Conjunctivitis Type Checker
Determine Your Conjunctivitis Type
Answer these questions to identify the most likely type of conjunctivitis based on your symptoms and triggers.
Your Results
Key Takeaways
- Allergic conjunctivitis is an eye inflammation driven by the same immune pathways that underlie many systemic allergic and autoimmune conditions.
- IgE antibodies, mast cells, and cytokines form the core cascade that links eye symptoms to disorders such as asthma, atopic dermatitis, and seasonal allergies.
- Accurate diagnosis relies on clinical signs and targeted allergy testing, while treatment blends antihistamine drops, mast‑cell stabilizers, and, for severe cases, immunotherapy.
- Managing co‑existing immune disorders can reduce eye flare‑ups and improve overall quality of life.
- Prevention focuses on environmental control, diet, and regular eye‑care check‑ups.
What Is Allergic Conjunctivitis?
When you hear the term Allergic Conjunctivitis is an inflammation of the thin, transparent membrane (the conjunctiva) that lines the inside of the eyelids and covers the white part of the eye, triggered by an allergic reaction, think of it as the eye’s version of a hay‑fever flare‑up. Redness, itching, tearing, and a gritty feeling are the classic signs. Unlike bacterial or viral infections, the condition is not caused by microbes; instead, the eyes react to allergens such as pollen, pet dander, or mold spores that have entered the ocular surface.
How the Immune System Triggers Eye Allergies
The Immune System a network of cells, tissues, and molecules that defends the body against foreign invaders and maintains internal balance is the hidden driver behind allergic conjunctivitis. When an allergen contacts the eye, specialized immune cells called mast cells sit ready on the Ocular Surface the outermost layer of the eye, which includes the cornea and conjunctiva. These mast cells carry receptors for IgE Antibody a class of immunoglobulin that binds to allergens and flags them for an immune response. When IgE on mast cells recognizes an allergen, it triggers a rapid release of Histamine a chemical messenger that dilates blood vessels, causes itching, and attracts other immune cells and a cocktail of Cytokine signaling proteins that amplify inflammation and recruit additional immune cells. The result is the familiar redness, swelling, and itching of allergic conjunctivitis.
Immune System Disorders Frequently Linked to Allergic Conjunctivitis
Because the same IgE‑mediated pathway fuels other allergic diseases, people with allergic conjunctivitis often have co‑existing immune disorders. Below are the most common companions:
- Asthma a chronic airway disease characterized by bronchial hyper‑responsiveness and inflammation
- Atopic Dermatitis a relapsing skin condition marked by itchy, inflamed patches, often called eczema
- Allergic Rhinitis inflammation of the nasal lining caused by allergens, commonly known as hay fever
- Seasonal Allergies allergic reactions that occur at specific times of the year, typically triggered by pollen
These conditions share a genetic predisposition toward a Th2‑dominant immune response, meaning the body leans heavily on the IgE pathway. When one site (like the eyes) is inflamed, it can amplify the overall allergic load, making other symptoms flare up sooner and harder to control.
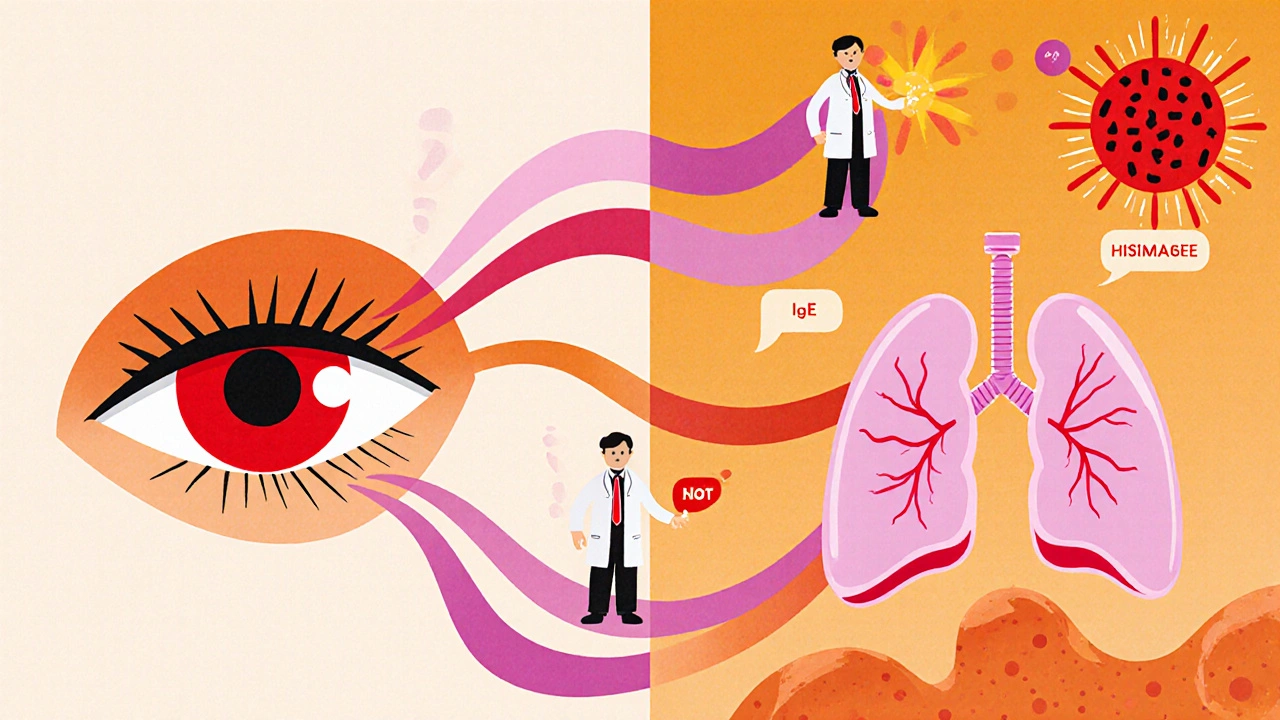
Cellular Players: Histamine, IgE, Mast Cells, and Cytokines
Understanding the key players helps demystify why eye allergies often mirror systemic issues.
- Histamine - Released within minutes of allergen exposure, it binds to H1 receptors on nerve endings, producing itching, and to H2 receptors on blood vessels, causing redness.
- IgE Antibody - Produced by B‑cells after sensitization, IgE circulates at low levels but clings to mast cells, priming them for rapid response.
- Mast Cell - Tissue‑resident cells packed with granules containing histamine, proteases, and cytokines; they act as the first responders.
- Cytokine - Molecules like IL‑4, IL‑5, and IL‑13 sustain the allergic inflammation and recruit eosinophils, another cell type that further damages the conjunctival tissue.
When this cascade repeats day after day-think of living in a high‑pollen environment-the eye’s surface can become chronically irritated, leading to complications such as giant papillary conjunctivitis or even corneal abrasions.
Diagnosing Allergic Conjunctivitis and Its Immune Links
Diagnosis begins with a thorough eye exam, looking for characteristic signs: bright red conjunctiva, papillary bumps on the inner eyelid, and watery discharge. A detailed history-seasonal patterns, exposure to pets, or recent travel-helps pinpoint triggers.
When systemic involvement is suspected, the Skin Prick Test a minimally invasive procedure where tiny amounts of allergens are introduced into the skin to observe a wheal‑and‑flare reaction or specific IgE blood tests can confirm sensitization to pollen, dust mites, or molds. Correlating positive results with eye symptoms strengthens the link between ocular and systemic allergy.
Treatment Options: From Drops to Immunotherapy
Effective management tackles both the symptoms in the eye and the underlying immune hyper‑reactivity.
- Antihistamine Eye Drops - Provide rapid relief by blocking H1 receptors. Examples include olopatadine and ketotifen.
- Mast‑Cell Stabilizers - Prevent degranulation, offering longer‑term control. Cromolyn sodium is a classic choice.
- Corticosteroid Eye Drops - For severe inflammation, a short course of low‑potency steroids (e.g., loteprednol) can quell the reaction, but they must be used under ophthalmic supervision to avoid raised intra‑ocular pressure.
- Oral Antihistamines - Helpful when conjunctivitis accompanies allergic rhinitis or asthma.
- Allergen‑Specific Immunotherapy (ASIT) - Gradual exposure to increasing doses of the culprit allergen can re‑train the immune system, reducing IgE production over months to years. Sublingual tablets for grass‑pollen or injectable shots are the most common formats.
Adjunct measures such as cold compresses, lubricating artificial tears, and strict avoidance of known triggers (e.g., staying indoors on high‑pollen days) round out the treatment plan.

Managing Co‑Existing Immune Disorders
Addressing only the eye symptoms often leads to recurring flare‑ups because the systemic allergic load remains high.
- Asthma Control - Use inhaled corticosteroids and bronchodilators as prescribed; poorly controlled asthma is linked to higher ocular allergy severity.
- Skin Care for Atopic Dermatitis - Regular moisturization and topical steroids reduce overall IgE levels.
- Allergic Rhinitis Management - Intranasal corticosteroids and antihistamine sprays lessen nasal congestion, which in turn reduces eye drainage and irritation.
- Dietary Considerations - A diet rich in omega‑3 fatty acids (found in salmon, flaxseed) and low in processed foods can dampen systemic inflammation.
Integrating these steps makes it easier for the eye’s immune response to stay calm, cutting down on drop usage and improving quality of life.
Prevention and Lifestyle Tips
Prevention is a blend of environmental control and personal habits.
- Keep windows closed and use HEPA filters during peak pollen seasons.
- Rinse eyes with sterile saline after outdoor exposure.
- Wear wrap‑around sunglasses to shield the ocular surface from wind‑borne allergens.
- Change and wash bedding weekly in hot water to reduce dust‑mite load.
- Consider using a dehumidifier to curb mold growth indoors.
Consistent eye‑care check‑ups every 1-2 years help catch early signs of chronic inflammation before they compromise vision.
Comparison of Common Conjunctivitis Types
| Condition | Primary Cause | Typical Symptoms | First‑Line Treatment |
|---|---|---|---|
| Allergic Conjunctivitis | IgE‑mediated response to environmental allergens | Itching, watery discharge, bilateral redness, papillary reaction | Antihistamine or mast‑cell stabilizer eye drops; avoid allergens |
| Viral Conjunctivitis | Contact with adenovirus, often linked to upper respiratory infection | Rash‑like crusting, watery to mucous discharge, often unilateral first | Supportive care - artificial tears, cold compresses; avoid touching eyes |
| Bacterial Conjunctivitis | Colonization by Staphylococcus, Streptococcus, or Haemophilus | Thick yellow‑green discharge, eyelid sticking, often unilateral | Topical antibiotic ointment or drops prescribed by a clinician |
Frequently Asked Questions
Can allergic conjunctivitis cause long‑term eye damage?
Rarely, but chronic inflammation can lead to complications like keratoconjunctivitis sicca (dry eye) or corneal scratches. Prompt treatment and allergen avoidance usually prevent permanent damage.
Is there a cure for allergic conjunctivitis?
There’s no permanent cure because the immune system remains predisposed, but immunotherapy can dramatically reduce symptom frequency and severity, making the condition almost unnoticeable for many patients.
Do eye drops for allergies affect vision?
Most over‑the‑counter antihistamine drops are formulated not to blur vision. However, some people experience temporary slight blurring, especially with thicker gels.
Should I see an ophthalmologist or an allergist first?
Start with an eye‑care professional to rule out infection or other eye disease. If allergies are confirmed, a referral to an allergist for systemic testing and possible immunotherapy is the next step.
Can lifestyle changes alone control allergic conjunctivitis?
Lifestyle tweaks-like using air filters, wearing sunglasses, and maintaining a low‑pollen indoor environment-significantly lower flare‑ups, but most patients still need at least occasional medication.






WILLIS jotrin
22 October 2025 - 17:53 PM
Allergic conjunctivitis is basically the eye's version of a seasonal sniffle, so when pollen spikes you’ll notice the itch and red eyes almost instantly. The mast cells in the conjunctiva act like tiny alarm bells, dumping histamine the moment they spot IgE‑bound allergens. Because the same IgE pathway drives asthma and eczema, a flare‑up in the eyes often signals that the rest of the immune system is on high alert. Keeping a daily antihistamine eye drop on hand can break that loop before the inflammation spreads. Pairing drops with a HEPA filter at home tends to keep the overall allergic load down.
Iris Joy
24 October 2025 - 05:59 AM
Thinking about the overlap with asthma, it helps to view the eye symptoms as a barometer for how well your whole respiratory system is doing. When you step up your inhaled steroid regimen, many people notice a quieter eye response too. It’s worth doing a quick skin‑prick test for the most common indoor allergens-dust‑mite and pet dander often sneak in unnoticed. Once you know the culprits, you can start targeted avoidance, like washing bedding weekly in hot water. Adding omega‑3 rich foods such as salmon or flaxseed can also tone down systemic inflammation. And don’t forget to give your tears a boost with preservative‑free artificial tears during high‑pollen days.
Joe Waldron
25 October 2025 - 18:06 PM
When you look at the cascade-IgE binds to mast cells, histamine is released, cytokines like IL‑4 and IL‑13 recruit eosinophils, and the whole conjunctival surface becomes a battlefield-it's easy to see why a single eye‑drop won't solve everything, you need a multi‑pronged approach, including environmental control, pharmacotherapy, and sometimes immunotherapy, especially for those with persistent seasonal allergies, because the immune system remembers the allergen and amplifies the response each year.
Wade Grindle
27 October 2025 - 05:13 AM
The literature shows that patients who combine mast‑cell stabilizers with antihistamine drops experience fewer rebound flare‑ups than those who rely on antihistamines alone. In addition, long‑term sublingual immunotherapy has been documented to reduce specific IgE levels over a period of six to twelve months, which can translate into fewer eye‑related symptoms. It is advisable to schedule regular follow‑ups with both an ophthalmologist and an allergist to coordinate care. Monitoring intra‑ocular pressure when using corticosteroid drops is also essential to avoid secondary glaucoma. Overall, a coordinated plan yields the best outcomes.
Joanne Ponnappa
28 October 2025 - 17:19 PM
Wow, I didn’t realize how linked eye allergies are to asthma and eczema! 🤯 Keeping windows shut on windy pollen days and using a humidifier can really help. Also, wearing wrap‑around sunglasses isn’t just for style, it actually blocks a lot of the allergens. 🌞 Try rinsing your eyes with sterile saline after being outside – it washes away the tiny particles. Stay safe and keep those drops handy! 😊
Michael Vandiver
30 October 2025 - 05:26 AM
Just keep a pair of cold compresses at your desk for instant relief.
Emily Collins
31 October 2025 - 17:33 PM
Cold compresses are a lifesaver, especially when the itch feels like a thousand tiny needles dancing across the surface of your eye, and the sudden coolness can actually shrink those dilated blood vessels for a few precious minutes of calm.
Harini Prakash
2 November 2025 - 05:39 AM
In my experience, the biggest improvement came after I started a nightly routine of cleaning the bedroom thoroughly and running a HEPA filter for a few hours before sleep; the reduced dust‑mite load made a noticeable difference in both my nasal congestion and eye itchiness. I also found that sipping warm ginger tea with a dash of honey in the evenings helped soothe the overall inflammation, likely due to ginger’s natural anti‑histamine properties. If you haven’t already, consider discussing a low‑dose oral antihistamine with your doctor to cover systemic triggers while you continue using eye drops locally.
Rachael Turner
3 November 2025 - 17:46 PM
It’s easy to forget that diet plays a role, but meals rich in antioxidants and omega‑3 fatty acids can dampen the cytokine storm that fuels chronic eye irritation. Cutting back on processed foods and adding leafy greens may not cure the allergy, yet many patients report fewer flare‑ups after a few weeks of the change. Consistency is key, so keep a simple food diary to track what helps.
Suryadevan Vasu
5 November 2025 - 05:53 AM
Allergy testing pinpoints exact triggers. Use that info to tailor avoidance strategies. Combine drops with environmental control for best results.
Diane Thurman
6 November 2025 - 17:59 PM
Allergic conjunctivitis often gets dismissed as a minor annoyance, but when you dig into the immunology it reveals a complex network that mirrors systemic allergic disease. The IgE antibodies that sit on mast cells in the conjunctiva are the same molecules that trigger asthma attacks and atopic dermatitis flares. When these antibodies recognize an allergen, they cause the mast cells to release histamine, leukotrienes, and a swarm of cytokines that amplify the local inflammatory response. This cascade not only makes the eyes red and itchy, it also sends signals to the rest of the immune system, raising overall IgE levels. Consequently, a person with uncontrolled asthma may notice that their eye symptoms worsen during an asthma exacerbation, creating a vicious feedback loop. Environmental control is therefore a cornerstone of management; removing or reducing exposure to the offending allergen cuts the initial trigger for the whole cascade. Simple measures such as using high‑efficiency particulate air (HEPA) filters, keeping windows shut on high‑pollen days, and washing bedding in hot water can lower indoor allergen loads dramatically. Pharmacologically, antihistamine eye drops provide quick relief by blocking H1 receptors, but they do not address the underlying mast‑cell activation. Mast‑cell stabilizers, on the other hand, prevent degranulation and are essential for long‑term control, especially in patients who experience daily exposure. For moderate to severe cases, short courses of low‑potency corticosteroid drops can quell acute inflammation, but they must be monitored to avoid increasing intra‑ocular pressure. Immunotherapy, either sublingual tablets or subcutaneous injections, offers the most disease‑modifying potential by gradually desensitizing the immune system to specific allergens. Studies have shown that after two years of consistent immunotherapy, many patients experience a 30‑40% reduction in both ocular and respiratory allergy symptoms. Lifestyle factors also play an underrated role; a diet rich in omega‑3 fatty acids, regular aerobic exercise, and adequate sleep can all help regulate cytokine production. Finally, coordinated care between an ophthalmologist, allergist, and primary care physician ensures that treatment plans are synchronized, reducing the risk of over‑medication and side‑effects. In summary, treating allergic conjunctivitis as an isolated eye problem ignores its systemic roots, and a comprehensive approach that blends avoidance, pharmacotherapy, and immunotherapy yields the best long‑term outcomes.