Parkinson's Disease: What You Need to Know Right Now
If you or someone you love has been diagnosed with Parkinson's, the first question is usually "What now?" The short answer: it's a condition that affects movement, but it doesn't have to control your life. In this guide you'll get straight‑to‑the‑point info on common signs, everyday tricks, and the medicines most people rely on.
Typical Signs You Might Notice
The early clues are often subtle. A tremor that shows up when you're relaxed, stiffness in your arms or legs, and slower movements are the trio many describe. Balance problems and a shuffling walk can appear later, but not everyone gets all three.
Beyond movement, some folks feel mood changes—like feeling down or anxious—without a clear reason. Sleep can get interrupted too, with vivid dreams or sudden leg jerks at night. Spotting these signs early helps you and your doctor plan better.
Treatment Options That Actually Help
Medication is the backbone of Parkinson's care. The most common starter is levodopa, which the brain turns into dopamine to smooth out movement. It often comes paired with carbidopa to reduce side effects like nausea.
If levodopa isn't enough or causes unwanted ups and downs, doctors might add dopamine agonists such as pramipexole or ropinirole. These mimic dopamine but work in a slightly different way. For some, MAO‑B inhibitors (like rasagiline) help preserve the dopamine you already have.
Non‑drug options are just as important. Regular exercise—think brisk walking, cycling, or yoga—keeps muscles flexible and can lessen tremor intensity. Speech therapy helps with voice changes, while occupational therapy teaches smart ways to handle daily tasks without extra strain.
Keeping a symptom diary makes appointments more productive. Write down when you notice shakiness, how long it lasts, and what you ate or did before. This data lets your doctor fine‑tune dosages and spot patterns.
Finally, stay updated on research. New treatments like gene therapy and focused ultrasound are moving through clinical trials and could become options soon. Joining a local Parkinson's support group gives you access to the latest news and a community that gets what you're going through.
Bottom line: Parkinson's disease is manageable with the right mix of meds, movement, and mental health tools. Start by talking openly with your doctor about symptoms, ask about medication timing, and add simple daily habits like stretching or a short walk. Small steps add up to bigger improvements in quality of life.
Understanding the Stages of Parkinson's Disease Progression
Alright folks, let's dive into this rollercoaster we call Parkinson's disease progression. It's like the stages of making a sandwich, but instead of lunch meat and mustard, we've got symptoms and treatments. First off, we have Stage 1, where symptoms are as mild as a baby's burp and mostly on one side of the body. Moving onto Stage 2, things get a bit more exciting, like adding pickles to your sandwich, where symptoms spread to both sides. By the time we hit Stage 3, balance becomes the main issue, and who hasn't had a sandwich fall apart, right? Stage 4 and 5, the final rounds, are where mobility becomes a challenge, like trying to eat a sandwich in a bouncing car. But hey, with the right care and treatment, we can make this ride as smooth as possible. So, let's buckle up and face Parkinson's with a smile!
Read More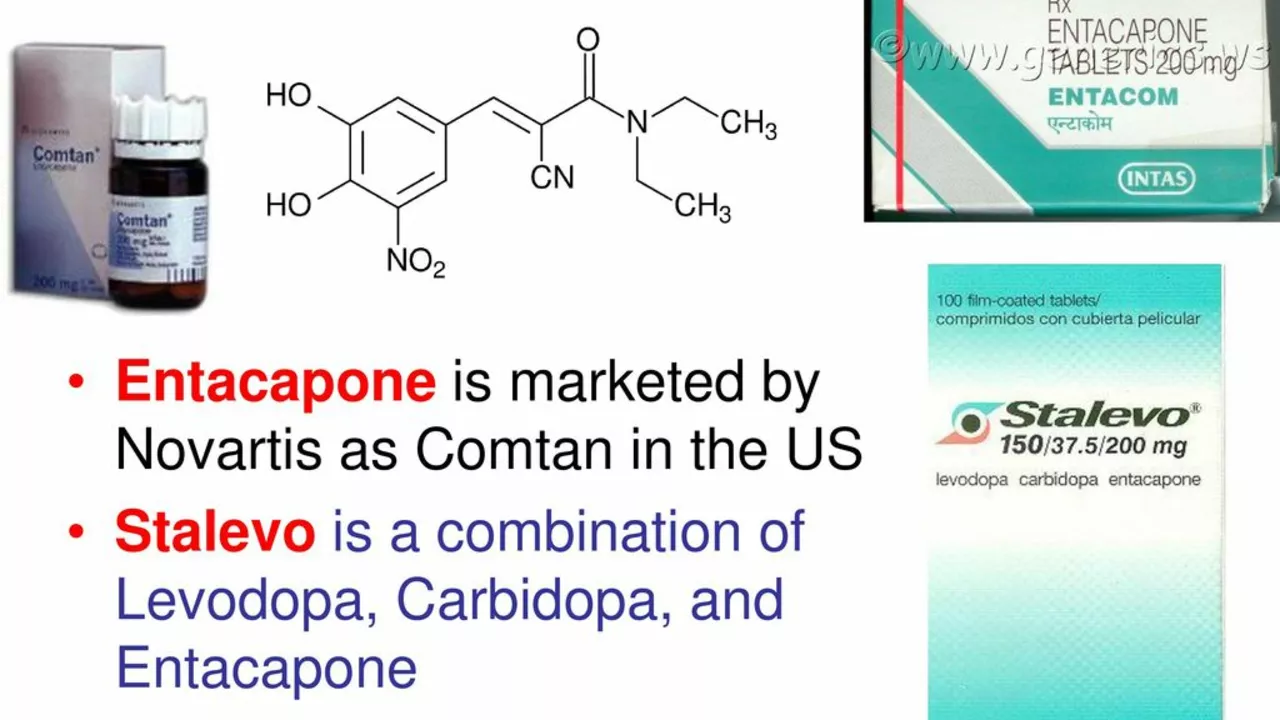
Carbidopa-Levodopa and Parkinson's Disease: Dispelling Common Myths and Misconceptions
Alright folks, buckle up because we're going on a myth-busting ride about Carbidopa-Levodopa and Parkinson's disease! Contrary to popular belief, Carbidopa-Levodopa, the dynamic duo of Parkinson's medication, isn't the big, bad wolf some make it out to be. In fact, it's not even habit-forming or addictive! Can you believe it? Plus, taking this medication early on in your diagnosis doesn't mean you're doomed to exhaust its benefits prematurely. And, the cherry on top is - it doesn't cause damage to your liver or kidneys. So, let's park those misconceptions and embrace the facts about this super combo of drugs!
Read More