Generic Drug Approval: How the FDA Ensures Safe, Affordable Medicines
When you pick up a generic drug, a medication that contains the same active ingredient as a brand-name drug but is sold under its chemical name. Also known as non-branded medication, it works the same way, costs far less, and is held to the same standards—thanks to the FDA generic approval, the official process the U.S. Food and Drug Administration uses to certify that generic drugs are safe and effective.
The system that makes this possible is the Hatch-Waxman Act, a 1984 law that balanced innovation with affordability by letting generic manufacturers skip expensive clinical trials if they prove their drug is bioequivalent to the original. That’s where bioequivalence, the scientific proof that a generic drug delivers the same amount of active ingredient into the bloodstream at the same rate as the brand-name version comes in. It’s not guesswork. It’s lab tests, blood samples, and strict thresholds: the generic must deliver between 80% and 125% of the brand’s absorption. If it passes, it gets approved under the ANDA pathway, the Abbreviated New Drug Application process that cuts years off development time and saves patients billions.
People still worry: "Is it really the same?" Yes. The FDA doesn’t approve generics based on price—they approve them based on science. A 2019 analysis of over 1,000 generic drugs found no meaningful difference in effectiveness or safety compared to brand names. Even the inactive ingredients—fillers, dyes, coatings—are reviewed. If a generic has a different coating that changes how fast it dissolves, it’s rejected. No exceptions.
What you’re getting isn’t a cheaper copy. It’s a legally identical medicine, made under the same quality controls, in the same kind of factories—even sometimes the same ones that make the brand-name version. The only real difference? The price tag. Generics cost up to 85% less because manufacturers don’t have to pay for marketing, patent lawsuits, or years of clinical trials. That’s not cutting corners. That’s smart policy.
And it’s not just about saving money. It’s about access. Millions of people rely on generics to afford blood pressure pills, diabetes meds, antibiotics, and antidepressants. Without the generic drug approval system, many wouldn’t get treated at all. This isn’t theoretical. It’s daily life for people managing chronic conditions on fixed incomes.
What you’ll find below is a collection of real, practical posts that dig into the details: how the FDA checks for bioequivalence, what the Hatch-Waxman Act really means for your prescription, why some generics still get flagged, and how supply chains keep counterfeit drugs out of your medicine cabinet. No marketing fluff. Just the facts you need to understand what’s in your bottle—and why it’s safe.
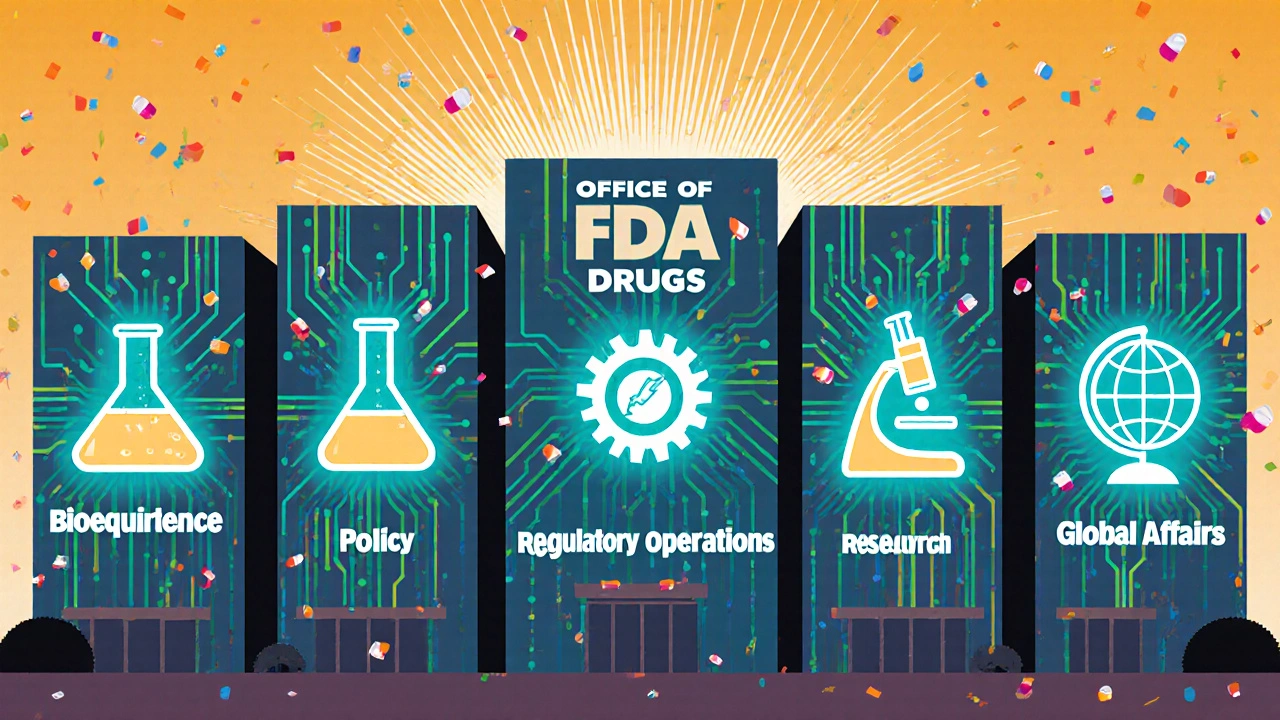
FDA Office of Generic Drugs: Role, Responsibilities, and Structure Explained
The FDA's Office of Generic Drugs ensures safe, affordable generic medications reach patients by reviewing applications, enforcing bioequivalence standards, and managing regulatory policy under GDUFA and the Hatch-Waxman Act.
Read More