Take a pill. Swallow it. Wait for it to work. Seems simple, right? But for millions of people, that simple act doesn’t guarantee the medicine will do what it’s supposed to. The problem isn’t the drug itself-it’s what happens inside the gut. Gastrointestinal medications face a brutal gauntlet before they ever reach your bloodstream. And if they don’t make it through, they’re useless.
Why Your Stomach and Intestines Fight Your Medication
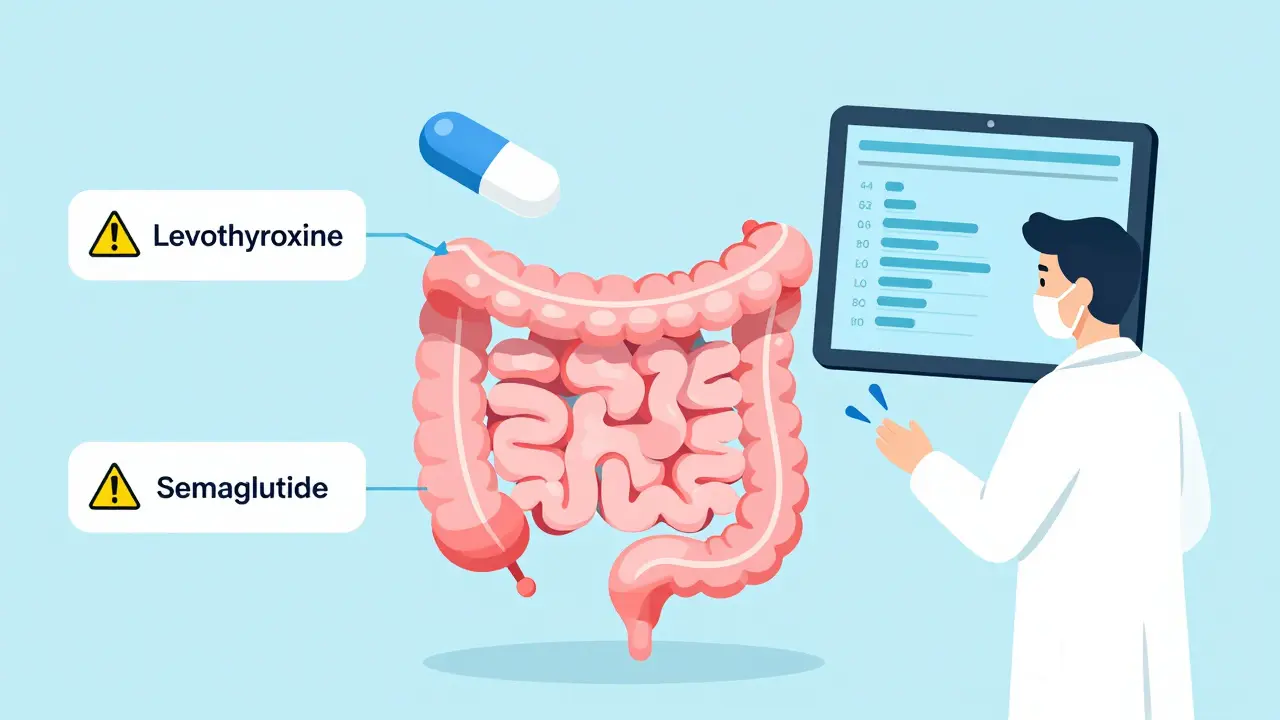
Your digestive system isn’t designed to let drugs pass through easily. It’s built to break down food, not deliver medicine. The stomach’s acid can destroy pills before they even start. The intestinal lining? It’s packed with defense mechanisms: thick mucus, tight junctions between cells, and pumps that kick drugs right back out. These aren’t bugs-they’re features. Your body’s trying to keep toxins out. But that same system blocks life-saving drugs too.Take levothyroxine, the thyroid hormone replacement. If you take it with breakfast, especially something fatty, your body absorbs 30-50% less of it. That’s not a small drop. It’s enough to throw your entire hormone balance off. That’s why doctors tell you to take it on an empty stomach-because your gut doesn’t care about your schedule.
And it’s not just food. The pH of your gut changes as you move down. Your stomach is acidic, around pH 2. By the time you hit the lower small intestine, it’s nearly neutral, around pH 8. Some drugs dissolve only in acid. Others need alkaline conditions. If your gut pH is off-because of antacids, infections, or disease-your drug might not dissolve at all. No dissolution? No absorption. No effect.
The Silent Killer: First-Pass Metabolism
Even if your pill makes it past the stomach and dissolves in the intestine, it’s not home free. The blood from your gut doesn’t go straight to your heart. It goes first to your liver. And your liver? It’s a chemical factory that loves to destroy drugs before they can do their job.This is called first-pass metabolism. For some medications, up to 90% of the dose gets wiped out before it ever reaches your bloodstream. That’s why drugs like nitroglycerin are given under the tongue-not swallowed. That’s why some pills are dosed at 10 times the strength of their injectable version. Your liver is stealing most of it.
And it’s not the same for everyone. Some people have more liver enzymes. Others have genetic variations that make them process drugs faster or slower. That’s why two people taking the same dose of the same pill can have wildly different results. One feels better. The other feels nothing.
When Disease Makes Medication Fail
If you have Crohn’s disease, ulcerative colitis, or short bowel syndrome, your gut isn’t just inefficient-it’s broken. Inflammation damages the lining. Scar tissue reduces surface area. Surgery removes parts of the intestine entirely. All of this cuts down the space where drugs can be absorbed.Take mesalamine, a common drug for ulcerative colitis. In healthy people, it works fine. But in someone with severe inflammation, bioavailability drops by 25-40%. The drug doesn’t reach the colon where it’s needed. It gets absorbed too early-or not at all. That’s why some patients on mesalamine still have flare-ups. It’s not that the drug doesn’t work. It’s that their body won’t let it work.
And then there’s the problem of transit time. In irritable bowel syndrome, food moves too fast or too slow. If it moves too fast, drugs don’t have time to absorb. If it moves too slow, they sit in the gut too long and get broken down. One patient on a forum described how her warfarin dose stayed the same, but her INR swung from 1.5 to 4.5-dangerously low to dangerously high-just because her gut motility changed. No one changed her pills. Her gut did.

Big Drugs, Bigger Problems
Most pills are small molecules that slip through the gut lining easily. But the future of medicine is big. Biologics. Peptides. Monoclonal antibodies. These are molecules too large, too polar, too fragile to survive digestion. Insulin, for example, is a protein. If you swallow it, your stomach digests it like chicken soup. That’s why insulin shots exist.But now, new drugs like semaglutide (Ozempic, Wegovy) are being developed as oral pills. How? They use absorption enhancers-chemicals that temporarily open the tight junctions in your gut lining. It’s like giving your intestine a key to let the drug through. But here’s the catch: these enhancers aren’t selective. They let everything through. That means if you take another pill at the same time-say, an antibiotic or a blood thinner-it might get absorbed too much. Too fast. Too strong. Dangerous levels.
Studies show semaglutide can reduce absorption of other drugs by 15-30%. For drugs with a narrow therapeutic window-where the difference between help and harm is tiny-that’s a serious risk. Pharmacists now have to ask: “Are you taking Ozempic? What else are you on?” It’s no longer just about the drug. It’s about the whole gut ecosystem.
Formulation Matters More Than You Think
Not all pills are created equal. Two versions of the same drug can behave completely differently because of how they’re made. Is it a tablet? A capsule? A delayed-release? A coated bead? These aren’t just packaging choices. They’re delivery systems.Take extended-release metformin. If you crush it, you destroy the slow-release mechanism. You get a spike in blood levels-then a crash. That’s why you’re told not to crush it. Same with enteric-coated aspirin. If the coating breaks down too early, it irritates your stomach. If it doesn’t break down at all, the drug never gets absorbed.
And then there’s the new wave: nanoparticles, liposomes, lipid carriers. These tiny packages protect drugs from digestion and help them slip through the gut wall. In lab tests, they’ve boosted bioavailability by 1.5 to 3.5 times for drugs that used to barely work. But these aren’t widely available yet. Only 15-20% of oral drugs on the market have special labeling for patients with GI disease. Most doctors don’t even know these options exist.
What You Can Do
If you’re on gastrointestinal meds and they’re not working, don’t assume it’s you. It might be your gut. Here’s what to check:- Timing matters. Take drugs on an empty stomach if instructed. Wait 30-60 minutes before eating.
- Watch your food. Fatty meals slow gastric emptying. Avoid them with drugs like levothyroxine or certain antibiotics.
- Don’t mix meds. If you’re on semaglutide or other absorption-altering drugs, space out other pills by at least 2 hours.
- Ask about formulations. Is there a liquid, chewable, or extended-release version that might work better for your condition?
- Track your symptoms. Keep a log: when you took the drug, what you ate, how you felt. Patterns matter.
And if you have a chronic GI condition, ask your pharmacist or gastroenterologist: “Does this drug have special instructions for my condition?” Most labels don’t say. But experts do.
The Future Is Personalized
Scientists are now building digital models of individual guts-simulating pH, transit time, inflammation, and enzyme levels-to predict how a drug will behave in a specific person. Early trials are testing smart capsules that send back data on pH and pressure as they move through the GI tract. Imagine a pill that tells your doctor: “I reached the colon, but the lining is inflamed. Absorption is low.” That’s not sci-fi. It’s coming.Right now, we treat GI meds like they’re one-size-fits-all. They’re not. Your gut is unique. Your disease is unique. Your absorption is unique. Until we start treating it that way, we’ll keep seeing patients who take their pills faithfully-and still feel worse.
Why This Isn’t Just a Patient Problem
This isn’t just about people struggling to feel better. It’s about the entire drug development system. Pharmaceutical companies spend billions developing drugs, then find out too late that they don’t work in real patients because of gut absorption issues. That’s why 65% of new drug applications now include models of diseased guts before they even hit clinical trials.The market for absorption enhancers is growing fast-projected to hit $2.8 billion by 2027. But until doctors, pharmacists, and patients understand how the gut works, we’ll keep missing the mark. Medication failure isn’t always about the drug. Sometimes, it’s about the delivery system. And that system? It’s inside you.



Shanahan Crowell
4 January 2026 - 17:48 PM
This is wild-I had no idea my thyroid med was getting wrecked by my morning avocado toast! 🤯 I always thought it was just me being lazy, but now I get it: my gut’s a hostile takeover zone for pills. I’m switching to 6 a.m. fasting from now on-no exceptions. Thanks for the wake-up call!
Kerry Howarth
4 January 2026 - 23:28 PM
Timing and formulation matter more than dosage. Simple. Stop blaming yourself. Start tracking.
Joy F
6 January 2026 - 16:40 PM
Let’s be real: the pharmaceutical-industrial complex doesn’t want you to know your gut is a sentient, judgmental entity that rejects your meds based on your breakfast choices. It’s not chemistry-it’s cosmic karma. Your liver is judging your life choices, and your tight junctions? They’re basically the bouncer at a club that won’t let your drugs in unless you’re wearing the right metaphorical suit. Semaglutide? That’s not a drug-it’s a Trojan horse for the entire GI ecosystem. And now we’re all just collateral damage in the war between biology and Big Pharma’s PowerPoint presentations. 😌✨
Haley Parizo
7 January 2026 - 07:21 AM
You’re all missing the point. This isn’t about pills or pH levels. It’s about the collapse of the human body’s autonomy in the face of corporate medicine. We’ve turned our biology into a broken vending machine: insert dollar, get pill, hope for result. But your gut doesn’t care about your insurance plan. It doesn’t care about your compliance. It remembers every antacid, every greasy meal, every rushed pill you swallowed without water. This isn’t pharmacology-it’s a spiritual reckoning. Your body is screaming. Are you listening? Or are you still scrolling through TikTok while your levothyroxine dissolves into nothing?
Ian Detrick
7 January 2026 - 22:03 PM
I’ve been on metformin for 12 years and never realized crushing it was a disaster. I used to do it because the pills were huge. Now I feel like a dumbass. But also… nanoparticles? Liposomes? This is the future. Why aren’t we talking about this more? I want to know what’s in the pipeline-this isn’t just about me, it’s about everyone with Crohn’s, IBS, or just a weirdly sensitive gut. We need a movement.
Brittany Wallace
7 January 2026 - 22:17 PM
OMG YES. I’ve been tracking my INR and meals for months and finally figured out why it spiked after I started eating chia pudding. My gut’s a drama queen. 🥺 I started spacing my meds 2 hours from food and now I’m not scared to leave the house. Thank you for validating what felt like madness. 🤗
Palesa Makuru
9 January 2026 - 15:35 PM
Actually, in South Africa, we don’t even have access to most of these fancy formulations. People are just taking generic pills with maize porridge and wondering why they’re still sick. This whole discussion feels like a luxury problem for Americans with $200 prescriptions. Meanwhile, my cousin with TB is taking his meds with sugary tea because that’s all he can afford. Maybe we should fix access before we optimize absorption?
Lori Jackson
10 January 2026 - 14:35 PM
Let me guess-you also believe in ‘healing crystals’ and ‘gut intuition.’ This isn’t mysticism. It’s science. And if you can’t follow basic instructions like ‘take on empty stomach,’ don’t blame the drug. Blame your inability to read. You’re not special. Your gut isn’t ‘unique.’ You’re just lazy. And now you’re spreading misinformation under the guise of ‘personalized medicine.’ Pathetic.
veronica guillen giles
12 January 2026 - 07:43 AM
Oh sweetie, you think *you’re* the problem? Honey, the entire medical system is designed to make you feel broken so you’ll keep buying pills. They don’t want you to know that your body is fine-it’s the drugs that are the glitch. Ever heard of a placebo? Maybe your gut is rejecting the *idea* of being sick. Just sayin’… 🤷♀️
Ian Ring
14 January 2026 - 00:48 AM
Interesting read. I’ve had ulcerative colitis since 2015, and I can confirm: mesalamine failed me until I switched to the delayed-release capsules instead of the tablets. Took me three years to figure it out. Also-yes, spacing meds by 2 hours with Ozempic is non-negotiable. My pharmacist flagged it. Most doctors don’t. So… talk to your pharmacist. They’re the real MVPs. 🙏
erica yabut
14 January 2026 - 15:52 PM
Ugh. Another ‘gut is a sentient being’ essay. Can we please stop anthropomorphizing our intestines? It’s not a drama queen-it’s a biological machine with enzymatic pathways, receptor densities, and permeability gradients. If your drug isn’t working, get a TDM (therapeutic drug monitoring) test. Or better yet-stop blaming your colon and start taking responsibility. Your gut doesn’t care about your trauma. It cares about pH, transit time, and bioavailability. Fix the variables. Not your mindset.
Vincent Sunio
15 January 2026 - 02:01 AM
This article is fundamentally misleading. Absorption variability is not ‘unique’ to each individual-it’s quantifiable, predictable, and modeled in pharmacokinetics. The notion that ‘your gut is special’ is pseudoscientific nonsense. The real issue is inadequate clinical trial stratification. If 65% of new drugs now include GI models, why are we still treating patients as if they’re blank slates? The problem isn’t patient ignorance-it’s systemic negligence in drug development. And no, ‘tracking your symptoms’ is not a substitute for proper dosing protocols based on pharmacogenomics.
JUNE OHM
17 January 2026 - 00:52 AM
THEY’RE DOING THIS ON PURPOSE. They want you dependent. Semaglutide? That’s not for weight loss-it’s a bioweapon to control your gut microbiome. They’re testing absorption enhancers to open your gut so they can inject nanobots or track your emotions. You think your INR swings are random? They’re watching. They’re mapping. They’re building a database of your digestion. Don’t be fooled. Take your meds. But don’t trust them. 🚨👁️