Chronic muscle pain that won’t go away, even after rest, stretching, or painkillers? You might not have a pinched nerve or a herniated disc-you could be dealing with myofascial pain syndrome. This condition isn’t rare. In fact, up to 85% of people who visit pain clinics have it. But most doctors don’t talk about it. That’s because the pain doesn’t show up on X-rays or MRIs. It hides in your muscles, in tight knots called trigger points.
What Are Trigger Points, Really?
Trigger points aren’t just sore spots. They’re hyperirritable knots inside taut bands of muscle. Think of them like a cramp that never lets go. When you press on one, you don’t just feel pain where you’re touching-you feel it shoot into your shoulder, head, or even down your arm. That’s referred pain. It’s why people think they have a pinched nerve when it’s actually a trigger point in their upper trapezius muscle.
These knots form because of a biochemical mess inside the muscle. Acetylcholine, serotonin, and other chemicals pile up. The muscle fibers contract and stay locked. Blood flow gets cut off. Oxygen drops. Waste builds up. It’s like a tiny storm inside your muscle that keeps spinning.
There are two kinds: active and latent. Active trigger points hurt all the time. They’re the ones keeping you up at night or making it hard to turn your head. Latent ones? They only hurt when you press on them. But they’re still trouble. They weaken your muscles, limit your movement, and can turn active if you get stressed, sleep poorly, or sit too long.
Where Do Trigger Points Hide?
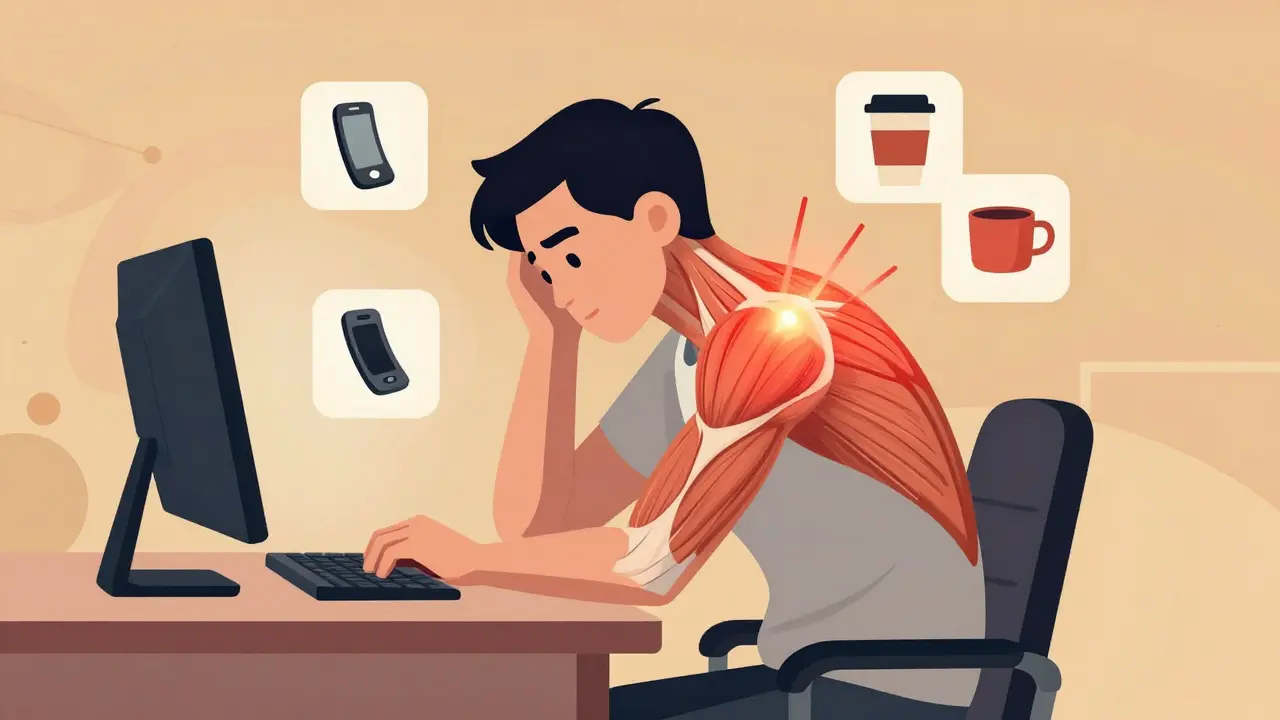
They can pop up anywhere there’s muscle. But some spots are way more common. The top three? Your upper traps (that’s the muscle from your neck to your shoulder), your levator scapulae (the muscle that runs from your neck to your shoulder blade), and your temporalis (a jaw muscle you don’t even think about).
Why these? Because they’re overworked. If you sit at a desk all day with your head leaning forward, your upper traps are holding your head up like a 10-pound weight. That’s 8-10 hours a day. No wonder they tighten up. Same with your jaw-if you clench your teeth at night or chew gum nonstop, your temporalis gets locked in a spasm. That’s why many people with chronic headaches don’t realize their pain is coming from their jaw.
Other common spots: the rhomboids between your shoulder blades, the glutes, the calves, and the muscles around your pelvis. If you’ve had a car accident, even a minor one, trigger points can form in your neck or lower back within days. Whiplash? About 60% of people develop MPS after it.
How Is It Different From Fibromyalgia?
This is a big one. People mix up myofascial pain syndrome and fibromyalgia all the time. But they’re not the same.
Fibromyalgia causes widespread pain all over the body. It’s symmetrical-both sides hurt the same. The pain is more about sensitivity than knots. You’ll have tender spots, but they don’t refer pain. They just hurt when pressed.
Myofascial pain? It’s localized. One side of your neck hurts. One shoulder. One hip. The pain follows a pattern. Press a trigger point in your upper trap, and you’ll feel pain in your temple. Press one in your glute, and your leg tingles. That’s a hallmark of MPS.
And here’s the kicker: fibromyalgia doesn’t have the local twitch response. If you poke a trigger point with a needle or your finger, and the muscle jumps, that’s a sign it’s MPS-not fibromyalgia.
What Causes Trigger Points to Form?
It’s not just one thing. It’s a combo.
- Posture: Slouching at your desk, cradling your phone between ear and shoulder, sleeping on your stomach-all these force muscles into unnatural positions. Over time, they lock up.
- Repetitive strain: Typing all day, lifting boxes, playing tennis, even knitting can overload specific muscles.
- Injury: A fall, a car crash, even a bad cough can tear muscle fibers. When they heal, they form scar tissue and trigger points.
- Stress: When you’re anxious, your body tenses. Your shoulders hike up. Your jaw clenches. That constant tension turns into knots.
- Nutrition: Low vitamin D (under 20 ng/mL) raises your risk by 60%. Low magnesium? Same thing. Thyroid problems? About 1 in 5 chronic MPS patients have hypothyroidism.
- Leg length differences: Even a 1-centimeter difference can tilt your pelvis and overload one side of your lower back and glutes.
It’s not weakness. It’s mechanics. Your body adapts to how you move-and if you move poorly for long enough, your muscles pay the price.

How Do You Find Trigger Points?
It’s not magic. It’s touch.
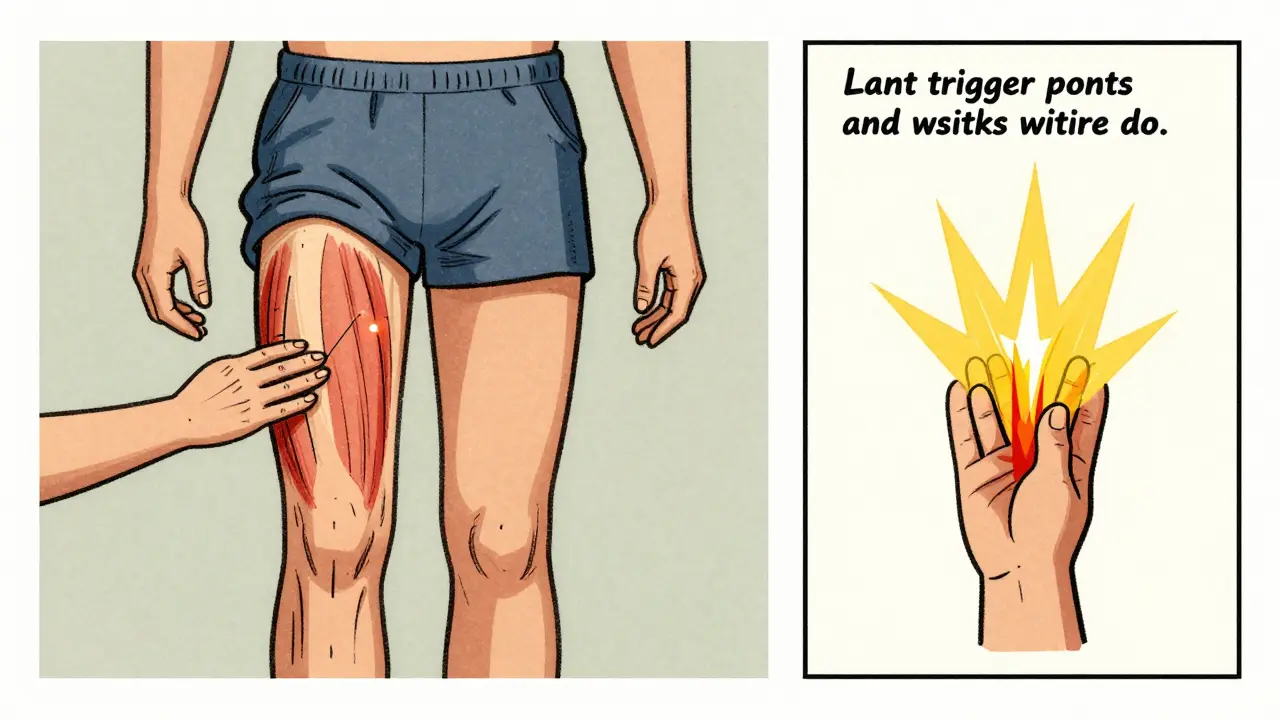
Start by feeling along the muscle. Run your fingers slowly from one end to the other. Look for a tight band-like a guitar string under your skin. Now press gently along that band. When you hit a spot that makes you wince or sends a sharp pain elsewhere? That’s your trigger point.
Here’s how to confirm: if you press it and the muscle twitches, you’ve found it. That’s called a local twitch response. It’s a sign the muscle is reacting. About 80% of active trigger points show this.
Don’t rely on apps or diagrams. Those are guides, not maps. Everyone’s body is different. What works for one person might not work for you. The best way to learn? Try it on yourself. Use your thumb or a tennis ball against a wall. Press slowly. Breathe. Notice where the pain goes.
Trigger Point Release Techniques That Actually Work
There are a lot of treatments out there. Some work. Most don’t. Here’s what the research says works best.
Ischemic Compression
This is the simplest and most effective. You press directly on the trigger point with your thumb, knuckle, or a tennis ball. Hold for 30 to 90 seconds. Don’t just tap. Hold. Keep breathing. The pain will peak, then slowly fade. When it drops by 50%, you can ease off.
Studies show 60-75% of people get relief after one session. Do it daily for a week. Most people see major improvement by day 4.
Dry Needling
This is when a physical therapist or doctor sticks a thin needle into the trigger point. It’s not an injection-no medicine goes in. Just the needle. When it hits the knot, the muscle jumps. That twitch is good. It means the muscle is resetting.
It works fast. Many feel relief right after. Effects last 4 to 12 weeks. About 70% of patients report at least 50% pain reduction. But it’s not for everyone. If you hate needles or have a bleeding disorder, skip it.
Spray and Stretch
This one’s old-school but still useful. A cold spray (like ethyl chloride) is sprayed over the area where the pain radiates. Then the muscle is stretched. The cold tricks the nerves. The stretch breaks the knot. It’s especially helpful for neck and jaw pain.
Self-Massage Tools
You don’t need a therapist to manage this. A foam roller works for big muscles like quads and back. A lacrosse ball is better for small spots like glutes or shoulders. A tennis ball against a wall? Perfect for upper traps.
Try this: lean against the wall with the ball between your shoulder blade and spine. Breathe. Roll slowly. Find the spot that hurts the most. Hold for 45 seconds. Do this 2-3 times a day.
Heat Before Stretching
Never stretch a cold, tight muscle. Warm it up first. Use a heating pad at 40-45°C for 15 minutes. Or take a warm shower. Heat loosens the tissue. Then stretch. Hold each stretch 30 seconds. Repeat 3 times. Do this twice daily.
Why Do People Get Worse After Treatment?
Because they stop too soon.
Trigger points don’t vanish after one session. They come back if the root cause isn’t fixed. If you sit at your desk the same way, keep clenching your jaw, or ignore your vitamin D levels, the knots will return.
A study of over 1,200 patients found that those who did daily self-care-massage, stretching, posture fixes-had 65% less pain after 12 weeks. Those who didn’t? Only 35% improvement. And 40-60% of people who quit maintenance therapy had pain return within 6 months.
Also, bad technique makes it worse. If someone presses too hard, too fast, or in the wrong spot, they can irritate the muscle more. That’s why some people say, “I went to a therapist and it made my pain worse.” They weren’t trained in trigger point therapy. Look for someone with certification in myofascial release or dry needling.
What to Avoid
- Overusing painkillers: NSAIDs like ibuprofen might mask the pain but don’t fix the knot. They can also hurt your gut or kidneys with long-term use.
- Ignoring posture: No amount of massage will help if you keep hunching over your phone.
- Waiting for it to go away: Myofascial pain doesn’t heal on its own. It gets worse.
- Getting unnecessary imaging: MRIs and X-rays won’t show trigger points. You’re wasting time and money.
How to Keep It From Coming Back
Think of this like brushing your teeth. You don’t do it once and expect your teeth to stay healthy forever. Same here.
- Do 10 minutes of self-massage daily. Use a ball or your fingers.
- Stretch your tight muscles twice a day. Focus on neck, shoulders, jaw, and hips.
- Check your posture every hour. Sit back. Shoulders down. Screen at eye level.
- Get your vitamin D checked. If it’s under 30 ng/mL, take a supplement.
- Manage stress. Try breathing exercises. Tension is the #1 trigger for trigger points.
Most people don’t realize how much their daily habits feed this pain. Fix those, and you won’t need endless treatments.
When to See a Professional
You can manage mild cases on your own. But see a specialist if:
- The pain lasts more than 3 weeks despite self-care
- It’s getting worse, not better
- You have numbness, tingling, or weakness along with the pain
- You’ve tried everything and still can’t sleep or move normally
Look for a physical therapist, chiropractor, or doctor certified in trigger point therapy. Ask if they’ve read Travell and Simons’ manuals. That’s the gold standard.
And don’t settle for someone who just gives you a massage. Myofascial release isn’t relaxation. It’s targeted, specific, and sometimes uncomfortable. If it feels like a spa day, they’re not treating the trigger points.






Michelle M
15 December 2025 - 15:43 PM
Trigger points are like emotional baggage stored in your muscles-every stress, every bad posture, every silent scream your body never got to release. I used to think my chronic headaches were from screen glare, but after finding a knot in my temporalis, everything changed. It’s not just physical-it’s psychological too. The body remembers what the mind tries to forget.
And yes, vitamin D matters. I was at 17 ng/mL last year. Took supplements. My jaw stopped clenching in my sleep. No more morning migraines. Simple fix, ignored by 90% of doctors.
Stop chasing MRIs. Start chasing your own breath. Press. Hold. Breathe. Repeat. It’s not magic. It’s mechanics.
And if you’re sitting right now? Adjust. Shoulders down. Chin tucked. You’re welcome.
Nupur Vimal
16 December 2025 - 13:11 PM
People think its just stress but its more like your muscles are holding a grudge against you for all the bad habits youve been doing for years and now theyre finally saying enough
Cassie Henriques
16 December 2025 - 21:37 PM
Acetylcholine dysregulation + serotonin depletion + ischemic hypoxia cascade = classic trigger point pathophysiology. The local twitch response is the gold standard diagnostic marker because it reflects sarcomere hypercontraction at the motor endplate. Dry needling works because it resets the neuromuscular junction via mechanical disruption. No magic-just neurophysiology.
Also, magnesium glycinate > oxide. Bioavailability matters. And yes, leg length discrepancy? 87% of chronic low back pain patients have it. Pelvic obliquity isn’t myth-it’s biomechanics.
John Brown
17 December 2025 - 04:48 AM
I used to think massage was just for relaxation. Then I found a knot in my glute that was sending pain down my leg like a live wire. One week of tennis ball therapy, daily, and I could finally sit through a movie without shifting every 2 minutes.
It’s not glamorous. It’s not quick. But it’s real. And honestly? More effective than half the meds I’ve taken.
Thanks for the clarity. I’m printing this out.
Benjamin Glover
19 December 2025 - 01:17 AM
Typical American self-help nonsense. In my country, we treat pain with discipline, not balls and stretches. If your muscles hurt, you didn’t train hard enough. Stop coddling yourself.
John Samuel
20 December 2025 - 09:06 AM
As someone who has spent 18 years in clinical pain management, I must commend the precision of this exposition. The delineation between MPS and fibromyalgia is not merely academic-it is clinically decisive. The referred pain patterns, the twitch response, the biochemical milieu-all are elegantly articulated.
Moreover, the emphasis on ischemic compression as first-line intervention aligns with the 2021 Cochrane review on myofascial interventions. The omission of pharmacological dependency as a primary strategy is not only prudent-it is heroic in an era of opioid overreliance.
For those who dismiss self-care: consider this. The human body is not a machine to be fixed, but an ecosystem to be tended. Daily 10-minute ritual? That is not indulgence. It is reverence.
Raj Kumar
21 December 2025 - 19:22 PM
bro i had this pain in my neck for 2 years and no doc ever said trigger point. i thought it was arthritis or something. i used a lacrosse ball on my trap for 30 sec every night and now i can turn my head without wincing. its not that complicated. just be consistent. and yeah vitamin d is huge. got mine checked and it was 19. took 5k daily for 3 months. life changed.
Jocelyn Lachapelle
23 December 2025 - 02:38 AM
My mom had this for 15 years. Doctors called it stress. Said she was imagining it. She found a physical therapist who knew about Travell and Simons. One session with dry needling and she cried because she could sleep on her side again.
It’s not in the textbooks because it’s not profitable. But it’s real. And it’s in us.
Thank you for writing this.
Mike Nordby
24 December 2025 - 14:25 PM
There is a significant body of literature supporting the efficacy of ischemic compression and dry needling, with randomized controlled trials demonstrating clinically meaningful reductions in pain intensity (VAS scores) and improved range of motion. However, the heterogeneity of trigger point localization necessitates individualized palpation protocols. Standardized anatomical diagrams are useful as starting points but lack the sensitivity of manual palpation. Furthermore, the role of micronutrient deficiency as a modulating factor-particularly magnesium and vitamin D-is underappreciated in mainstream clinical practice. This post represents a rare synthesis of evidence-based practice and patient-centered education.
Christina Bischof
24 December 2025 - 15:30 PM
i used to think i was just lazy. turns out i had knots in my shoulders that were making me tired all day. now i roll on a tennis ball before bed. no more 3pm crashes. also stopped chewing gum. jaw pain vanished. small changes. big difference.
Melissa Taylor
26 December 2025 - 10:22 AM
You know what’s wild? The first time I found a trigger point in my own hip, I cried. Not because it hurt-though it did-but because I realized my body had been screaming for years and I’d been too busy to listen.
This isn’t about fixing a problem. It’s about learning to live with your body again. Not against it.
Thank you for giving me the language to understand what was happening. I’m not broken. I’m just holding tension I didn’t know I had.
Sai Nguyen
26 December 2025 - 12:50 PM
India has been doing this for centuries with Ayurveda and pressure points. Why do Americans need a blog post to learn what our grandmothers knew? Massage. Heat. Breath. Simple. You don’t need a ball. You need discipline.