Antibiotic Selection Assistant
Select Patient Factors
Treatment Recommendation
Select patient factors to see personalized recommendation.
When you or a loved one need a prescription for a bacterial infection, the choice of antibiotic can feel like a gamble. Roxithromycin is a semi‑synthetic macrolide marketed in many countries for respiratory and skin infections. It promises once‑daily dosing and fewer gut complaints than older macrolides, but is it really the best pick? This guide lines up Roxithromycin against the most common alternatives, breaks down the science, and gives you a checklist to decide what fits your case.
Key Takeaways
- Roxithromycin shares the same core mechanism as azithromycin and clarithromycin - it blocks bacterial protein synthesis.
- Its 12‑hour half‑life allows a convenient once‑daily schedule, but the drug is unavailable in the U.S., limiting access.
- For typical community‑acquired pneumonia, azithromycin and doxycycline are often cheaper and have broader evidence in Western guidelines.
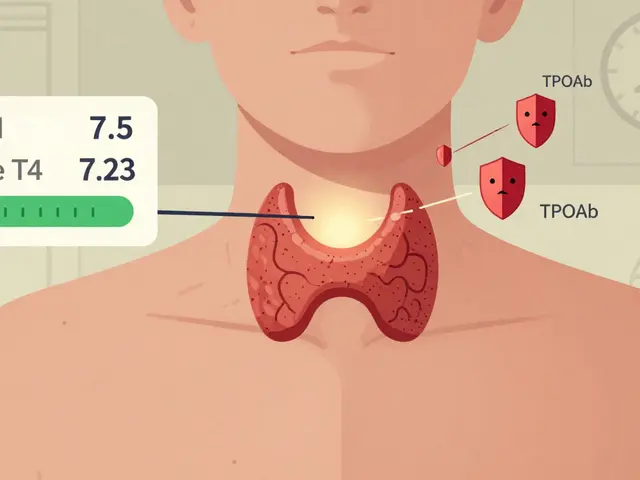
- Patients with liver disease or taking statins should avoid macrolides due to CYP3A4 interactions.
- A quick side‑effect checklist helps you spot when switching to a different class (e.g., fluoroquinolones) might be safer.
What Is Roxithromycin?
Roxithromycin belongs to the macrolide class, a group of antibiotics that bind to the 50S ribosomal subunit and halt bacterial protein production. First approved in Europe in the mid‑1990s, it was designed to improve tolerability over erythromycin. The drug is a 14‑membered lactone ring with a keto‑group that makes it more stable in acidic environments, resulting in better oral absorption.
Pharmacology at a Glance
- Class: Macrolide
- Mechanism: Inhibits the 50S ribosomal subunit
- Spectrum: Gram‑positive cocci, atypical pathogens (Mycoplasma, Chlamydia), some Gram‑negative bacilli
- Absorption: 90% oral bioavailability, food‑independent
- Half‑life: ~12hours (supports once‑daily dosing)
- Elimination: Primarily hepatic metabolism via CYP3A4
Typical Indications
In the countries where it’s sold, clinicians prescribe Roxithromycin for:
- Community‑acquired pneumonia (CAP)
- Acute sinusitis
- Bronchitis
- Skin and soft‑tissue infections caused by susceptible Staphylococcus aureus
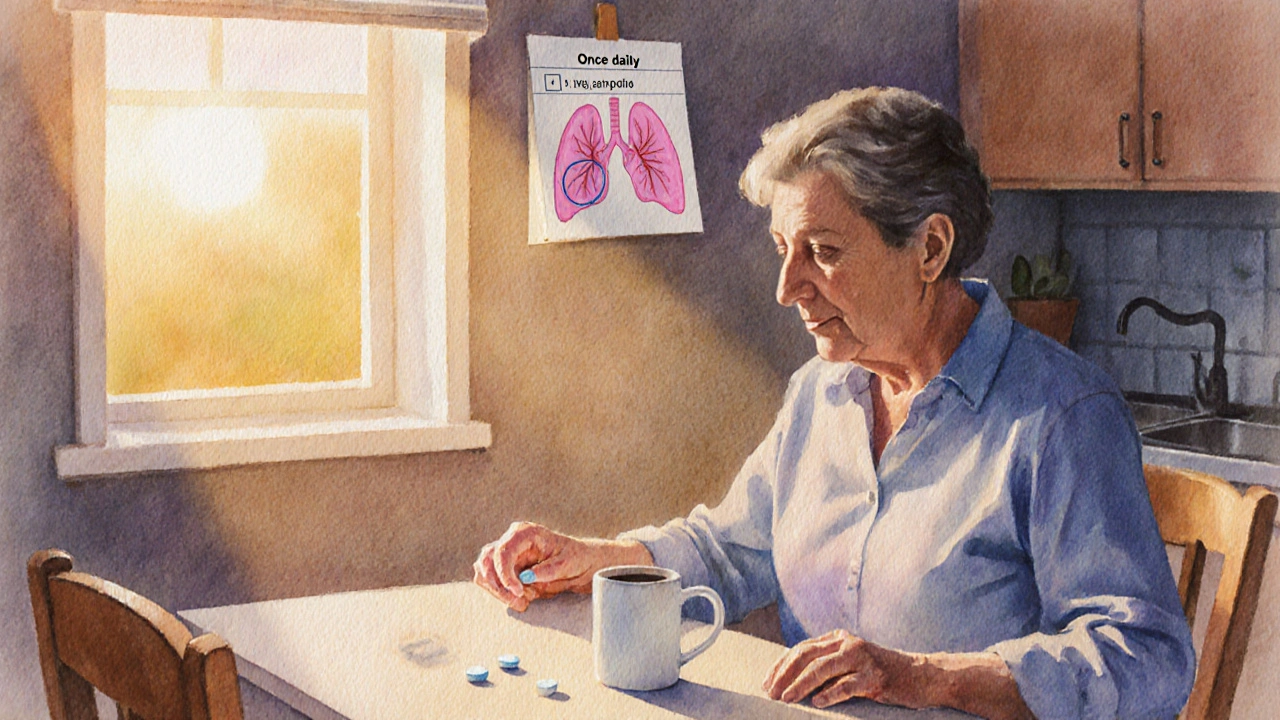
- Chronic obstructive pulmonary disease (COPD) exacerbations with bacterial component
Standard Dosing
The usual adult regimen is 150mg taken orally once daily for 5‑7days. Pediatric dosing follows weight‑based calculations (10‑15mg/kg once daily). No loading dose is required because steady‑state concentrations are reached within 2‑3days.
Safety Profile & Common Side Effects
- Gastro‑intestinal upset (nausea, mild diarrhea) - reported in <5% of users
- Transient elevation of liver enzymes - monitor in patients with pre‑existing liver disease
- QT‑interval prolongation - caution in patients on other QT‑prolonging drugs
- Rare hypersensitivity reactions (rash, angioedema)
Because Roxithromycin is metabolized by CYP3A4, it can increase serum levels of statins, warfarin, and certain antidiabetic agents.
Why Compare? The Decision‑Making Landscape
Choosing an antibiotic isn’t just about “which pill works.” You need to weigh local resistance patterns, drug availability, patient comorbidities, and insurance coverage. Below is a side‑by‑side look at the most frequently considered alternatives.
| Drug | Class | Typical Indications | Dosing (Adult) | Half‑Life | Key Side Effects | US Availability (2025) |
|---|---|---|---|---|---|---|
| Roxithromycin | Macrolide | Pneumonia, sinusitis, bronchitis, skin infections | 150mg once daily ×5‑7days | ≈12h | GI upset, mild liver enzyme rise, QT‑prolongation | No (not FDA‑approved) |
| Azithromycin | Macrolide | Pneumonia, chlamydia, atypical infections, traveler's diarrhea | 500mg day1, then 250mg daily ×4days | ≈68h | Diarrhea, hepatic injury (rare), QT‑prolongation | Yes |
| Clarithromycin | Macrolide | Helicobacter pylori eradication, CAP, skin infections | 500mg twice daily ×7‑14days | ≈3-4h | Metallic taste, GI upset, strong CYP3A4 inhibition | Yes |
| Doxycycline | Tetracycline | Lyme disease, acne, atypical pneumonia, malaria prophylaxis | 100mg twice daily ×7‑14days | ≈18h | Photosensitivity, esophagitis, dyspepsia | Yes |
| Levofloxacin | Fluoroquinolone | Severe CAP, urinary tract infections, skin infections | 750mg once daily ×5‑7days | ≈6-8h | Tendon rupture, CNS effects, QT‑prolongation | Yes |
| Amoxicillin | Penicillin | Otitis media, sinusitis, streptococcal pharyngitis | 500mg three times daily ×7‑10days | ≈1h (renally cleared) | Allergic rash, GI upset | Yes |
Deep‑Dive Comparisons
Roxithromycin vs. Azithromycin
Both drugs are macrolides, but azithromycin’s extremely long half‑life (≈68h) makes it attractive for short‑course regimens. Azithromycin also has a broader “real‑world” evidence base in the U.S., especially for atypical pneumonia and sexually transmitted infections. However, azithromycin’s high tissue concentration can increase the risk of QT prolongation, especially when combined with other heart‑acting meds.
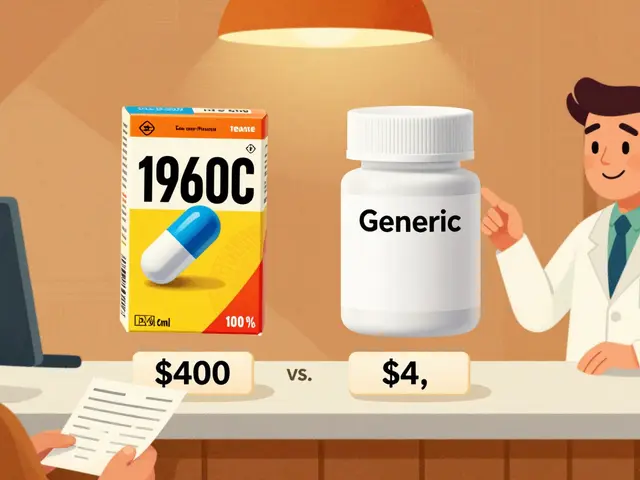
Roxithromycin’s once‑daily dosing is easier for elderly patients who struggle with multiple tablets, but the lack of FDA approval means you’ll need a specialty pharmacy or travel abroad to obtain it. Cost‑wise, generic azithromycin is usually under $10 for a 5‑day pack, while Roxithromycin can be $30‑$45 per pack in European markets.
Roxithromycin vs. Clarithromycin
Clarithromycin has a shorter half‑life and requires twice‑daily dosing, which can be a compliance hurdle. On the flip side, clarithromycin is a stronger CYP3A4 inhibitor, leading to more drug‑drug interactions. For patients on statins, clarithromycin can raise the risk of rhabdomyolysis - a concern that Roxithromycin shares but to a lesser degree.
Clinically, clarithromycin shines in Helicobacter pylori eradication protocols, where its acid‑stable formulation helps. If you’re treating a simple CAP, Roxithromycin’s efficacy is comparable, making it a reasonable alternative when clarithromycin isn’t tolerated.
Roxithromycin vs. Doxycycline
Doxycycline belongs to a different class (tetracycline) and works by binding the 30S ribosomal subunit. It’s widely used for atypical pneumonia, especially in younger adults and military personnel. Doxycycline offers the advantage of a broader antimicrobial spectrum against intracellular pathogens likeChlamydiaandMycoplasma.
Side‑effect profiles differ: doxycycline is notorious for photosensitivity, which can be problematic for outdoor workers. Roxithromycin’s GI upset is usually milder. Dosage frequency is another factor - doxycycline is twice daily, while Roxithromycin needs only once daily.
Roxithromycin vs. Levofloxacin
Levofloxacin, a fluoroquinolone, provides excellent coverage against both typical and atypical bacteria, plus high lung penetration. It’s often reserved for severe CAP or when macrolide resistance is suspected. The trade‑off is a higher risk of tendon rupture, peripheral neuropathy, and serious CNS effects.
If a patient has a history of tendon issues or is over 60, the safety advantages of a macrolide like Roxithromycin become persuasive, despite its narrower spectrum.
Roxithromycin vs. Amoxicillin
Amoxicillin is a first‑line beta‑lactam for many community infections, especially streptococcal pharyngitis and otitis media. It’s cheap, well‑tolerated, and has a short half‑life, requiring three daily doses. However, its activity against atypical organisms (Mycoplasma, Legionella) is limited.
When the suspected pathogen is a typical gram‑positive cocci, amoxicillin wins on cost and safety. When atypical coverage is needed, a macrolide - Roxithromycin or azithromycin - becomes the logical choice.
Quick Decision Checklist
- Is the infection typical or atypical? Atypical → consider macrolide or doxycycline.
- Can the patient take a once‑daily pill? Yes → Roxithromycin or azithromycin.
- Any known drug‑drug interactions? CYP3A4 substrates (statins, warfarin) need caution with macrolides.
- Allergy history? Macrolide allergy → switch to doxycycline or a beta‑lactam.
- Cost/availability? If US insurance covers azithromycin cheaper than imported Roxithromycin, choose azithromycin.
Potential Pitfalls & How to Avoid Them
- Resistance misconceptions: Assuming macrolides never fail leads to treatment delays. Check local resistance data before defaulting.
- Ignoring QT risk: Combine macrolides with anti‑arrhythmics only after ECG confirmation.
- Missing liver function: Elevated ALT/AST warrants dose reduction or switching to a non‑hepatic drug.
- Prescribing without allergy verification: Cross‑reactivity between macrolides is rare but documented; always ask.
Summary of When to Pick Roxithromycin
Roxithromycin makes sense when you need a once‑daily macrolide, have a patient who tolerates it better than azithromycin, and can access the drug through a specialty pharmacy. It’s especially handy for moderate CAP in adults without significant cardiac or liver disease.
Frequently Asked Questions
Can I take Roxithromycin if I’m pregnant?
Animal studies show no major teratogenic effect, but human data are limited. Most guidelines place macrolides, including Roxithromycin, in Pregnancy Category B, meaning they are generally considered safe after weighing benefits against risks. Always discuss with your obstetrician before starting.
How does Roxithromycin compare to Azithromycin for treating COVID‑19 secondary bacterial infection?
Both drugs have similar activity against common bacterial co‑pathogens likeStreptococcus pneumoniaeandHaemophilus influenzae. Azithromycin’s longer half‑life makes it easier for short‑course COVID‑19 regimens, but the evidence for macrolide benefit in viral infections is weak. Choose based on local resistance and drug availability.
Is a food‑fasting interval needed when taking Roxithromycin?
No. Roxithromycin’s absorption isn’t significantly affected by food, so patients can take it with or without meals, which helps adherence.
What should I monitor while on Roxithromycin?
Baseline liver enzymes, ECG if you have a history of arrhythmia, and watch for any rash or GI upset. If you notice palpitations or severe diarrhea, contact your clinician.
Can I switch from Roxithromycin to Azithromycin mid‑course?
Switching is possible, but you need to consider the remaining dose and avoid double‑counting the macrolide effect. Typically, clinicians finish the current Roxithromycin course then start a new 5‑day azithromycin regimen if needed.





Ben Small
14 October 2025 - 17:12 PM
Alright folks, if you’re weighing Roxithromycin against the usual suspects, remember it’s a once‑daily macrolide that sounds great on paper. The real kicker is that it’s not even sold in the U.S., so getting it is a hassle. For CAP you’re better off with azithro or doxy because the guidelines back them up and they’re cheap. Bottom line: don’t chase the novelty if you can grab a proven drug today.
Dylan Hilton
26 October 2025 - 02:39 AM
That’s a solid summary! I’d add that the hepatic metabolism via CYP3A4 can be a real issue for patients on statins, so the interaction risk isn’t just theoretical. Also, the 12‑hour half‑life does give you convenient dosing, but the lack of U.S. availability limits its practicality. Overall, sticking with azithromycin or doxycycline keeps things simple and evidence‑based.
Christian Andrabado
6 November 2025 - 11:06 AM
Roxithro sounds like a marketing gimmick. No US approval, limited data, and still the same CYP3A4 worries. Why risk it when cheaper alternatives exist. It’s just another brand trying to sell a repackaged macrolide.
Chidi Anslem
17 November 2025 - 20:32 PM
While the commercial angle is clear, we should also consider patient‑centered factors. In regions where Roxithromycin is accessible, its once‑daily schedule can improve adherence, especially for elderly patients with polypharmacy. However, the metabolic pathway still raises concerns for those with hepatic impairment or on statins, aligning with the broader caution applied to macrolides. Balancing convenience against safety is the core of antibiotic stewardship.
Holly Hayes
29 November 2025 - 05:59 AM
People should stop glorifying cheap shortcuts.
Jennifer Banash
10 December 2025 - 15:26 PM
Permit me to elucidate the gravity of this discourse. The decision to employ Roxithromycin, an agent not sanctioned by the United States Food and Drug Administration, transcends mere pharmacokinetic curiosity. It implicates ethical stewardship, patient safety, and the unwavering adherence to evidence‑based protocols that underpin modern medicine. In the face of robust data favoring azithromycin and doxycycline, resorting to an obscure macrolide would be, to phrase it with appropriate gravitas, a dereliction of professional duty.
Stephen Gachie
22 December 2025 - 00:52 AM
When we contemplate the choice of an antibiotic we are, in essence, confronting the paradox of human control over microscopic life. The macrolide class, to which Roxithromycin belongs, promises a tidy mechanism- inhibition of the 50S ribosomal subunit. Yet the elegance of this mechanism belies the tangled web of hepatic metabolism that ensnares it. CYP3A4, the enzyme at the heart of this process, is a shared conduit for countless pharmaceuticals, statins most notably. This shared conduit creates a battlefield within the liver, where drug‑drug interactions are not mere footnotes but potential catastrophes. The clinical literature from Western guidelines leans heavily toward azithromycin and doxycycline for community‑acquired pneumonia, citing superior efficacy and cost. Moreover, the absence of Roxithromycin from the United States pharmacopeia is not an oversight but a deliberate regulatory judgment. Accessibility, therefore, becomes a secondary concern to evidence. The principle of antimicrobial stewardship demands that we prioritize agents with a well‑established safety profile. One could argue that the once‑daily dosing of Roxithromycin offers adherence benefits, but adherence is a function of many variables beyond dosing frequency. Patient education, comorbidities, and health system factors play equal roles. In cases of liver impairment, the drug’s metabolic pathway becomes a liability rather than an asset. The risk of hepatotoxicity and interaction supersedes the modest convenience offered. Ultimately, the decision matrix tilts heavily against Roxithromycin when we weigh evidence, safety, and practicality. The philosopher’s quest for truth aligns with the clinician’s duty to choose the most proven therapy.
Sara Spitzer
2 January 2026 - 10:19 AM
Honestly, the whole Roxithromycin hype is overblown. The data simply doesn’t support it as a first‑line agent, and the cost‑benefit analysis falls flat compared to azithromycin or doxycycline. It’s a textbook case of marketing over medicine.
Jennifer Pavlik
13 January 2026 - 19:46 PM
Hey everyone, if you’re not sure which antibiotic to pick, think about a few easy points: is the drug easy to get, does it work well for the infection, and does it have safe side effects? For most people azithromycin or doxycycline hit those marks, so they’re a solid start.
Jacob Miller
25 January 2026 - 05:12 AM
It’s surprising how many still cherry‑pick Roxithromycin without checking the guidelines. If you want to stay safe, follow the evidence instead of chasing the latest brand.
Anshul Gandhi
5 February 2026 - 14:39 PM
Don’t be fooled-the pharma giants keep Roxithromycin hidden in the U.S. to push more profitable drugs. They control the market, and the “lack of approval” is just a smokescreen for profit motives. Wake up and look beyond the official narrative.
Emily Wang
17 February 2026 - 00:06 AM
Let’s cut to the chase: if you have a liver issue or are on statins, skip Roxithromycin. Pick a proven alternative and move on.