Cognitive Impairment Duration Calculator
Enter Your Dose Information
How This Works
First-generation antihistamines like Benadryl cross the blood-brain barrier and block histamine receptors, causing drowsiness. According to clinical studies, cognitive impairment can last:
- 6-12 hours for 12.5 mg doses
- 10-18 hours for 25 mg doses
- 14-18 hours for 50 mg doses
Have you ever taken Benadryl for allergies, only to feel like you’ve been hit by a bus the next morning? Or maybe you used it to help you sleep, but woke up groggy, dry-mouthed, and struggling to focus at work? You’re not alone. First-generation antihistamines like diphenhydramine, chlorpheniramine, and promethazine are everywhere-shelves in drugstores, medicine cabinets, even online ads promising quick relief. But behind the convenience is a hidden cost: severe drowsiness and brain fog that can last hours, sometimes even into the next day.
Why These Medications Make You Sleepy
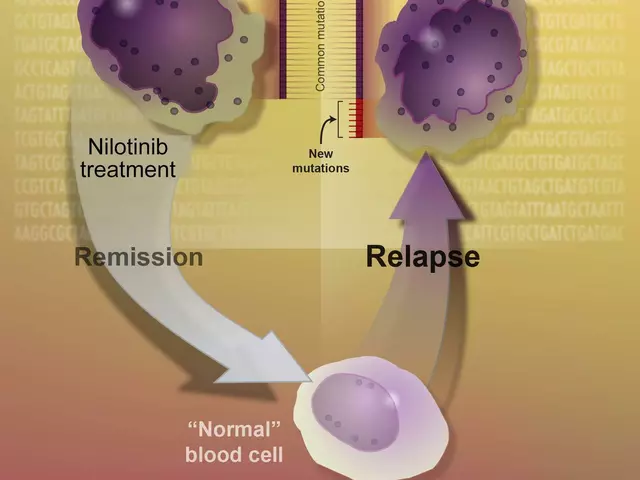
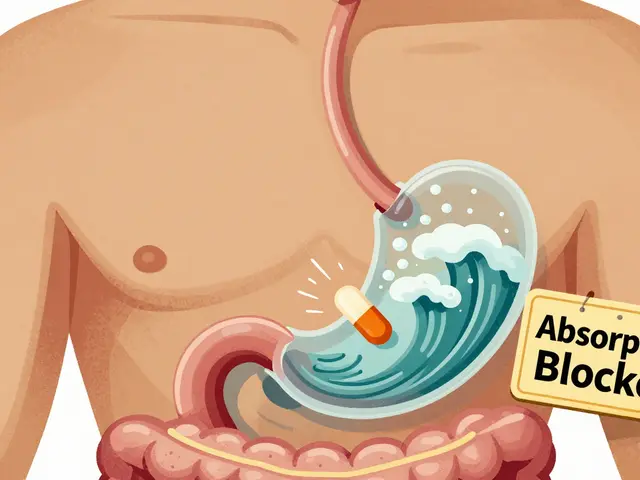
First-generation antihistamines work by blocking histamine, a chemical your body releases during allergic reactions. But here’s the catch: they don’t stop at the allergy sites. These drugs are small, oily molecules that slip easily through the blood-brain barrier. Once inside your brain, they bind to histamine receptors that help keep you alert. When those receptors are blocked, your brain slows down. That’s not just mild tiredness-it’s full-blown sedation. Studies show that after taking a standard 25-50 mg dose of diphenhydramine, brain concentrations reach 15-25 ng/mL within a couple of hours. Compare that to second-generation antihistamines like cetirizine or loratadine, which stay below 1 ng/mL in the brain. That’s a 15-to-25-times difference. No wonder one feels awake and the other feels like a zombie. The sedation isn’t just a side effect-it’s the main reason these drugs were originally used for insomnia. In fact, many people still take them for sleep because they work quickly. But if you’re using them nightly, you’re not just sleeping-you’re poisoning your brain’s natural alertness system.Anticholinergic Effects: More Than Just Dry Mouth
Beyond drowsiness, these drugs have another dangerous side effect: anticholinergic activity. That means they also block acetylcholine, a neurotransmitter involved in memory, muscle control, digestion, and bladder function. It’s not a coincidence that the same molecules that block histamine also bind tightly to muscarinic receptors-about 45% of their structure is similar. The result? A laundry list of uncomfortable and sometimes dangerous symptoms:- Extremely dry mouth, so bad some people need artificial saliva
- Blurred vision and trouble focusing on screens or reading
- Difficulty urinating or feeling like your bladder won’t empty
- Constipation that doesn’t go away
- Confusion, memory lapses, and trouble concentrating-even when you’re awake
Who Uses Them-and Why It’s Risky
You might think these drugs are only for allergy sufferers. But they’re also used for motion sickness, nausea, colds, and sleep. That’s why 45 million Americans use them every year, mostly over the counter. They’re cheap-about $5 for 24 tablets of diphenhydramine-while second-generation options like Zyrtec or Claritin cost three times as much. But here’s the problem: most people don’t realize how long the effects last. Studies show cognitive impairment from these drugs can persist for up to 18 hours after a single dose. That means if you take it at 8 p.m., you could still be impaired at 2 p.m. the next day. And that’s dangerous if you’re driving, operating machinery, or even just trying to work. Emergency data backs this up. In 2021, 35% of drowsy-driving crashes involved first-generation antihistamines. That’s more than alcohol in some age groups. And it’s not just adults. Between 2018 and 2022, pediatric emergency visits for diphenhydramine misuse rose 27%. Kids accidentally overdose because the packaging doesn’t scream “danger”-it says “sleep aid” or “allergy relief.”
Real People, Real Consequences
Reddit threads are full of stories like this one: “Took Benadryl for hives at 8 p.m. Woke up at 2 p.m. the next day feeling like I’d been hit by a truck. Not worth it for mild allergies.” That’s not an exaggeration. On Drugs.com, 38% of users report “extreme sleepiness,” and 22% say they couldn’t concentrate at all. Elderly users are even more vulnerable. A 2022 survey of over 1,200 seniors found that while 65% said diphenhydramine helped them sleep, 42% admitted to morning confusion lasting 3-4 hours. Some reported forgetting where they put their keys, missing appointments, or feeling disoriented. One woman wrote: “I thought I was just getting older. Turns out it was the pills I took every night to sleep.” And it’s not just memory. Long-term users on WebMD forums report urinary issues-trouble starting to pee, feeling like they’re never done. That’s anticholinergic bladder dysfunction. It’s not rare. One in four chronic users experiences it.When Are They Actually Worth It?
Let’s be clear: these drugs aren’t useless. They’re powerful-and in some cases, they’re the best tool for the job. For motion sickness, first-generation antihistamines like dimenhydrinate (Dramamine) are more effective than newer options. For short-term insomnia, if you’re only taking it once or twice a week and you’re not driving the next day, they can help you fall asleep faster-by 30-40 minutes, on average. But here’s the rule: if you need to be alert, don’t use them. No exceptions. If you’re a truck driver, a nurse, a student taking an exam, or a parent watching kids after school-choose something else. The FDA warns that these drugs impair driving ability for up to six hours. Real-world data says it’s longer.What to Use Instead
Second-generation antihistamines like cetirizine (Zyrtec), loratadine (Claritin), and fexofenadine (Allegra) are the new standard. They’re just as good for allergies, but they barely enter the brain. Their sedation index? Around 0.1-0.3, compared to 0.7-0.9 for first-gen drugs. That’s the difference between feeling a little tired and feeling drugged. They cost more, yes. But if you’re paying for lost productivity, accidents, or long-term brain health, they’re cheaper in the long run. For sleep, consider melatonin, magnesium, or cognitive behavioral therapy for insomnia (CBT-I). These don’t mess with your brain chemistry the same way. For motion sickness, ginger capsules or scopolamine patches are safer long-term options.
How to Use Them Safely (If You Must)
If you’re going to use a first-generation antihistamine, follow these rules:- Take it only at night-never during the day.
- Never combine it with alcohol, benzodiazepines, or opioids. It triples the sedation risk.
- Start with the lowest dose (12.5 mg for diphenhydramine).
- Don’t use it for more than 3-5 nights in a row.
- Check your other meds. Many cold pills, pain relievers, and sleep aids already contain diphenhydramine. You could be doubling up without knowing it.
- If you’re over 65, avoid them entirely. The risks far outweigh any benefit.
The Future: Are These Drugs Disappearing?
The tide is turning. The UK banned over-the-counter sales of promethazine to minors in 2022. The FDA is considering similar restrictions on diphenhydramine. Pharmaceutical companies are developing “third-generation” antihistamines that block allergies without crossing into the brain. Two are already in Phase II trials, showing 80% less brain penetration. Market analysts predict a 15-20% drop in OTC sales by 2030 as people wake up to the risks. But until then, these drugs are still on every shelf, still marketed as harmless, still taken by millions who don’t know what they’re really doing to their brains. You don’t need to be a doctor to understand this: if a pill makes you so sleepy you can’t think clearly, it’s not helping you-it’s hurting you. And the damage doesn’t always show up right away. Sometimes, it shows up years later-in memory loss, confusion, or a diagnosis you never saw coming. Ask yourself: Is a quick fix worth your focus, your safety, your future?Why do first-generation antihistamines cause drowsiness?
They easily cross the blood-brain barrier and block histamine receptors in the brain that regulate wakefulness. Unlike second-generation antihistamines, which are designed to stay out of the brain, first-generation ones like diphenhydramine and chlorpheniramine penetrate deeply, slowing down brain activity and causing intense sedation.
Can these drugs cause long-term brain damage?
Yes, especially in older adults. Chronic use of first-generation antihistamines increases dementia risk by 54%, according to the American Geriatrics Society. Their anticholinergic effects reduce acetylcholine activity, a key neurotransmitter for memory and learning. Even occasional use adds up over time, contributing to cognitive decline.
Is it safe to drive after taking Benadryl?
No. Studies show driving impairment from diphenhydramine lasts up to 18 hours after a single dose. The FDA warns it affects reaction time and alertness for at least six hours. In 2021, 35% of drowsy-driving crashes involved first-generation antihistamines-more than many people realize.
What are the signs of anticholinergic toxicity?
Signs include dry mouth, blurred vision, difficulty urinating, constipation, confusion, rapid heartbeat, and flushed skin. In older adults, it can mimic dementia. If you experience these symptoms after taking an antihistamine, stop the medication and talk to your doctor.
Are there safer alternatives for allergies and sleep?
For allergies, use second-generation antihistamines like cetirizine (Zyrtec), loratadine (Claritin), or fexofenadine (Allegra)-they’re just as effective with minimal drowsiness. For sleep, try melatonin, magnesium, or cognitive behavioral therapy for insomnia (CBT-I). These don’t disrupt brain chemistry the same way and are safer for long-term use.
Why are these drugs still sold over the counter?
They’re cheap, widely available, and effective for short-term use. Many people don’t know the risks, and manufacturers aren’t required to highlight them strongly on OTC packaging. But regulators are starting to act-some countries have restricted sales to minors, and the FDA is reviewing stronger warnings.
Should I stop using diphenhydramine if I take it for sleep?
If you use it nightly, yes. Long-term use increases dementia risk and can cause next-day cognitive fog, urinary issues, and dependency. If you need help sleeping, talk to your doctor about safer options like melatonin or CBT-I. Occasional use (once or twice a week) is less risky, but still not ideal.





Colin L
30 December 2025 - 11:52 AM
Man, I took Benadryl last week for a rash and woke up at 3 PM the next day thinking it was still night. My cat was staring at me like I’d been possessed. I didn’t even remember getting out of bed. That’s not sleep, that’s a chemical hostage situation. And don’t get me started on how dry my mouth felt-like I’d been chewing sandpaper for six hours. I thought I was just old, turns out I was just poisoned by a $5 pill. Now I keep Zyrtec in my bag like a survival kit. Don’t be like me.
Henry Ward
31 December 2025 - 07:36 AM
Anyone who still uses first-gen antihistamines is either ignorant or self-sabotaging. This isn’t ‘mild drowsiness’-it’s neurochemical sabotage. You’re not ‘just sleeping better,’ you’re rewiring your brain for cognitive decline. The FDA’s warnings are there for a reason. If you’re taking this for sleep, you’re not lazy-you’re stupid. And if you’re driving after? Congrats, you’re a walking liability. Stop pretending these are ‘safe OTC options.’ They’re not. They’re slow-motion brain damage with a cute label.
Joseph Corry
31 December 2025 - 12:53 PM
It’s fascinating how pharmacologically naive society has become. We treat psychoactive substances like dietary supplements-when in reality, anticholinergic burden is a silent epidemic. The blood-brain barrier isn’t a suggestion, it’s a biological firewall. And yet, we casually breach it with diphenhydramine like it’s chamomile tea. The real tragedy isn’t the sedation-it’s the normalization of neurotoxicity under the banner of convenience. We’ve outsourced our cognitive sovereignty to pharmacy shelves.
Cheyenne Sims
31 December 2025 - 17:27 PM
There is no excuse for the continued over-the-counter availability of these drugs. The data is clear. The risks are documented. The consequences are irreversible in elderly populations. This is not a matter of personal choice-it is a public health failure. Manufacturers must be held accountable. Regulators must act. And consumers must be educated-not with vague disclaimers, but with bold, unambiguous warnings. If you can’t spell out the danger, you shouldn’t be selling it.
Shae Chapman
2 January 2026 - 00:02 AM
OMG I JUST REALIZED I’VE BEEN TAKING THIS FOR YEARS 😭 I thought it was just ‘me being tired’ but nooo… it was the pills. I forgot my kid’s birthday last year because I was ‘too foggy’ 😭 I switched to melatonin and I feel like a new person 🙏✨ thank you for this post-this changed my life 💖
Nadia Spira
3 January 2026 - 05:00 AM
Let’s be real: if you’re using first-gen antihistamines for sleep, you’re not solving insomnia-you’re medicating your inability to practice good sleep hygiene. You’re outsourcing your neurobiology to a $5 chemical crutch. And now you’re surprised you can’t focus? Congratulations, you’ve turned your prefrontal cortex into a ghost town. CBT-I isn’t ‘hard’-it’s the only thing that doesn’t chemically castrate your cognition.
henry mateo
3 January 2026 - 05:52 AM
damn i took benadryl for my allergies last month and i was so out of it i forgot to pay my rent… i thought i was just stressed but now i realize it was the pill. i switched to claritin and i feel like my brain came back. i’m sorry for all the times i snapped at people when i was foggy. my bad. 🙏
Kunal Karakoti
4 January 2026 - 14:28 PM
There is a philosophical tension here: convenience versus consciousness. We have the power to alter our neurochemistry with a single pill, yet we rarely ask: who are we becoming when we do? The body remembers. The brain remembers. And when we trade presence for relief, we are not healing-we are silencing. Perhaps the real allergy is to discomfort itself.
Kelly Gerrard
5 January 2026 - 19:11 PM
This is why we need regulation not recommendations. People are dying because they don’t know the risks. This isn’t opinion. This is science. Stop letting corporations profit from ignorance. Ban these drugs from OTC shelves. Period. End of story.
Glendon Cone
7 January 2026 - 13:18 PM
Big shoutout to the person who posted this. I used to take diphenhydramine every night to sleep. Felt like a zombie by 10 AM. Switched to magnesium + 10mg melatonin and now I wake up actually refreshed. No more brain fog, no more dry mouth. My wife says I’ve been ‘less grumpy’ too 😅. If you’re using these, just try swapping for a week. You’ll be shocked. Your future self will thank you 🙌
Aayush Khandelwal
7 January 2026 - 23:12 PM
It’s wild how we treat the CNS like a vending machine. Push a button, get sleepy. But the brain doesn’t have an ‘off’ switch-it has a rhythm. First-gen antihistamines don’t just quiet the noise, they smash the entire symphony. And then we wonder why we feel ‘off’ for days. The body doesn’t forgive ignorance. It just accumulates debt.
Sandeep Mishra
9 January 2026 - 00:36 AM
Hey, I’m a nurse in Delhi and I see this every day. Grandmas take Benadryl for ‘sleep’ because it’s cheap. Grandpas take it for ‘stomach issues’-not knowing it’s causing urinary retention. We’re not just treating symptoms-we’re creating new ones. Please, if you’re reading this and you’re over 50: talk to your doctor. Don’t let a $5 pill steal your memory. You’re worth more than convenience.
Hayley Ash
10 January 2026 - 05:06 AM
Oh wow, so now we’re calling people stupid for using OTC meds? Next you’ll tell me caffeine is a gateway drug. Maybe the real problem is that you’ve never had a real allergy. Try breathing through a pollen storm for a week and then come back with your ‘neurochemical sabotage’ lecture. Some of us don’t have the luxury of $30/month prescriptions. Not everyone lives in your bubble.