike overt hypothyroidism, where doses of 100-125 mcg are common.
Take it on an empty stomach, at least 30-60 minutes before breakfast. Don’t take it with iron, calcium, or multivitamins. Those can block absorption by up to 39%. Wait four hours if you need to take them.
Check your TSH every 6-8 weeks after starting. Adjust the dose in 25 mcg increments until your TSH is between 1 and 3 mIU/L. Don’t aim for the bottom of the range - that’s overtreatment. And don’t go below 1.0. That can cause bone and heart problems.
What Happens If You Don’t Treat?
For many people, nothing. Their TSH stays stable. They feel fine. They live a normal life.
But for others - especially those with high antibodies, high TSH, or existing heart disease - untreated subclinical hypothyroidism can lead to higher LDL cholesterol, increased risk of heart attack, and progression to full hypothyroidism. A 2019 study found that people with TSH over 7 had a 1.5-fold higher risk of cardiovascular events over 10 years.
It’s not a guarantee. But it’s a risk. And for some, that risk is worth addressing.
The Future: TSH Velocity and Precision Medicine
The next big shift isn’t about one TSH number. It’s about how fast that number is climbing.
The European Thyroid Association now uses “TSH velocity” - how much your TSH rises per month. If your TSH jumps from 5.0 to 7.0 in six months, that’s a red flag. A rise of 1 mIU/L per month increases progression risk by 1.8 times. This is why some clinics now track TSH trends over time, not just single values.
Companies like Roche Diagnostics have already launched tools that calculate TSH velocity from past lab results. In the next five years, we’ll likely see personalized treatment based on your antibody status, age, TSH trend, and heart health - not just a number on a page.
The SHINE trial, a five-year study tracking 1,000 people with TSH between 4 and 10, will deliver results in late 2024. It’s the largest study of its kind. It may finally tell us whether treating this group reduces heart attacks or strokes.
What Should You Do Right Now?
If your TSH is high:
- Confirm it. One high TSH isn’t enough. Get a second test in 6-8 weeks.
- Test for TPO antibodies. This is non-negotiable.
- Check your cholesterol and blood pressure. High TSH often comes with higher LDL.
- Rate your symptoms. Use a simple scale: fatigue, cold intolerance, constipation, brain fog, dry skin, weight gain. Are they new? Are they getting worse?
- Ask your doctor: “Based on my age, antibodies, and TSH trend, do you think treatment will help me - or just add risk?”
If you’re over 65 and your TSH is under 10, the safest move is usually to do nothing - unless you have symptoms and positive antibodies. Then, talk carefully about the trade-offs.
If you’re under 50 with antibodies and TSH over 7, treatment is often the smarter long-term play. It’s not about feeling better tomorrow. It’s about protecting your thyroid for the next 10 years.
And if you’re unsure? Get a second opinion from an endocrinologist. This isn’t a decision to rush. It’s a decision to think through - with data, not fear.
Final Thought
Subclinical hypothyroidism isn’t a disease you can cure. It’s a signal - a quiet warning from your body. Sometimes, that signal means you need help. Sometimes, it just means you’re aging. The key is learning how to listen - and not overreact.
There’s no one-size-fits-all answer. But there is a better way: use your numbers, your antibodies, your age, your symptoms, and your risk - together - to make a choice that’s yours, not just your doctor’s.






sakshi nagpal
25 December 2025 - 08:12 AM
Interesting breakdown. I’ve been watching my TSH climb slowly over two years - started at 5.2, now at 7.1. No symptoms, but I got my TPO antibodies tested last month and they came back positive. After reading this, I’m leaning toward treatment. Not because I feel bad, but because I don’t want to wake up in five years with full hypothyroidism and regret not acting sooner.
Sumler Luu
25 December 2025 - 17:19 PM
My endo told me the same thing - if you’re under 50 and antibody-positive, treat before 8. But my GP said ‘wait and see.’ I ended up getting a second opinion. Best decision I made. Medicine should be personalized, not dictated by a guideline pamphlet.
roger dalomba
27 December 2025 - 05:56 AM
Wow. A whole essay on how to overmedicalize a number. Next up: ‘When to treat a slightly high BMI - it might mean you’re secretly dying.’
Brittany Fuhs
28 December 2025 - 00:45 AM
Of course the Americans are still arguing about this. In Germany, we treat TSH over 4.5 as a warning sign - not a suggestion. We don’t wait for people to have heart attacks before we act. Maybe if we stopped letting patients dictate treatment based on ‘how they feel,’ we’d have better outcomes.
Steven Destiny
29 December 2025 - 15:46 PM
STOP WAITING. If your TSH is over 7 and you have antibodies - start the med. I was skeptical too. Took levothyroxine for 3 months. My brain fog vanished. My energy came back. My hair stopped falling out. This isn’t magic. It’s biology. Don’t let fear of pills stop you from living.
Fabio Raphael
31 December 2025 - 13:41 PM
I’ve got a TSH of 6.8 and positive TPO. I don’t feel any different than I did last year. But I’m scared to start meds because I’ve heard stories of people going too high and getting heart issues. What’s the safest way to start low? And how often do you really need to test after that?
Amy Lesleighter (Wales)
1 January 2026 - 05:06 AM
my tsh was 8.2 last year. no symptoms. got tested for antibodies. positive. started 25mcg. felt nothing at first. then after 2 months? like someone turned the lights on in my head. no more 3pm crashes. no more forgetting where i put my keys. it wasn’t magic. it was just my body finally working right. if you’re under 50 and antibodies are up - just try it. worst case? you stop. best case? you get your life back.
Rajni Jain
2 January 2026 - 06:20 AM
hi i’m from india and my mom has this. she’s 62, tsh 8.9, no symptoms, no antibodies. her doctor said don’t touch it. she’s been fine for 3 years now. i think for older people, especially without symptoms, it’s better to leave it alone. the body knows what it’s doing. don’t mess with it unless you have to.
Natasha Sandra
4 January 2026 - 00:01 AM
OMG YES 🙌 I had this! TSH 7.5, antibodies up, felt like a zombie. Started levothyroxine and now I’m hiking on weekends and actually smiling 😊 Don’t let anyone tell you it’s ‘all in your head’ - your thyroid is real, and so is your fatigue 💪💖
Erwin Asilom
5 January 2026 - 04:53 AM
It’s not about whether you feel bad. It’s about whether you’re protecting your long-term health. If your TSH is rising, your thyroid is failing. Early intervention preserves function. Waiting until you’re symptomatic is like waiting for your car to catch fire before changing the oil.
Sandeep Jain
6 January 2026 - 20:16 PM
i had tsh 9.1 and thought it was just stress. then i found out i had hashimotos. started med. lost 12lbs in 3 months without trying. my skin stopped being like sandpaper. my brain stopped feeling like it was underwater. if you’re thinking about it - just do it. no regrets.
Sophia Daniels
7 January 2026 - 09:19 AM
Oh look, another ‘trust your doctor’ lecture from the medical-industrial complex. Meanwhile, Big Pharma is quietly funding every guideline that says ‘treat early.’ Do you really think they want you to wait? They want you on a pill for life. TSH is a number. Your body is the truth. If you feel fine? You are fine. Stop letting labs dictate your worth.
Nikki Brown
8 January 2026 - 20:28 PM
You’re all missing the point. This isn’t about medicine. It’s about control. Doctors are scared of being sued. Patients are scared of being wrong. So they both hide behind numbers. But the truth? Most people with subclinical hypothyroidism are perfectly healthy. The real problem? We’ve turned every biological variation into a disease that needs fixing.