Contrast Sensitivity: What It Is and Why It Matters
When working with contrast sensitivity, the eye’s ability to distinguish subtle differences in light and dark. Also known as luminance discrimination, it determines how well you see edges, textures, and low‑contrast objects—think of reading a road sign on a foggy morning or spotting a phone screen in dim light. Most people mix it up with visual acuity, the sharpness of detail you can resolve at high contrast. While a 20/20 chart tests acuity, contrast sensitivity tests how well you perceive shades that aren’t starkly black‑and‑white. The two metrics together give a fuller picture of visual performance.
How Contrast Sensitivity Connects to Common Eye Conditions
One of the biggest links is with glaucoma, a progressive optic nerve disease that often sneaks up without obvious vision loss. Early‑stage glaucoma tends to erode contrast sensitivity before visual acuity drops, so a drop in luminance discrimination can be an early warning sign. Similarly, an eye injury, any trauma that damages cornea, lens, or retina can blunt contrast perception, making everyday tasks feel fuzzy even if you can still read a eye chart. Knowing this, eye‑care professionals regularly include contrast tests when evaluating patients with suspected glaucoma or post‑trauma recovery.
Contrast sensitivity isn’t just a clinical curiosity; it drives real‑world safety. Drivers with reduced contrast perception may struggle to see pedestrians at dusk, and older adults often miss low‑contrast hazards on stairs, leading to falls. Studies have shown that people with poor contrast scores are more likely to report difficulties with night driving, reading magazines, and recognizing faces in soft lighting. That’s why optometrists recommend regular testing, especially for those over 60 or anyone diagnosed with ocular disease.
Testing methods have come a long way. The classic Pelli‑Robson chart presents rows of letters that fade from black to gray, providing a quick snapshot of contrast capability. Newer digital tools use sinusoidal gratings that vary spatial frequency and contrast, offering finer detail about which visual pathways are affected. These tests help differentiate whether a problem stems from the retina, the optic nerve, or higher‑order brain processing.
When you understand your contrast sensitivity, you can make smarter choices about lighting and screen settings. Increasing ambient light, using high‑contrast fonts, and avoiding glare can boost performance instantly. For gamers or graphic designers, tweaking monitor contrast levels can reduce eye strain and improve detail detection. Even simple habits like positioning a TV away from windows or using anti‑glare filters can make a noticeable difference.
Beyond everyday adjustments, several medical interventions aim to preserve or restore contrast function. Eye drops that lower intra‑ocular pressure in glaucoma patients have been shown to stabilize contrast scores. Nutritional supplements rich in omega‑3 fatty acids and lutein support retinal health, which can indirectly benefit contrast perception. For severe cases, low‑vision rehabilitation programs teach patients to use assistive devices—like magnifiers with high‑contrast illumination—to compensate for losses.
All this shows that contrast sensitivity sits at the crossroads of eye health, safety, and quality of life. In the collection below you’ll find articles that explore related topics such as diet’s impact on fungal infections, deep‑brain stimulation for Parkinson’s, and practical guides for buying cheap generic medications online. While not all pieces focus directly on vision, they share a common thread: helping you understand how body systems, treatments, and lifestyle choices intersect with everyday well‑being. Dive in to see how these insights might complement your own eye‑care plan.
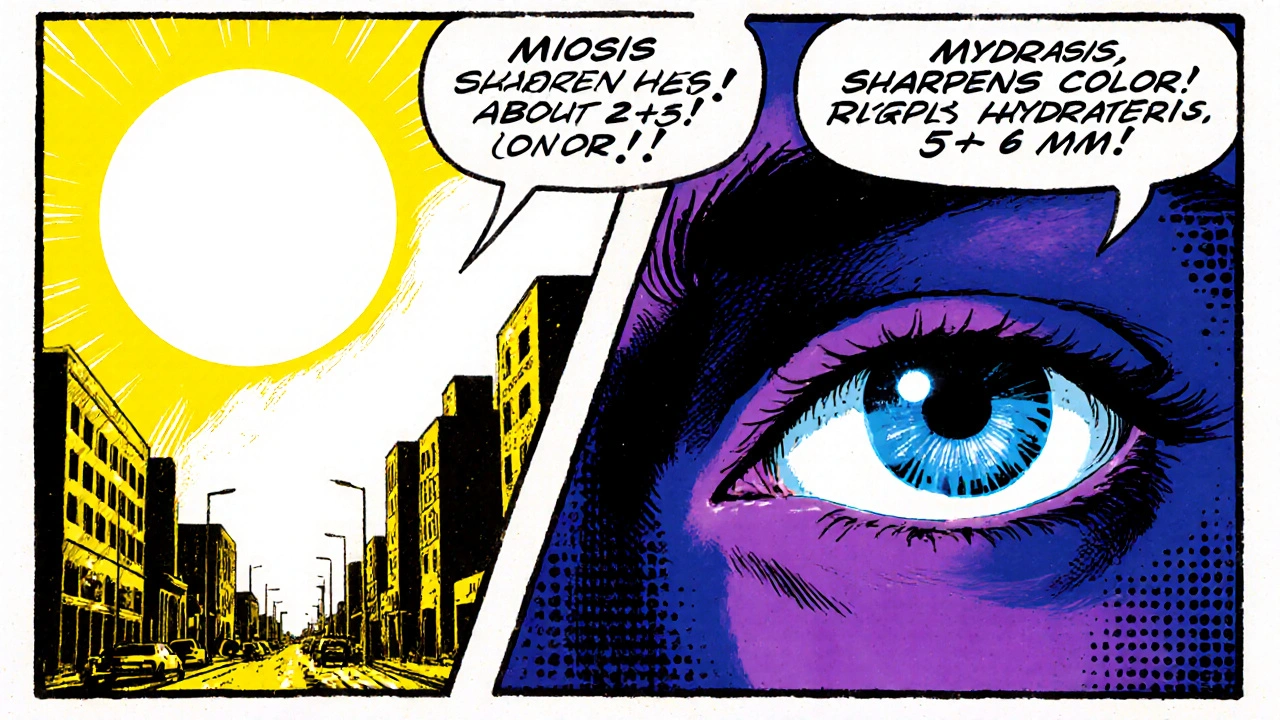
How Miosis Affects Color Perception and Contrast Sensitivity
Explore how pupil constriction (miosis) influences color perception and contrast sensitivity, with tips, comparisons, and the latest research insights.
Read More