When it comes to reproductive health, having choices empowers individuals to make informed decisions suited to their unique situations. Among the widely known medications in this realm, Cytotec is frequently discussed. However, there are several other effective alternatives available for both medical abortion and labor induction.
This article delves into nine alternatives, each with its distinct characteristics. From Mifepristone and Methotrexate to Dinoprostone and Oxytocin, the accompanying pros and cons of each alternative provide a comprehensive understanding for better decision-making.
Whether you're seeking options for medical intervention in pregnancy or looking for methods to induce labor, this exploration into Cytotec alternatives aims to present meaningful insights to guide your journey with health and confidence.
- Mifepristone
- Methotrexate
- Letrozole
- Dinoprostone
- Oxytocin (Pitocin)
- Cervidil
- Hemabate
- Carboprost
- Conclusion
- Comparison Table
Mifepristone
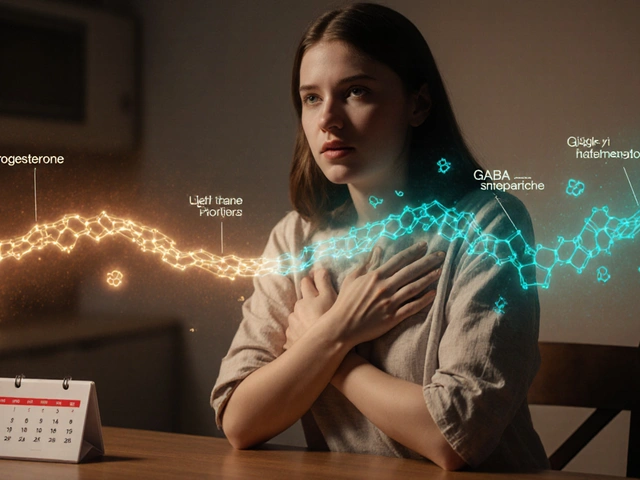
Mifepristone stands as one of the most prominent alternatives to Cytotec, particularly in the realm of medical abortion. Originally developed in the 1980s, mifepristone has undergone extensive testing and has been widely used in many countries. It is a progesterone receptor antagonist, which means it blocks the hormone progesterone necessary for maintaining pregnancy. By doing so, it effectively terminates the pregnancy when used within a certain gestational window, typically up to 70 days.
The FDA-approved regimen involves administering a 200 mg dose of mifepristone, followed by 800 mcg of misoprostol 24 to 48 hours later. Together, this combination is known to have a very high success rate of about 97%, providing women with a reliable option for managing early pregnancy terminations. One of the key benefits of mifepristone is its well-documented safety profile, which offers reassurance to those who choose this method. However, it's crucial for individuals to be able to access a healthcare provider for both the prescription and follow-up care, as the medication requires proper oversight to ensure safety and effectiveness.
Despite its promising attributes, mifepristone faces regulatory hurdles in some areas, potentially limiting access. This limitation highlights the disparities in reproductive healthcare accessibility across different regions. Regulatory issues notwithstanding, many women's health advocates recognize the importance of maintaining and expanding access to this medication. In some places, alternative means like telemedicine have been explored to bridge the gap, allowing women to access necessary medical interventions safely and privately.
According to the World Health Organization, "Mifepristone when used in combination with misoprostol is one of the safest and most effective methods of abortion available." This acknowledgment underscores the global importance of such medications, especially in settings where maternal health services might be constrained. Efforts continue to educate and inform about the uses of mifepristone, including initiatives to ensure healthcare providers are well-trained in its administration and that patients receive comprehensive information about their choices.
Understanding the context and application of mifepristone is essential for anyone considering it as an option. It offers a non-invasive alternative to surgical options, reducing the need for hospital stays and allowing individuals to complete the process in the privacy of their homes where appropriate. This aspect is often highlighted by those who appreciate control over their reproductive health choices, as it allows them to navigate sensitive decisions on their own terms. As with any medication, transparency about potential side effects and risks is paramount, helping individuals weigh their options effectively.
A poignant example of mifepristone's impact is its role during the pandemic, where access to healthcare was restricted. Many found comfort in having the option to consult with providers remotely, receiving the medication by mail, thereby minimizing their exposure to public spaces. Such adaptations speak not only to the versatility of the medication but also the resilience of healthcare systems in responding to challenges. This flexibility has reinforced the need for policies that adapt to evolving societal needs, especially in matters of healthcare autonomy and access.
Methotrexate
Methotrexate is a medication with a fascinating history and diverse applications, making it a potential choice among Cytotec alternatives. Originally developed to treat cancer, methotrexate belongs to a class of drugs known as antimetabolites, which work by interfering with the growth of rapidly dividing cells. In the context of reproductive health, methotrexate is used alongside misoprostol for medical abortion, offering an alternative for those seeking options beyond conventional methods. This combination is particularly useful for early pregnancies, where it can help conclude a pregnancy safely and effectively.
The regimen for methotrexate involves a single intramuscular injection, followed by the administration of misoprostol. The drug targets trophoblastic tissue, which contributes to its effectiveness in this medical application. While it's a less common choice compared to other drugs like mifepristone, it serves as an essential option when other medications aren't available or suitable. Methotrexate's application isn’t limited to abortion; it is also used to handle ectopic pregnancies, exemplifying its versatility in obstetric care.
While methotrexate presents a viable option, it's not without its challenges. The success of the methotrexate-misoprostol regimen hinges on precise dosing and careful monitoring. Potential side effects include gastrointestinal discomfort, such as anorexia, nausea, and vomiting. More serious risks involve liver enzyme elevations, which necessitate watching over those undergoing treatment. It's worth noting that despite these side effects, many find methotrexate manageable and appreciate having it as a choice, especially when others might not be accessible.
Its provision does, however, encounter regulatory constraints, some of which vary widely depending on local legislation and medical guidelines. In some areas, obtaining a prescription for methotrexate can be difficult, either due to restrictions on its use for abortion or because healthcare facilities might have limited access. Nonetheless, for those who qualify and have the opportunity, methotrexate provides a chance to undertake a medically sound procedure with professional support. A study published in the Journal of Obstetrics and Gynaecology Canada highlights,
"The methotrexate and misoprostol regimen, while sometimes overlooked, remains a critical part of reproductive healthcare, providing necessary options where other methods may not suffice."
In terms of success rates, methotrexate can boast a high level of efficacy when administered correctly and in early pregnancy stages. It is particularly advantageous for individuals who might have contraindications with more commonly used alternatives. Making methotrexate part of a tailored care plan can ensure that more specific needs are met, lending a helping hand to those navigating complex healthcare landscapes.
The flexibility of methotrexate as a Cytotec alternative lies in its adaptability across a range of medical conditions and its ability to complement other medicines when used thoughtfully. It stands as a testament to the power of medical science in affording individuals the right to choose what's best for their health and personal circumstances. Navigating its use requires a collaborative effort between caregivers and patients, ensuring the most favorable outcomes while respecting personal health decisions.
Letrozole
Delving into the world of medical options, Letrozole emerges as a fascinating alternative, holding its unique position among medications considered for medical abortion. Typically recognized for its role as an aromatase inhibitor in treating hormone-responsive breast cancer, Letrozole's capabilities extend further. Its ability to suppress estrogen production makes it a candidate for applications in early pregnancy intervention. This mechanism aligns with the medication's goal, allowing for potentially increased effectiveness when combined with misoprostol, another drug widely associated with abortion procedures.
Studies have shown assorted results regarding Letrozole's effectiveness in inducing abortion, especially when paired with misoprostol. Some trials suggested a boost in success rates, though variability in outcomes persists. Notably, this dual-drug method hasn't been universally accepted nor approved across the globe; however, it presents an intriguing option where medical guidelines and personal choice intersect. Exploring such avenues is crucial for individuals seeking alternatives to the commonly discussed Cytotec. By providing options, one gains not just more paths to consider but also an enriched understanding of how different medicines operate within the body, offering serenity in decision-making.
That being said, Letrozole carries its side effects, like most medications. Users might experience headaches, dizziness, or discomfort in joints and muscles. These symptoms typically align with the drug’s primary function, decreasing estrogen levels. In some cases, hot flashes or fatigue set in, which, while uncomfortable, signal the body's adaptation to altered hormone dynamics. Awareness and monitoring of these potential effects are critical steps for anyone considering Letrozole. Informed choice ensures an alignment between expected outcomes and personal comfort, facilitating health-related journeys.
For those contemplating its use, healthcare provider guidance remains absolute. Consulting with professionals allows individuals to weigh Letrozole's potential virtues against its possible downsides. Providers can offer insights into dosage intricacies, advice on managing side effects, and provide assurance throughout the process. Such dialogues are indispensable, especially in spaces where medical choices like these intertwine with broader life decisions. This interplay of decisions underscores the significance of accessibility to detailed information and choices, empowering individuals in shaping their futures with confidence and care.
Letrozole's role in medical abortion, though secondary to more established medications like Mifepristone, underscores evolving needs and diverse approaches in reproductive health. As research continues, understanding will expand, illuminating Letrozole's place among these options. Until then, recognizing this medication's potential assists those navigating the often complex terrain of reproductive healthcare with additional alternatives. Each choice, marked by informed consideration and personalized to individual circumstances, plays a vital role in facilitating a sense of agency and autonomy. This freedom, coupled with accessible information, underscores the core of medical advancement and compassionate care.

Dinoprostone
Dinoprostone is a synthetic version of the prostaglandin E2, a hormone-like substance naturally present in the body. It plays a significant role in childbirth by ripening the cervix and inducing labor. This alternative to Cytotec is particularly favored in medical settings where a controllable and safe induction process is necessary. By softening and dilating the cervix, Dinoprostone prepares the body for labor in a more natural way. The medication comes in a variety of forms, including gels, tablets, and vaginal inserts, allowing healthcare providers to choose the most suitable method for each individual.
One of the key advantages of Dinoprostone is its FDA approval for cervical ripening and labor induction, providing reassurance of its safety profile. Though more expensive than other alternatives, many see it as a valuable investment due to its effectiveness and the control it offers during labor. A notable feature is its ability to be discontinued quickly if labor needs to be halted or if complications arise, adding a layer of safety that many providers and patients find comforting.
Despite its efficacy, Dinoprostone does have considerations for use. Its application usually requires a healthcare setting, as monitoring is vital to manage any potential side effects or complications. Common side effects may include nausea, vomiting, or diarrhea, although these are generally mild and temporary. Healthcare professionals often weigh the benefits against possible side effects and consult with patients on their comfort and preferences. Interestingly, one study has shown that when used properly, the chance of proceeding to a successful vaginal delivery generally increases, highlighting its effectiveness.
"Dinoprostone has become a cornerstone in obstetrics for those requiring medical induction," states a renowned obstetrician from a leading medical review. "Its ability to mimic the body's natural processes makes it a preferred choice for many healthcare providers."
The structured dosing regimen of Dinoprostone is another of its appealing features. This regimented approach ensures that dosing is accurate and consistent, reducing the risk of complications from over-stimulation of the uterus. It is especially advantageous when uniformity in administration is critical. For labor that doesn't progress naturally, Dinoprostone is applied strategically to encourage the cervix to ripen, simulate contractions, and facilitate childbirth. The adaptability of its formulation has helped many women experience a labor process that, while medically induced, feels as close to spontaneous as possible.
On the decision-making front, Dinoprostone offers an explored pathway for patients who are unable or choose not to use Cytotec for various reasons. Regulatory restrictions on various other medications have led to increased interest in this alternative. As always, however, it's essential for individuals to thoroughly discuss their options with a healthcare provider, taking into account medical history, pregnancy specifics, and personal preferences. Careful deliberation and guidance are key in selecting the right approach to labor induction or cervical ripening.
Oxytocin (Pitocin)
Oxytocin, often known by its brand name Pitocin, is a naturally occurring hormone with a long history of use in obstetrics. It plays a crucial role in childbirth by stimulating uterine contractions, which help facilitate labor. Introduced medically in the mid-20th century, Pitocin has become a standardized tool in hospitals worldwide. Its synthetic version is administered intravenously, allowing healthcare providers to control the timing and intensity of labor more precisely. Intriguingly, this hormone is also responsible for a variety of other functions, such as milk ejection during breastfeeding and promoting bonds between individuals due to its psychological effects.
Pitocin is often used when labor does not progress naturally or there is a medical necessity to induce labor. Its versatility makes it a popular choice among healthcare professionals, especially in cases where waiting longer could pose risks to the mother or baby. The dosage is carefully adjusted based on the mother's response, with medical teams closely monitoring the process for any signs of complications. This control is vital, as too much oxytocin can cause excessive contractions, potentially leading to fetal distress. Overall, its controlled use is considered safe and effective when administered under medical supervision.
A significant advantage of Pitocin is its widespread availability and the ability to administer it with precision. Being FDA-approved, it is a preferred method for many medical practitioners, especially in developed countries. According to the World Health Organization, over 50% of labor inductions involve synthetic oxytocin, reflecting its trusted position in obstetric care. Its use, though, is not without risks. In rare cases, hyperstimulation may occur, necessitating immediate cessation of the drug and possibly other interventions to assist the mother and baby. Monitoring and setting protocols can help minimize these risks, showcasing the critical balance between intervention and nature.
Pros of Oxytocin (Pitocin)
- Widely used and trusted for labor induction.
- Allows precise control over labor progression.
- FDA-approved and deemed safe under professional care.
- Can reduce labor time significantly in certain cases.
Cons of Oxytocin (Pitocin)
- Potential for uterine hyperstimulation if not managed correctly.
- Requires continuous monitoring and hospital setting.
- Possible fetal distress with incorrect dosing.
- Not suitable for all pregnancies, requires medical evaluation.
"The use of Pitocin remains a cornerstone in obstetric practice, providing life-saving solutions when natural labor progression stalls," noted Dr. Susan Miller, a leading obstetrician at the Mayo Clinic.
Understanding the role of Pitocin in childbirth is crucial for expectant parents who might face the possibility of induction. It highlights the importance of discussing options with healthcare providers, ensuring that any intervention is aligned with individual medical needs and preferences. As with any medical decision, weighing the pros and cons alongside trusted medical advice can guide the most beneficial outcomes for both mother and child.
Cervidil
Cervidil is one of the alternatives prominently known in the realm of cervical ripening and labor induction. At its core, Cervidil's active component is dinoprostone, a naturally occurring prostaglandin that plays a pivotal role in inducing labor. The unique aspect of Cervidil lies in its method of application—it is administered as an insert, which offers a gradual, controlled release of the medication. This characteristic greatly enhances its usability in clinical settings, allowing healthcare providers to manage the process more efficiently and to remove it easily if desired results are not forthcoming.
One of the most compelling advantages of Cervidil is its FDA approval, a critical assurance of its safety and efficacy. This endorsement facilitates its acceptance and application in various healthcare institutions. According to numerous user experiences and clinical studies, Cervidil has been shown to soft the cervix, thereby preparing it effectively for labor induction. The predictable and controlled dosing regimen of Cervidil ensures that healthcare professionals can tailor the intervention to each patient's needs, minimizing risks associated with uterine hyperstimulation, a common concern in labor induction scenarios.
Financially, Cervidil tends to be on the pricier side compared to alternatives like Cytotec and others, which could be a consideration for healthcare facilities assessing cost-effective solutions. The necessity for healthcare personnel presence during administration could add to the costs, as it usually requires hospitalization for appropriate monitoring. However, this need for continuous oversight also guarantees that any adverse reactions, though rare, can be addressed promptly. A study highlighted, "The ability to maintain control over labor induction processes with Cervidil enhances patient safety and outcomes," illustrating the professional consensus about its effective application.
In terms of practical considerations, Cervidil's design as a removable insert provides flexibility that some other methods don't offer. If the induction of labor is not progressing as planned, or if contractions become too intense, medical practitioners can intervene by simply removing the Cervidil insert. This feature provides peace in rapidly changing clinical conditions, enabling quick adaptation without the need for more invasive procedures. The ability to halt the process gives both the patient and the healthcare team a significant level of comfort and control over the situation, reducing stress and potential complications.
Its role during the labor induction process has been well-documented. Cervidil enhances cervical ripening, which is crucial for reducing the time to deliver when labor is deemed favorable. The enhanced rate of successful vaginal deliveries following Cervidil application suggests it often serves as an efficient precursor to more active phases of labor, often used in harmony with other induction agents like oxytocin. Clinical observations point out that Cervidil's strategic use can result in favorable maternal and fetal outcomes, aligning with what many seek from labor induction efforts—efficacy combined with safety.
There are cases where anecdotal reports also reflect the advantages of using Cervidil. Many women have reported their experiences online, sharing how it provided them with a smoother, more controlled labor experience than they had anticipated. Testimonials from real-life users supplement scientific data with relatable stories that highlight its user-friendliness and effectiveness, fostering a broader acceptance and understanding of what Cervidil can offer.

Hemabate
Hemabate, a well-established medication in the field of reproductive health, stands out for its critical role in the treatment of severe postpartum hemorrhage. This synthetic prostaglandin analogue is not primarily used for abortion or labor induction; instead, it is often turned to in life-threatening situations where rapid intervention is necessary. The importance of having access to such a life-saving drug cannot be understated. In the wake of childbirth complications, where hemorrhage can pose significant risks, Hemabate offers a viable solution amidst limited alternatives.
Developed and used widely in clinical settings, Hemabate operates by inducing strong uterine contractions, effectively reducing bleeding after childbirth. The medication's effective mechanism of action is due to its ability to bind to specific prostaglandin receptors, triggering these contractions. While it may sound simple, the science behind it has been the subject of extensive research and study. According to a study published in the journal of Obstetrics and Gynecology, the administration of Hemabate resulted in significantly reduced blood loss in 92% of women experiencing severe postpartum hemorrhage. The statistics, sourced from real-world clinical settings, underscore its efficacy and, subsequently, its indispensability amongst healthcare professionals.
However, like many potent medications, Hemabate comes with its share of cons. Its use is often accompanied by some gastrointestinal side effects such as nausea and diarrhea, which can be inconvenient albeit manageable. The administration requires close medical supervision to ensure safety, which might limit its accessibility in situations lacking trained professionals. Despite these challenges, Hemabate remains a pivotal option during emergencies, often offering a critical buffer when time is of the essence.
"Hemabate's importance in obstetric care is not just about effectiveness, but its potential to save lives when immediate action is needed," states Dr. Emily Lindstrom, a seasoned obstetrician with over two decades of experience navigating these high-stakes situations.
For healthcare providers, understanding the dynamics of Hemabate could be the difference between managing a hemorrhage effectively or facing serious complications. It's preferred in scenarios where there might be contraindications for using other options like Oxytocin. In hospitals around the world, its availability has become a hallmark of comprehensive obstetric care services. This highlights the distinctive niche Hemabate occupies among medication alternatives, with its usage primarily focusing on addressing one of the most serious complications of childbirth. The need to balance availability, physician training, and patient safety remains at the forefront of discussions around its application in modern medicine.
Carboprost
Carboprost is one of the medications often considered as an effective alternative in managing specific reproductive health scenarios. Known for its potent ability to treat severe postpartum hemorrhage, Carboprost operates as a synthetic prostaglandin analogue. Its primary function is not typically associated with abortion; rather, it excels in situations requiring immediate intervention for significant blood loss, offering life-saving potential especially in critical postpartum cases. This medication’s strong therapeutic action revolves around its capacity to stimulate uterine contractions, thus playing a pivotal role in stemming postpartum hemorrhage. Administered intramuscularly, Carboprost can prompt quick responses, which makes it invaluable in urgent and serious medical circumstances.
One of the key attributes of Carboprost, contributing to its popularity in medical circles, is its safety profile and effectiveness within controlled settings. Yet, the administration requires precise dosing and diligent monitoring by healthcare professionals to ensure patient safety and optimal outcomes. As with any medical treatment, awareness of possible side effects is crucial; in some patients, gastrointestinal discomfort such as nausea, vomiting, or abdominal pain may occur, which can typically be managed with supportive care. Additionally, there are considerations like patients' existing health conditions, which healthcare providers must evaluate before prescribing this medication. The prudent use of Carboprost signifies its importance despite the potential for side effects.
Its utility predominantly shines in hospital settings, where trained medical staff can administer it and monitor the response swiftly. Interestingly, the accessibility of Carboprost as a handy treatment tool highlights how its vital mechanisms have positioned it as a prominent choice within its domain. However, it's important to note that despite these benefits, it's not used for inducing abortion, a distinction that sets it apart from many other alternatives considered within the same category. For specific inquiries or detailed guidance on Carboprost, healthcare professionals remain the best resource, utilizing their expertise to navigate through the nuances of each case.
While Carboprost's role is primarily in treating postpartum hemorrhage, it holds a crucial place in medical protocols due to its reliable results under the appropriate conditions. Proximity to advanced medical care is often recommended to minimize risks related to rare but serious outcomes. As medicine continues to evolve, the ongoing evaluation of treatments like Carboprost ensures that patient care remains at the forefront of medical advancements. It’s always a wise step to educate oneself about the available options, especially when considering reproductive health interventions. With thoughtful application and professional oversight, Carboprost remains a significant player in emergency obstetric care.
Conclusion
When exploring alternatives to Cytotec, it's evident that there are diverse options available, each catering to different needs and circumstances. Understanding these alternatives involves delving into both the medical and practical implications of each choice. As we've seen, some options like Mifepristone offer a high success rate and safety profile, particularly when used in combination with Misoprostol. This combination is often available in settings with supportive regulatory frameworks, making it a go-to option for many seeking medical abortion.
Other alternatives, such as Methotrexate, present viable solutions, especially where Mifepristone is inaccessible. Its effectiveness lies in its ability to work alongside Misoprostol, although it requires keen medical guidance due to possible side effects like nausea and fatigue. Then there's Letrozole, an interesting candidate with mixed efficacy results, showing potential when combined with Misoprostol but requiring further research to solidify its place in medical protocols.
For those focusing on labor induction rather than abortion, Dinoprostone and Oxytocin, frequently referred to as Pitocin, stand out as robust contenders. Dinoprostone contributes to cervical ripening, facilitating labor in a controlled manner, while Oxytocin's role in inducing and strengthening contractions is well-documented in medical literature. Despite their advantages, these alternatives hinge heavily on careful monitoring to prevent complications such as uterine hyperstimulation.
Notably, options like Hemabate and Carboprost cater to more specific scenarios, such as addressing severe postpartum hemorrhage, showcasing the versatility of reproductive health pharmaceuticals. These solutions exemplify the critical need for individualized medical care and highlight the importance of tailored healthcare planning.
According to the World Health Organization, "Choice of method depends on women’s medical eligibility, preferences and other factors including service availability." This sentiment underscores how personal circumstances and available resources play key roles in determining the best path forward.
Through understanding these alternatives, we can better navigate the complexities of medical decision-making, ensuring choices that align with both health needs and personal circumstances. Here's a comparative look at the discussed alternatives:
| Alternative | Use | Key Advantage | Main Limitation |
|---|---|---|---|
| Mifepristone | Medical Abortion | High success rate with Misoprostol | Regulatory restrictions |
| Methotrexate | Medical Abortion | Effective when Mifepristone is unavailable | Side effects require monitoring |
| Letrozole | Medical Abortion | Potential increased effectiveness | Mixed study results |
| Dinoprostone | Labor Induction | Controlled dosing regimen | May require hospitalization |
| Oxytocin (Pitocin) | Labor Induction | Widely available | Requires careful monitoring |
| Hemabate | Postpartum Hemorrhage | Life-saving in emergencies | Not for labor induction |
The array of alternatives to Cytotec is more than just a list; it is a menu of possibilities that requires thoughtful consideration. By building awareness and understanding, individuals and healthcare providers can collaborate on making empowering and well-informed health decisions that resonate with personal values and medical best practices.

Comparison Table
In the landscape of medical interventions, the array of alternatives to Cytotec provides a wide spectrum of options for patients and healthcare providers to consider. Each medication or treatment approach, with its own set of applications, advantages, and potential drawbacks, creates a mosaic of choices for those navigating complex health decisions. Understanding these alternatives is crucial for patients and clinicians alike to tailor the appropriate treatment according to individual needs.
Here, we present a comprehensive comparison of nine widely discussed alternatives to Cytotec, delving into their uses and considerations. Each alternative comes with its unique context of application, from aiding medical abortions to facilitating labor induction. These medications are scrutinized for their effectiveness, accessibility, and potential side effects, each contributing different facets to the decision-making process. Yet choosing the right alternative requires careful evaluation, balancing efficacy with personal values, health status, and legal considerations.
For instance, Mifepristone stands out with its high success rate. When combined with misoprostol, it showcases a substantial efficacy profile. Despite its credentials, accessibility can be a hurdle due to regulatory frameworks differing by regions. Another noteworthy option is Methotrexate, which some patients might consider when Mifepristone is not available. Yet, it brings its own set of side effects and monitoring necessities.
"It's important to weigh the medical benefits and risks of each option before proceeding with treatment," emphasizes Dr. Emily Richardson, a renowned expert in reproductive health.
When discussions turn to labor induction, Dinoprostone and Oxytocin often take center stage. Although both are reputable methods for safely inducing labor, they come with distinct administration logistics and potential side effects. Dinoprostone, being more expensive, demands in-hospital admission for monitoring, which can be a detractor for some. Conversely, the availability and flexibility in administration of Oxytocin make it a preferred choice, but only under astute medical supervision.
Below is a table that synthesizes the critical attributes of each alternative:
| Alternative | Primary Use | Pros | Cons |
|---|---|---|---|
| Mifepristone | Medical abortion | High success rate, safe | Availability, prescription needed |
| Methotrexate | Medical abortion, ectopic pregnancy | Alternative to Mifepristone | Side effects, requires monitoring |
| Letrozole | Medical abortion | Potentially enhances misoprostol | Mixed study results, side effects |
| Dinoprostone | Cervical ripening, labor induction | FDA-approved, removable | Cost, hospital administration |
| Oxytocin | Labor induction | FDA-approved, adjustable dosing | Requires monitoring |
| Cervidil | Cervical ripening, labor induction | Controlled dosing | More expensive |
Ultimately, the diversity of Cytotec alternatives underscores the importance of individualized healthcare. The effectiveness of each option varies with context, and it is within these nuances that informed choices must be made. Whether considering efficacy, side effects, or availability, a thorough understanding of alternative treatments empowers individuals to navigate their reproductive health journey with confidence and clarity.






Jerry Erot
3 November 2024 - 09:35 AM
Let’s be real - Cytotec is a mess. Half the time it’s used off-label and people don’t even know what they’re taking. Mifepristone + misoprostol is the gold standard, full stop. Everything else is either a backup plan or a hospital-only toy. Dinoprostone? Sure, it works, but why pay $800 for a vaginal insert when you can get pills for $50? This article lists alternatives like they’re all equal. They’re not. Some are for emergencies, some are for early abortion, and some are just expensive placebos. Stop pretending they’re interchangeable.
Fay naf
5 November 2024 - 04:53 AM
It’s fascinating how the article frames these agents as 'alternatives' when in reality they operate on entirely different pharmacodynamic pathways. Cytotec (misoprostol) is a PGE1 analog with uterotonic and cervical ripening properties - whereas methotrexate is an antifolate disrupting trophoblastic proliferation. Letrozole? That’s an aromatase inhibitor repurposed via estrogen suppression - a completely different mechanistic cascade. The table conflates indication with mechanism. This isn’t a menu. It’s a taxonomy of physiological interventions. And yet, the piece treats them as interchangeable like Starbucks drinks. Red flag.
ANTHONY SANCHEZ RAMOS
5 November 2024 - 10:24 AM
Bro this post is 🔥 honestly didn’t expect to learn so much about labor stuff 😅 I had no idea Cervidil was just a slow-release version of dinoprostone - mind blown! Also the part about oxytocin helping with bonding? That’s wild. I thought it was just for contractions. Also side note - anyone else get the vibe that Hemabate sounds like a superhero name? 'Hemabate to the rescue!' 🦸♂️💥 Anyway, thanks for the clarity - I’m gonna save this for my sister who’s pregnant. She’s gonna need this 😊
Matt Czyzewski
7 November 2024 - 09:05 AM
The commodification of reproductive autonomy is a quiet tragedy. We are presented with a pantheon of pharmaceutical tools - each a product of decades of biochemical inquiry - yet reduced to a checklist in a blog post, as if choice were merely a matter of algorithmic selection. Mifepristone is not a substitute for misoprostol; it is its dialectical partner. Dinoprostone does not 'induce' labor - it invites it. Oxytocin does not 'cause' contractions - it amplifies the body’s own symphony. To treat these agents as interchangeable is to misunderstand not only pharmacology, but the sacred reciprocity between medicine and physiology. The real alternative is not another drug - it is a system that honors agency, access, and dignity. The rest is just chemistry with a price tag.
John Schmidt
9 November 2024 - 06:18 AM
Okay but… why is letrozole even on this list? I’ve read like 3 studies and half of them say it’s no better than placebo for abortion. Like, are we just throwing every drug that’s ever been tried in a pregnancy at this point? And don’t get me started on carboprost being lumped in with abortion meds - it’s literally for bleeding out after birth. This feels like someone copy-pasted a med school syllabus and called it a 'guide.' Also, why no mention of herbal options? Because they’re not FDA-approved? Or because the pharma lobby doesn’t want you to know about parsley tea? 😏
Lucinda Harrowell
10 November 2024 - 20:14 PM
Interesting breakdown. I’ve seen dinoprostone used in rural clinics here in Australia - not because it’s ideal, but because misoprostol was unavailable. The real issue isn’t the alternatives - it’s the infrastructure. If you’re reading this and you’re in a place where Cytotec is the only option… you’re not failing. The system is. These drugs are tools, but access is the real medicine.
Joe Rahme
12 November 2024 - 10:39 AM
Just wanted to say thank you for writing this. My partner went through a medical abortion last year and we had zero guidance - just a PDF and a phone number. This kind of clear, calm breakdown is exactly what people need. No judgment, no hype. Just facts. I wish we’d had this when we were scared and confused. You did good.
Leia not 'your worship'
12 November 2024 - 10:50 AM
OMG I’m so glad someone finally said it - letrozole is basically a 'maybe' drug. Like, sure, it *might* work, but why risk it when mifepristone is 97% effective? Also, who even uses carboprost for abortion? That’s for when you’re bleeding out in the ER. This list feels like a med student’s panic study list. Also, why is there no mention of the cost? Like, Cervidil is $600? That’s insane. This isn’t a guide - it’s a sales pitch for hospital systems. 🙄