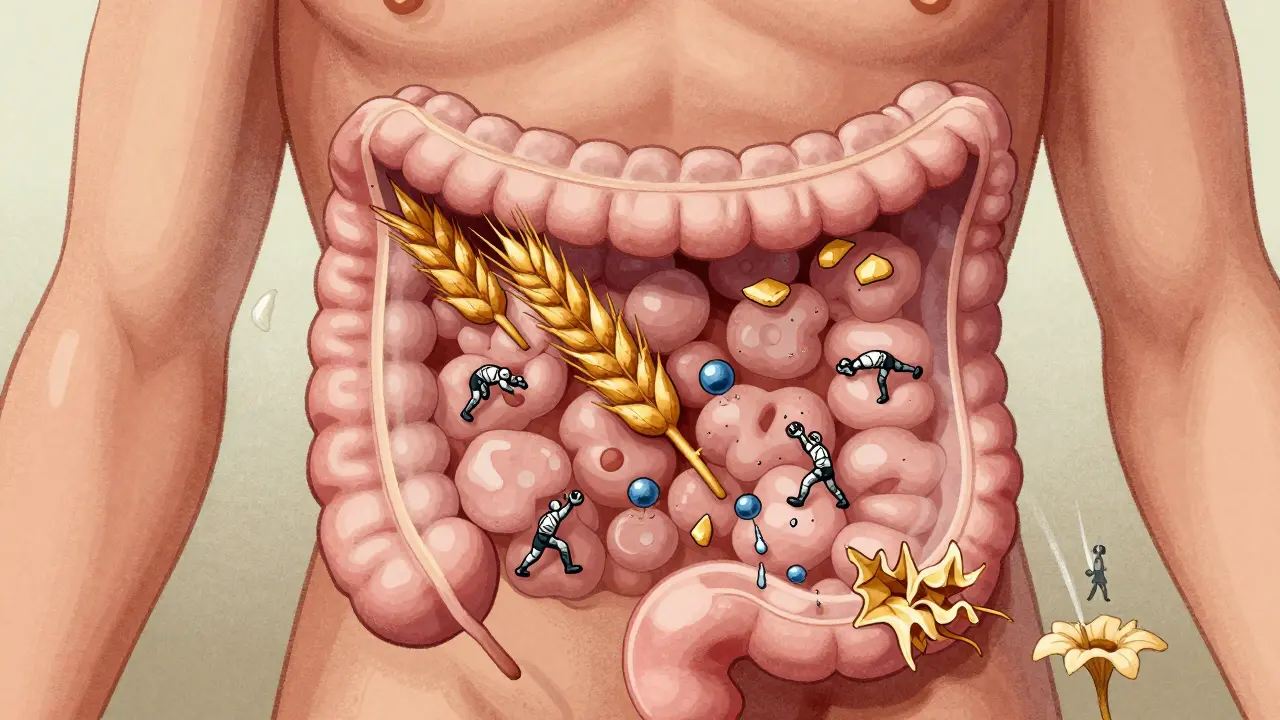
When you eat bread, pasta, or beer, your body usually breaks down the gluten without a second thought. But for about 1 in 100 people, that same bite triggers a silent war inside their intestines. This isn’t a food allergy. It’s celiac disease - a genetic autoimmune disorder where the immune system turns against the body’s own tissues. And the trigger? Gluten.
What Happens When Someone with Celiac Disease Eats Gluten
Gluten isn’t just a protein in wheat. It’s a group of proteins - gliadin and glutenin - that resist normal digestion. In people with celiac disease, fragments of gliadin, especially a stubborn 33-amino-acid piece called the 33-mer, slip through the gut lining. This doesn’t happen by accident. Gluten causes cells in the intestinal wall to release zonulin, a protein that opens the tight junctions between cells like a drawbridge. Suddenly, these gluten fragments are in the wrong place - inside the gut wall, where they shouldn’t be.
That’s when tissue transglutaminase 2 (TG2), an enzyme normally involved in wound healing, jumps into action. It chemically modifies the gluten fragments, adding negative charges that make them stick like magnets to special immune molecules called HLA-DQ2 or HLA-DQ8. These molecules are found on immune cells, and they’re the reason celiac disease runs in families. If you don’t have one of these gene variants, you won’t develop celiac disease - no matter how much gluten you eat.
Once the modified gluten is presented to the immune system, T-cells go into overdrive. They release interferon-gamma and interleukin-21, signaling molecules that turn the gut lining into a war zone. The finger-like projections in the small intestine - called villi - start to flatten. The crypts deepen. Immune cells flood in. This damage reduces your ability to absorb nutrients, leading to fatigue, anemia, weight loss, and even osteoporosis over time.
What’s new since 2024? Research from McMaster University showed the gut lining itself isn’t just a passive victim. Cells in the epithelium can actually express the same immune molecules (MHC class II) that trigger the attack. This means the gut doesn’t just get damaged - it helps start the fire.
Celiac Disease vs. Gluten Sensitivity: The Key Differences
Many people think they have celiac disease because they feel better on a gluten-free diet. But not all gluten-related issues are the same. Non-celiac gluten sensitivity (NCGS) affects up to 13% of people in some regions, but it’s not autoimmune. There’s no villous atrophy, no tissue transglutaminase antibodies, and no genetic marker.
Here’s how they break down:
- Celiac disease: Autoimmune, causes intestinal damage, positive tTG-IgA blood test, HLA-DQ2/DQ8 positive, requires lifelong strict gluten-free diet.
- Non-celiac gluten sensitivity: No autoimmune damage, no specific biomarkers, symptoms improve with gluten removal, but tolerance can vary. Some people with NCGS can eat small amounts of gluten without harm.
The blood test for celiac disease - anti-tissue transglutaminase (tTG-IgA) - is over 98% accurate if you’re still eating gluten. But if you’ve already gone gluten-free, the test can be falsely negative. That’s why diagnosis requires eating gluten for at least 6 weeks before testing.
And here’s a hard truth: 30% of people diagnosed with celiac disease still have symptoms even after going gluten-free. Why? Cross-contamination, hidden gluten, or other triggers like gut infections or stress. The disease isn’t always as simple as “no gluten = no symptoms.”
The Only Treatment: A Strict Gluten-Free Diet
There’s no pill, no shot, no cure. The only proven treatment is removing all gluten from your diet - permanently. That means avoiding wheat, barley, rye, and anything made from them. But it’s not just about bread. Gluten hides in soy sauce, salad dressings, medications, vitamins, lip balm, and even Play-Doh.
The legal limit for a product to be labeled “gluten-free” is 20 parts per million (ppm) in the U.S. and Europe. That’s tiny - like one drop of water in a full bathtub. But for someone with celiac disease, even that tiny amount can cause damage over time. Studies show that eating just 50 mg of gluten a day (about 1/8 teaspoon of flour) can trigger inflammation and prevent healing.
Getting started means a full pantry reset. You’ll need to replace:
- Flours (swap wheat for rice, quinoa, buckwheat, or certified gluten-free oats)
- Condiments (check labels for malt vinegar, hydrolyzed vegetable protein)
- Snacks (many chips and granola bars contain wheat starch)
- Cooking tools (dedicated toaster, cutting boards, and utensils reduce cross-contamination risk by 85%)
The average cost of switching to gluten-free is $350-$500 upfront. And it’s not cheap to stay that way - gluten-free products cost about 242% more than regular ones, according to Consumer Reports. But the payoff? 89% of people report major symptom improvement within six months.

Hidden Gluten Sources and Everyday Traps
Most people know to avoid pasta and beer. The real trouble spots are the invisible ones:
- Medications: Only 37% of prescription drugs list gluten content. Always ask your pharmacist - even if the pill says “gluten-free” on the box, the filler might not be.
- Restaurant food: 67% of celiac patients report cross-contamination in restaurants. Shared fryers, grills, and toasters are major culprits. Always ask: “Do you have a dedicated gluten-free prep area?”
- Processed foods: Modified food starch, dextrin, maltodextrin - these sound harmless but can come from wheat. Only certified gluten-free versions are safe.
- Supplements: Many probiotics, vitamins, and protein powders use wheat-derived fillers. Look for “certified gluten-free” on the label.
Smart tools help. Apps like Find Me Gluten Free (rated 4.7 stars by 185,000 users) crowdsource restaurant safety ratings. Carrying emergency gluten-free snacks - like nuts, fruit, or certified bars - prevents desperate meals when options are limited.
Long-Term Health and Nutrient Deficiencies
Damage to the small intestine doesn’t just cause bloating or diarrhea. It steals nutrients. By the time most people are diagnosed, they’re already deficient in:
- Iron: Affects 33% of celiac patients - leads to fatigue and anemia
- Vitamin D: Found in 47% - impacts bone health and immunity
- B12 and folate: Needed for nerve function and red blood cell production
- Copper and zinc: Often low due to malabsorption
After diagnosis, most people need supplements for 6-12 months while their gut heals. Regular blood tests are critical. One patient on Reddit shared: “After five years of being gluten-free, my endoscopy showed complete healing - but I still take vitamin D and iron because my body never fully caught up.”

What’s on the Horizon: New Treatments Beyond Diet
While the gluten-free diet works, it’s exhausting. That’s why researchers are racing to develop alternatives. Three therapies are in late-stage trials:
- Nexvax2: A vaccine-like treatment that desensitizes T-cells to gluten. Phase 2 results showed a 42% drop in symptoms.
- Latiglutenase: An enzyme pill that breaks down gluten before it triggers a reaction. In trials, it reduced symptoms by 37%.
- TAK-101: A nanoparticle therapy that reprograms the immune system to tolerate gluten. Early results showed 63% less intestinal damage.
These aren’t cures - yet. But they could one day allow people to eat gluten occasionally without damage. For now, they’re only for those who struggle with the diet or have ongoing symptoms despite strict avoidance.
Researchers are also testing devices that can detect gluten in food at 5 ppm levels - far more sensitive than current lab tests. And studies into the gut microbiome suggest that people with celiac disease have different gut bacteria, which might one day be corrected with targeted probiotics.
Living with Celiac: Real-Life Challenges
It’s not just about food. The emotional toll is real. 58% of people say their diet has damaged their social life. Birthdays, holidays, work lunches - every meal becomes a risk assessment. One young adult wrote: “I turned down a trip to Italy because I was terrified of getting sick. I missed out on the food I’d dreamed of for years.”
Diagnosis delays are still common. The average time from first symptom to diagnosis is 6.7 years. Many are misdiagnosed with IBS, anxiety, or chronic fatigue. If you’ve had unexplained digestive issues, fatigue, or nutrient deficiencies for months or years, ask your doctor for a celiac blood test - while still eating gluten.
And yes, healing is possible. With strict avoidance, most people see their villi regenerate within 6-18 months. Children often heal faster than adults. But it takes discipline. One patient said: “I used to think gluten-free was a trend. Now I know it’s my lifeline.”
Can you outgrow celiac disease?
No. Celiac disease is a lifelong genetic condition. Even if symptoms disappear, the immune system still reacts to gluten. Stopping the gluten-free diet will cause damage to return - often more severely than before.
Are oats safe for people with celiac disease?
Pure, uncontaminated oats are generally safe for most people with celiac disease. But most commercial oats are processed in facilities that also handle wheat, barley, or rye. Only choose oats labeled “certified gluten-free.” Even then, some people react to avenin, a protein in oats that’s similar to gluten. Start with small amounts and monitor symptoms.
Can celiac disease cause other autoimmune diseases?
Yes. People with celiac disease have a higher risk of developing other autoimmune conditions like type 1 diabetes, thyroid disease (Hashimoto’s), and autoimmune liver disease. This is because the same genetic factors that predispose someone to celiac also increase vulnerability to other immune system misfires.
What should I do if I accidentally eat gluten?
There’s no antidote. Symptoms can appear within hours or take up to three days. Drink water, rest, and avoid more gluten. Most people recover in a few days, but the intestinal damage takes weeks to heal. Keep a food log to identify the source and prevent future exposure. If symptoms are severe - vomiting, intense pain, or dehydration - contact your doctor.
Is there a blood test to confirm celiac disease?
Yes. The tTG-IgA test is the most accurate, with 98% sensitivity and 95% specificity. But it only works if you’re eating gluten. If the test is positive, a biopsy of the small intestine is needed to confirm damage. Genetic testing for HLA-DQ2/DQ8 can rule out celiac disease - if you don’t have the genes, you won’t develop it.
If you’ve been told your symptoms are “just stress” or “IBS,” push for a celiac test. Early diagnosis prevents long-term damage - from osteoporosis to intestinal cancer. And while the diet is tough, it’s the one thing that gives you back your health. The science is clear: no gluten, no attack. No attack, no damage. And that’s the foundation of every recovery.




Elen Pihlap
7 January 2026 - 17:54 PM
I just ate a bagel this morning and now I’m terrified I’m going to die. My stomach’s been weird for weeks. Is this it? Am I dying? I can’t even look at bread anymore.
Rachel Steward
8 January 2026 - 03:12 AM
Let’s be real - the entire gluten-free industry is a capitalist scam built on fear and pseudoscience. The real issue isn’t gluten, it’s industrialized food systems that strip nutrients and overload our microbiomes with emulsifiers and preservatives. Celiac is real, but the panic? Manufactured. You don’t need to avoid wheat - you need to stop eating processed crap. The body wasn’t designed for Wonder Bread and soy sauce from a factory that uses wheat starch as a filler. That’s the problem, not evolution.
Aparna karwande
8 January 2026 - 16:51 PM
How dare you call this a ‘diet’? This isn’t some trendy keto phase - it’s a war against your own body, and you’re lucky if you survive it. I’ve seen people collapse from nutrient loss, their bones turning to dust, their hair falling out in clumps. And now some guy in Ohio thinks he can ‘tolerate small amounts’? You’re not special. You’re not immune. You’re just ignorant. If you have celiac, you don’t get to pick and choose. One crumb, one fryer, one soy sauce bottle - and you’re back in hell. Stop romanticizing your ‘gluten sensitivity.’ It’s not a lifestyle. It’s a sentence.
Paul Mason
9 January 2026 - 08:42 AM
My mate in London got diagnosed last year after 8 years of being told it was ‘stress.’ He cried when he finally ate a proper pint of beer again - not gluten-free, the real stuff. Said it tasted like childhood. Anyway, the real nightmare? Trying to find gluten-free curry sauce. No one knows what’s in it. I just stick to rice and chutney now. Simple. Safe. Happy.
Alex Danner
10 January 2026 - 10:09 AM
For anyone just diagnosed: get your vitamin D, iron, B12, and zinc levels checked ASAP. Most people don’t realize how deep the deficiency goes. I was anemic, had nerve tingling, and thought it was ‘just aging.’ Turned out my villi were flat as pancakes. Took 14 months to heal. Took 2 years to feel normal. Supplements helped, but consistency mattered more. And yes - dedicated toaster. No exceptions. Even if your roommate says ‘it’s fine.’ It’s not.
Kyle King
12 January 2026 - 04:44 AM
Gluten is a bioweapon. Big Ag and the FDA are in cahoots. They know wheat triggers autoimmunity but they keep pushing it because pharma makes billions off the side effects. The ‘20 ppm’ rule? A joke. They let poison in so you’ll keep buying ‘gluten-free’ overpriced bread. And don’t get me started on the ‘certified gluten-free’ label - it’s a marketing gimmick. The real cure? Stop eating anything that comes in a box. Eat meat, veggies, and potatoes. That’s it. The rest is control.
Mina Murray
13 January 2026 - 04:01 AM
Why is no one talking about the glyphosate? It’s sprayed on wheat before harvest. That’s what’s actually triggering the immune response, not gluten. The ‘gluten-free’ products are still sprayed with it. They just swap the wheat for corn or rice - same chemical load. You’re still poisoned. And the ‘tTG-IgA test’? It’s designed to miss early-stage damage. They want you to wait until your intestines are shredded before they admit you’re sick. That’s not medicine. That’s negligence.
steve rumsford
14 January 2026 - 05:37 AM
so i tried gluten free for a week and my stomach felt like a balloon that got popped. like, i was fine before. now i’m eating quinoa and feeling like i swallowed a rock. maybe i’m just allergic to healthy food. also why is everything so expensive??
Sai Ganesh
16 January 2026 - 04:11 AM
In India, we’ve eaten wheat for centuries without this crisis. But we didn’t have industrial flour, preservatives, or hybridized wheat strains. Traditional methods - stone grinding, sour fermentation - made wheat digestible. Today’s bread? It’s not food. It’s a chemical product. The solution isn’t to abandon wheat - it’s to return to how our ancestors prepared it. Rotis made from whole grain, fermented dough, slow-risen. That’s not gluten-free. That’s gluten-respectful.
Kamlesh Chauhan
17 January 2026 - 00:46 AM
gluten is fine its the stress and the dairy and the sugar that makes you sick stop blaming the bread you lazy bums why dont you just go outside and run for once
Anthony Capunong
18 January 2026 - 21:02 PM
People like you think celiac is just a ‘Western problem.’ But in rural India, where people eat chapati three times a day, the rates of autoimmune disease are skyrocketing. Why? Because they’re eating the same industrial wheat we are. The same pesticides. The same refined flour. This isn’t about culture. It’s about toxins. And if you think your grandma’s roti is safe, check where the wheat was grown. It’s not 1950 anymore.
Jessie Ann Lambrecht
19 January 2026 - 09:28 AM
Healing is possible. I was diagnosed at 22 - couldn’t walk without fatigue, had mouth sores every week. Now, five years later, I hike mountains, eat at restaurants, and even bake my own gluten-free sourdough. It’s not easy. But you’re not broken. Your body just needs time and care. Start with whole foods. Get a blood test. Find a support group. You’re not alone. And yes - you can still have joy. It just looks different now. And that’s okay.